Causes
NVEs develