Subendocardial myocardial infarction is understood as necrosis of the heart muscle, accompanied by severe pressure on certain areas of the myocardium. The disease leads to disturbances in the rhythm of the heart and its blood supply, and the development of heart failure. This type of heart attack is characterized by a large area of damage. The attack develops rapidly.
Description of the disease
An attack is characterized by significant pressure on certain areas of the myocardium.
This is accompanied by disturbances in heart rhythm, deterioration in the supply of blood to the heart and other internal organs. The area of the affected area in subendocardial infarction is very large. Inflammation develops at an accelerated pace and leads to serious disorders.
This type of heart attack occurs frequently. Subendocardial attacks occur in 50% of all cases, but doctors are trying to reduce the incidence among different segments of the population with the help of:
- unscheduled examination of people at risk to determine pathology at the initial stages of development;
- the use of new treatment methods to get rid of the disease in a short time;
- public awareness of the dangers of cardiovascular system abnormalities.
Small focal subendocardial MI
Subendocardial MI - the QRS complex remains virtually unchanged, since with this type of infarction the magnitude of the myocardial excitation vector does not change (cardiac excitation begins from the ventricular conduction system, which is located under the endocardium and spreads towards the intact endocardium). For this reason, the first and second ECG signs for subendocardial MI are absent.
When cardiomyocytes die in the endocardial zone, potassium ions spread under the endocardium, thus forming minor damage currents, the vector of which is directed outward. Since the strength of such currents is very small, they can only be recorded by an electrode located directly above the infarction zone, which is reflected on the ECG by a horizontal displacement of the ST segment below the isoelectric line by more than 0.2 mV - this is the main sign of subendocardial MI (displacement of the ST segment by an amount less than 0.2 mV indicates ischemia, but not infarction).
It should be said that in practice it is not possible to correlate ECG changes in subendocardial MI with the magnitude of true damage to the heart muscle. In most cases, we can speak of a severe, complicated MI, with suspicion of latent major myocardial necrosis (according to statistics, 40% of subendocardial MI become transmural).
Staging of ECG changes in subendocardial MI
Acute period:
- the first hours of subendocardial MI are characterized by an increase in the T wave, which becomes equal to or higher than the R wave, isosceles or hairpin-shaped;
- by the end of 2-4 hours, depression of the ST segment is observed, and the T wave becomes biphasic;
- in the period of 12-24 hours, the depression of the ST segment increases even more, the T wave merges in one arc with the ST segment, becoming completely negative.
Subacute period and scarring phase:
- the subacute period begins at the end of the 2nd week, when the ST segment gradually approaches the isoline, while the T wave remains negative;
- the beginning of the scarring phase is characterized by a period when the ST segment becomes isoelectric;
- further transformation of the T wave, when it becomes isoelectric or positive, lasts for months.
Provoking factors
The likelihood of developing a pathological process increases under the influence of modified and unmodified factors. The first group is acquired, and a person can completely reduce the risks. Unmodified factors do not depend on the person himself, and he is not able to influence them. These reasons include:
- Bad heredity. Pathologies of the cardiovascular system are often transmitted from parents to children. These are usually chronic diseases that have no cure. These include subendocardial infarction.
- Age-related changes. This form of the disease occurs after 50 years, but cases of an acute attack are also known in young people.
- Floor. The problem is more common in men. But after 70 years, the chances of developing pathology become the same for both sexes.
Modified factors include:
- poor nutrition. Abuse of animal products, salt and lack of the required amount of vitamins, minerals and fiber in the diet lead to the development of heart pathologies;
- increased or decreased blood pressure;
- high blood cholesterol levels. This leads to the appearance of deposits on the walls of blood vessels, narrowing their lumen and disrupting the blood circulation process;
- abnormal level of physical activity. A sedentary lifestyle is just as harmful as excessive exercise. It is useful to do gymnastics daily. But grueling training should be abandoned;
- excess body weight. Obesity leads to the development of various pathologies, including heart attack;
- drinking alcohol in large quantities and smoking;
- metabolic disorders caused by diabetes mellitus;
- stress, emotional stress. Statistics show that seizures are more common in overly excitable people.
Patients at risk are advised to completely eliminate the influence of these factors on the body and undergo a complete examination of the body every six months.
Main causes and symptoms of the disease
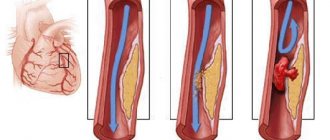
Subendocardial myocardial infarction is a disease the essence of which is necrosis of the inner wall of the heart as a result of various causes. The most common of these is atherosclerosis of the coronary arteries of the heart.
In most cases, atherosclerotic damage is accompanied by the presence of a blood clot, which completely or partially blocks the lumen of the vessel, as a result of which the blood circulation of one or another part of the heart is severely impaired.
- presence of diabetes mellitus;
- arterial hypertension;
- frequent stress;
- presence of mental disorders;
- angina pectoris;
- excess weight;
- bad habits;
- severe genetic inheritance.
Scientists have also proven that poor environmental conditions and prolonged contact with harmful chemicals can also provoke acute subendocardial myocardial infarction in humans.
After suffering a heart attack, the appearance of the first symptoms can be observed within a few minutes. First, you may notice pain behind the sternum, which tends to radiate to the left arm and neck. In the presence of ischemia, shortness of breath and angina can also be observed.
The following can also be observed after a heart attack:
- periodic nausea and vomiting;
- cachexia;
- increased heart rate;
- cold sweating;
- frequent headaches and loss of consciousness.
However, about a quarter of attacks are completely asymptomatic, which poses a great danger in the future, because for some time the consequences will also develop without the presence of obvious symptoms. This is due to the fact that in some people the heart is poorly innervated, so pain and some other signs may not be felt.
Any symptom that is associated with an acute violation of the blood supply to the myocardium can be called acute coronary syndrome.
You should be very careful about your health and if you notice any symptoms, immediately consult a doctor, because any slowness in this case can lead to death.
Prodromal period
Its duration ranges from 2–3 weeks to several months. This phase may not exist, and the acute stage will immediately begin.
Symptoms of the pathology appear slowly. Patients primarily feel pain in the left chest area. Pain appears under the influence of physical activity or in a calm state. To eliminate discomfort, drugs from the nitrate group are prescribed.
If you start treatment at this stage, you can avoid serious health consequences. The disease can be eliminated quickly and forever.
ECG and other diagnostic methods
Since the focus is located under the inner lining of the heart, the Q wave is not formed, and the following signs can be found in the chest leads, the first standard and from the left hand:
- the decrease in ST is dome-shaped, with its apex facing downwards;
- change of T direction or two-phase configuration;
- reduced amplitude R.
Changes in cardiac-specific enzymes have a dynamic appearance and disappearance:
- the first hours myoglobin is increased, peak – 6 – 10 hours, normalization by the end of the day;
- from 3 hours to 6 hours, CPK-MB and troponin increase, reaching a maximum at 20 hours, creatine phosphokinase decreases on days 2 - 3, troponin - on days 7 - 12.
If the increase does not reach 50 - 100 percent, and there is no decrease at the appropriate time, then the diagnosis of myocardial infarction may be questionable. Coronary angiography is performed to determine the patency of the coronary arteries, usually before choosing a surgical method of revascularization.
The most acute period
This phase is short-lived and lasts from several minutes to half an hour. It is during this period that most deaths occur. But if drug treatment is carried out in time, the situation can be improved. Medicines break up blood clots and prevent complications. But only if used in a timely manner.
Also read: Typical clinical form of myocardial infarction
The patient at this stage suffers from:
- severe pain in the chest. The pain syndrome lasts constantly or comes in periods;
- increased sweating;
- weakness and dizziness;
- loss of consciousness;
- constant feelings of anxiety and panic;
- insomnia.
What are subendocardial ischemia and infarction?
Ischemia is the process of bleeding of a certain area of the heart, which occurs either due to stenosis of the supply artery, or due to its blockage by a blood clot / atherosclerotic plaques.
With a long course of this pathology, the patient experiences a heart attack and further necrosis of the heart muscles (a certain part of it). It is important to understand that in the case of ischemia (impaired nutrition of the heart) bioelectric processes are suspended in the cells of the myocardium (the main muscle of the heart). At this point, the patient has a potassium deficiency.
It is worth noting that ischemia itself cannot last long. At one point, either metabolic processes will overcome the pathology and the work of the heart will be restored, or the pathology will take an irreversible turn in the form of myocardial infarction.
Important: the endocardium more often suffers from ischemia than the epicardium, due to the fact that the endocardial cells experience quite a lot of pressure from the blood in both ventricles of the heart. In addition, the endocardial blood supply is already significantly lower than the epicardial supply.
Subacute period
During this period, there is no severe discomfort and pain in the heart. The patient feels much better, so he begins to think that he has fully recovered.
But at the subacute stage, the activity of the affected area of the myocardium decreases. This is accompanied by symptoms such as:
- shortness of breath;
- the appearance of edema of the lower extremities;
- intolerance to any physical activity, even minor and short-term ones. The body eliminates the resulting defect by replacing destroyed cardiomyocytes with connective tissue.
How subendocardial necrosis manifests itself on the ECG
Excitation of the myocardium occurs incorrectly. The subendocardial areas of the heart muscle react first, and only then the subepicardial zone is excited. There is no pathological Q wave in this case. Other changes in the electrocardiogram are associated with deformation of the subendocardial zone and the appearance of areas of necrosis in it.
The development of myocardial infarction is promoted by diabetes mellitus, hypertension, obesity, neuropsychic stress, addiction to alcohol, smoking
Characteristic signs can be easily seen on an ECG:
- reduction and reduction of the ST segment with the arch facing downwards;
- biphasic T wave, which can be either negative or positive;
- the R wave decreases.
Sometimes subepicardial myocardial infarction can have signs similar to necrosis of the posterior wall of the heart muscle, so it is very important for the cardiologist to learn to distinguish between them.
Scarring period
The development of the subendocardial myocardium ends with the scarring stage. What the consequences will be and the patient’s condition depends on the size of the affected area. At this time, a full-fledged scar is formed from coarse fibrous connective tissue.
A person’s well-being improves during this period, the level of pressure in the arteries and body temperature normalize, and all painful sensations disappear. Symptoms of angina pectoris may occur periodically.
If the course of the heart attack was observed by doctors and the correct treatment was prescribed, then the scarring stage passes successfully and the patient can return to their usual lifestyle, but with restrictions.
How it manifests itself
The clinical picture of a heart attack depends on the stage of the attack:
- Prodromal period. At this stage, signs of angina pectoris appear: pain in the left side of the chest. They occur after physical activity. Pain is relieved with nitroglycerin.
- Acute stage. During this period, intense chest pain appears. Nitroglycerin and other drugs of similar action are ineffective. The patient experiences severe fear: he becomes agitated and restless. The first signs of heart failure appear: swelling of the legs, coldness of the upper and lower extremities, pallor of the skin.
- The most acute period. At this stage, the patient's condition deteriorates sharply. A cutting pain in the chest appears, which has an increasing character. The pain syndrome is accompanied by increased sweating, muscle weakness, impaired consciousness, panic attacks, and night insomnia.
- Subacute stage. The intensity of pain decreases. The patient's condition returns to normal, which is mistakenly taken for recovery. The activity of the affected areas of the heart muscle becomes low. Because of this, shortness of breath, severe swelling of the legs, and exercise intolerance appear.
- Scarring phase. At this stage, the process of replacing dead muscle tissue with connective tissue is completed. The clinical picture of this stage depends on the area of the lesion. The patient's condition has stabilized. Blood pressure and body temperature reach normal values. Painful sensations become mild. Attacks of angina pectoris and asphyxia may occur. The patient complains of pressing pain in the chest, lack of air, and attacks of cardiac asthma (suffocation).
Diagnosis and treatment
With such a heart attack, the focus of necrosis is located in the form of a strip near the endocardium of the left ventricle. The diagnosis is made by cardiogram.
Subendocardial myocardial infarction on the ECG must be distinguished from changes in infarction of the posterior wall of the heart muscle. During the study, the condition of the heart, the location of blood clots and the size of the affected area are determined.
Using electrocardiography, you can obtain accurate information about the patient's health status. The procedure is carried out every month to track the dynamics of the disease and monitor the state of health.
Acute subendocardial myocardial infarction is also diagnosed by studying cardiac-specific markers.
They provide information about the death of cardiomyocytes. After laboratory and instrumental examinations, differential diagnosis is carried out with angina pectoris, cardiomyopathies, pericarditis, and aortic aneurysm.
It is important to carry out proper treatment for such a problem. In most cases, endocardial infarction is treated with drug therapy. The patient's condition is normalized with the help of:
- Aspirin. It is prescribed only if there are no contraindications.
- Clopidogrel. The dosage of the medicine depends on the age of the patient. Older people are allowed small doses.
- Anticoagulants. These medications thin the blood and prevent the formation of blood clots. With their help, they achieve a reduction in blood clotting.
- Beta blockers. They normalize the level of pressure in the arteries and reduce the heart rate.
A serious circulatory disorder that occurs during a heart attack negatively affects not only the heart muscle, but also all internal organs. Therefore, there is a need for additional oxygen. It is delivered into the body through special nasal catheters. This process is carefully controlled, since oxygen oversaturation is just as harmful as its deficiency.
Throughout the entire period of treatment, the patient must remain in bed. Any physical and emotional stress is contraindicated for him. These factors negatively affect the course of the disease and lead to a deterioration in the patient’s well-being.
Treatment of subendocardial myocardial infarction
Treatment for suspected myocardial infarction begins at the stage of emergency medical care and continues in the hospital in an intensive care unit or intensive care unit. Use:
- oxygen inhalation;
- nitrates (Isoket, Perlinganite);
- painkillers (Morphine, Droperidol, Fentanyl);
- antiplatelet agents (Aspirin - first dose 300 mg, Clopidogrel, Coplavix, Brilinta);
- anticoagulants (Arixtra, Clexane, Angioks);
- beta blockers for tachycardia and hypertension (Betalok, Egilok).
To restore blood flow in the first hours of a heart attack, thrombolysis (drug dissolution of a blood clot) or balloon expansion of the coronary artery followed by stenting can be performed. Multiple lesions of the coronary vessels are an indication for coronary artery bypass grafting.
Forecast
More than 20% of patients with an acute heart attack die before the treatment process begins. A slightly smaller number die in a medical facility.
The overall mortality rate for patients with subendocardial infarction is 35%. This usually happens in the first two days after the start of treatment.
If blood circulation is restored within 4 hours, the size of the damage will be small, local and general contractility of the left ventricle will improve, and the incidence of hospital complications and the risk of mortality will decrease.
The most favorable prognosis can be achieved if blood circulation is restored within two hours after the onset of the attack.
Late normalization of blood flow also leaves a chance of survival. This is possible when the myocardium heals and the heart rate decreases. But the size of the infarction lesion will be quite large.
Forecast and prevention of the disease
In order for the heart to function fully for many years, it is necessary to take care of it from a young age. Preventive measures are:
- complete cessation of smoking and alcohol;
- moderate physical cardio exercise;
- proper nutrition;
- prolonged exposure to fresh air;
- well-organized work and rest schedule;
- creating a favorable emotional background.
It is worth understanding that it is always easier to prevent any pathology than to reap the benefits of what happened later. So take care of your heart and stay healthy for many years to come.
Myocardial infarction is considered to be a dangerous disease, because it can lead to many unpleasant complications. About half of deaths from heart attacks occur within the first 24 hours after the attack.
This happens in situations where more than half of the heart tissue is damaged, as a result of which it cannot function normally and the person dies. In some cases, even with small foci of necrosis, acute heart failure can develop.
Treatment
Subendocardial myocardial ischemia is treated strictly in a hospital setting. Independent elimination of pathology on the advice of neighbors “who had the same thing” is contraindicated. In general, the therapeutic tactics plan looks like this:
- Drastic limitation of physical activity in the first 5–10 days. Only light exercise in the form of walking and simple gymnastic exercises is allowed.
- Diet therapy with the exclusion of fatty and fried foods. The diet includes dried fruits rich in potassium, plant foods, dairy products, low-fat fish and meat. The entire diet is aimed at correcting body weight and restoring normal metabolic processes.
Against the background of the measures taken, the cardiologist also prescribes drug therapy. Its main goal is to restore blood supply to the heart and strengthen the walls of blood vessels. The following drugs are prescribed:
- Nitrates. In particular, nitroglycerin is indicated for pain relief. For hypotensive patients, nitrates are prescribed very carefully, as they reduce blood pressure.
- Antiplatelet agents and anticoagulants. These drugs thin the blood. In particular, “Aspirin Cardio”, “Thrombo Ass”, “Warfarin”, “Cardiomagnyl”, etc. are prescribed.
- ACE inhibitors. Indicated for relieving spasms in blood vessels and maintaining normal blood pressure. Today they use Enap, Lisinopril or Captopril.
- Beta blockers. Indispensable for ischemia, as they make the heart work more economically. That is, the heart, deprived of sufficient blood supply, works in a lighter mode, without requiring a lot of oxygen. Carvedilol, Metoprolol, etc. are prescribed.
- Fibrates and statins. This group of drugs significantly reduces the concentration of cholesterol fractions. They prescribe Simvastatin, Fenofibrate, etc.
- Diuretics. Indicated for removing excess fluid from the body, which puts significant pressure and stress on the myocardium.
- Antiarrhythmic drugs. Indicated if the patient has arrhythmia.
If drug treatment does not produce the desired effect, the patient is indicated for surgical intervention. One of the most popular surgical methods is balloon angioplasty (stenting) or coronary artery bypass grafting. Both methods are aimed at restoring blood supply in the affected vessels.
Atypical types of disease
Atypical forms of the disease are most often found in elderly patients with various chronic diseases. Especially often against the background of heart failure or a history of heart attack. The following atypical forms of myocardial damage exist:
- Peripheral infarction with atypical location of pain. In such situations, pain may be in the throat, under the shoulder blade, or in the cervicothoracic spine. To diagnose, pay attention to other symptoms: dizziness, weakness, sweating, fear of death, problems with heartbeat.
- Abdominal form. It is a sign of a posterior infarction and is manifested by pain in the epigastrium, in the right hypochondrium or in the entire right half of the abdomen. Symptoms of the pathology are: cold sweat, drop in blood pressure, possible intestinal or stomach bleeding.
- Asthmatic form. The main symptom in such cases is a sudden and severe attack of suffocation. Foamy pink sputum and cold sweat may be produced. Develops with extensive transmural infarctions, as well as with mitral valve insufficiency.
- Collaptoid form. There is no pain, suddenly fainting occurs, darkening of the eyes, and a drop in blood pressure.
- Edema. Sudden onset of shortness of breath, weakness. Feeling of unstable heart function.
- Arrhythmic form. In this case, there is no pain and other signs of a heart attack may be mild. The main symptom is arrhythmia of various types and suddenness.
Diagnosis is carried out in a clinical setting and under the supervision of a specialist. Atypical forms are dangerous because most patients, not suspecting they are having a heart attack, do not seek qualified help.
Classification of myocardial infarction and differences between types
Stages of development and clinical picture of typical forms
The classification of myocardial infarction implies four stages of disease development according to time and clinical picture - damage, acute, subacute, cicatricial.
Damage period (initial)
Symptoms occur within a few hours to 3 days. At this stage, transmural damage to fibers is observed as a result of circulatory disorders. The longer the latent phase, the more serious the disease.
An ECG allows you to recognize the disease. Potassium ions, leaving the dead cells, form damage currents. Then a pathological Q wave appears, which is recorded already on the second day.
If necrotic disorders have appeared in the heart, then the ST segment is much higher than the isoline, the convexity is directed upward, repeating the shape of the monophasic curve. At the same time, the fusion of this segment with a positive T-wave is recorded.
It is noteworthy that if there is no Q wave, then all the cardiac muscle cells are still alive. This tooth may appear even on the 6th day.
The duration of the second stage is from 1 day to 3 weeks.
Gradually, potassium ions are washed out from the damaged area, weakening the strength of the currents. In this case, the damaged area decreases, since some part of the fibers dies, and the surviving part tries to recover and goes into ischemia (local decrease in blood circulation).
The ST segment descends to the isoline, and the negative T wave acquires an expressive contour. However, with infarction of the anterior wall of the left ventricle, ST elevation is likely to persist for some time period.
If a large transmural infarction has occurred, the ST segment rise lasts the longest, indicating a severe clinical picture and poor prognosis.
If in the first stage there was no Q wave, now it appears in the form of QS in the transmural type and QR in the non-transmural type.
The stage lasts about 3 months, sometimes up to a year.
At this stage, deeply damaged fibers move into the necrosis zone, which stabilizes. Other fibers are partially restored and form an ischemic zone. During this period, the doctor determines the size of the lesion. In the future, the ischemic zone is reduced, and the fibers in it continue to recover.
Cicatricial (final)
Scarring of the fibers lasts the entire life of the patient. At the site of necrosis, the tissues of neighboring healthy areas are united. The process is accompanied by compensatory hypertrophy of fibers, the affected areas are reduced, and the transmural type sometimes turns into a non-transmural type.
In the final stage, the cardiogram does not always show the Q wave, so the ECG does not report the disease. There is no zone of damage, the ST segment coincides with the isoline (myocardial infarction occurs without its elevation). Due to the absence of an ischemic zone, the ECG shows a positive T wave, characterized by flattening or less height.
Division by anatomy of the lesion
Based on the anatomy of the lesion, the disease is distinguished:
- transmural;
- intramural;
- subendocardial;
- subepicardial.
Transmural
With a transmural infarction, ischemic damage occurs to the entire muscular layer of the organ. The disease has many symptoms that are common to other diseases. This makes treatment significantly more difficult.
In terms of symptoms, the disease resembles angina pectoris with the difference that in the latter case ischemia is a temporary phenomenon, and with a heart attack it becomes irreversible.
Intramural
The lesion is concentrated in the thickness of the wall of the left ventricle and does not affect the endocardium or epicardium. The size of the lesion may vary.
Subendocardial
This is the name for a heart attack in the form of a narrow strip near the endocardium of the left ventricle. Then the affected area is surrounded by subendocardial damage, as a result of which the ST segment descends below the isoline.
During the normal course of the disease, excitation rapidly passes through the subendocardial sections of the myocardium. Therefore, a pathological Q wave does not have time to appear above the infarction zone. The main sign of the subendocardial form is that the ST segment horizontally shifts above the affected area below the electrical line by more than 0.2 mV.
Subepicardial
The lesion occurs near the epicardium. On the cardiogram, the subepicardial form is expressed in a reduced amplitude of the R wave, a pathological Q wave is visible in the leads above the infarction area, and the ST segment rises above the isoline. A negative T wave appears in the initial stage.
For more details about determining the disease on an ECG, watch the video:
Volume of affected area
There are large-focal, or Q-myocardial infarction, and small-focal, which is also called non-Q-infarction.
Large-focal
Causes large-focal infarction, thrombosis or prolonged spasm of the coronary artery. As a rule, it is transmural.
The following symptoms indicate the development of a Q-infarction:
- pain behind the sternum, radiating to the right upper part of the body, under the left shoulder blade, to the lower jaw, to other parts of the body - shoulder, arm on the right side, epigastric region;
- ineffectiveness of nitroglycerin;
- the duration of pain varies - short-term or more than a day, possibly several attacks;
- weakness;
- depression, fear;
- often - difficulty breathing;
- lower blood pressure in patients with hypertension;
- pale skin, cyanosis (blue color) of mucous membranes;
- profuse sweating;
- sometimes - bradycardia, in some cases turning into tachycardia;
- arrhythmia.
When examining the organ, signs of atherosclerotic cardiosclerosis and expansion of the heart in diameter are revealed. Above the apex and at Botkin's point, the 1st tone is weakened, sometimes split, the 2nd tone dominates, and systolic murmurs are heard. Both heart sounds become muffled. But if necrosis did not develop against the background of pathological changes in the organ, then the 1st tone prevails.
With a large-focal infarction, a pericardial friction noise is heard, the heart rhythm becomes galloping, which indicates a weakened contraction of the heart muscle.
Laboratory studies reveal a high level of leukocytes in the body, an increase in ESR (after 2 days), and a “scissors” effect is observed in the relationship between these two indicators. The large-focal form is accompanied by other biochemical abnormalities, the main one of which is hyperenzymemia, which occurs in the first hours and days.
In case of a large-focal form, hospitalization is indicated. In the acute period, the patient is prescribed bed rest and mental rest. Meals are fractional, limited in calories.
The goal of drug therapy is to prevent and eliminate complications - heart failure, cardiogenic shock, arrhythmias. To relieve pain, narcotic analgesics, antipsychotics and nitroglycerin (intravenously) are used. The patient is prescribed antispasmodics, thrombolytics, antiarrhythmic drugs, ß-blockers, calcium antagonists, magnesia, etc.
Finely focal
With this form, the patient develops small lesions of the heart muscle. The disease is characterized by a milder course compared to large-focal lesions.
The sonority of the tones remains the same, there is no galloping rhythm and pericardial friction noise. The temperature rises to 37.5 degrees, but not higher.
The level of leukocytes is about 10,000–12,000, high ESR is not always detected, and in most cases eosinophilia and band shift do not occur. Enzymes are activated briefly and insignificantly.
On the electrocardiogram, the RS-T segment is displaced, most often falling below the isoline. Pathological changes in the T wave are also observed: as a rule, it becomes negative, symmetrical and takes on a pointed shape.
A small focal infarction is also a reason for hospitalization of the patient. Treatment is carried out using the same means and methods as for the large-focal form.
The prognosis for this form is favorable, mortality is low - 2-4 cases per 100 patients. Aneurysm, cardiac rupture, heart failure, asystole, thromboembolism and other consequences of small-focal myocardial infarction occur rarely, but this focal form of the disease develops into a large-focal form of the disease in 30% of patients.
Localization
Depending on the location, myocardial infarction occurs in the following clinical variants:
- left and right ventricles - blood flow to the left ventricle often stops, and several walls may be affected at once.
- septal, when the interventricular septum suffers;
- apical - necrosis occurs at the apex of the heart;
- basal - damage to the high parts of the posterior wall.
Read also: IBS acute myocardial infarction
Atypical types of disease and their clinical manifestations
In addition to the above, there are other forms of this disease. Atypical forms develop, in particular, in the presence of chronic illnesses. Thus, with osteochondrosis, the main pain syndrome is supplemented by girdle pain in the chest, which intensifies when the back is arched. Atypical forms make diagnosis difficult.
Atypical forms of myocardial infarction include:
- abdominal - in this form, the symptoms resemble acute pancreatitis, pain is localized in the upper abdomen and is accompanied by nausea, bloating, hiccups, and sometimes vomiting;
- asthmatic - this form resembles the acute stage of bronchial asthma, shortness of breath appears, the severity of the symptom increases;
- atypical pain syndrome - a person complains of pain in the lower jaw, iliac fossa, arm, shoulder;
- asymptomatic - this form is rarely observed, and it affects mainly diabetics, who, due to the characteristics of the chronic disease, have reduced sensitivity;
- cerebral - neurological symptoms occur, complaints of dizziness, disturbances of consciousness.
Based on this criterion, the following types of myocardial infarction are distinguished:
- primary - occurs for the first time;
- recurrent - the lesion is recorded within two months after the previous one, and in the same area;
- continued - the same as recurrent, but the affected area is different;
- repeated - diagnosed after two months or later, any area is affected.
Therefore, at the first symptoms that may indicate a heart attack, you should immediately seek medical help.
Prevention
Considering the causes of myocardial infarction, one can easily understand that by following preventive measures, the risk of developing the disease is greatly reduced. For the purpose of prevention, the following rules must be observed:
- Control your body weight. The main goal is to prevent obesity, since this factor is decisive in the formation of atherosclerosis - one of the main causes of myocardial infarction.
- Dieting. Reducing salt intake, as well as reducing the intake of fats from food, can not only reduce the risk of obesity, but also normalize blood pressure.
- Maintaining an active lifestyle. Adequate physical activity helps normalize metabolic processes, reduce body weight, and generally strengthen the body. If you have a history of a heart attack or other cardiovascular pathologies, you should consult your doctor about the amount of exercise.
- Rejection of bad habits.
- Cholesterol control.
- Pressure control.
- Measuring sugar levels.
- Carrying out preventive examinations with a specialist.
Thus, given the etiology of myocardial infarction, we can say with confidence that prevention plays an important role. If you follow the above recommendations, the risk of developing the disease is reduced significantly.
The importance of ECG in the diagnosis of myocardial infarction
- What information is included in the ECG technique?
- What indicates the period and duration of the disease
- How is the location of a heart attack determined?
- Is it possible to find out how extensive the damage area is?
- Diagnosis of the depth of myocardial necrosis
- Difficulties of ECG diagnostics
Electrocardiography (ECG) plays an important role in making the diagnosis of myocardial infarction. The technique is simple and informative. Modern portable devices allow you to take ECGs at home, in a factory health center. And in medical institutions, multi-channel technology has appeared that conducts research in a matter of minutes and helps in decoding.
According to various authors, the signs identified during the examination can be deceptive in 9% of cases.
The nature of the ECG, which reflects the potential difference between healthy and diseased tissue, changes depending on the course of the pathological process in the tissue. Therefore, the results of repeated studies are important.
What information is included in the ECG technique?
100 years ago, a method was developed to record electrical changes in the heart muscle. Electrocardiography is a method that allows you to record the action currents arising in the beating heart. In their absence, the galvanometer needle writes a straight line (isoline), and at different phases of excitation of myocardial cells, characteristic teeth appear with the direction up or down. The processes occurring in the heart tissue are called depolarization and repolarization.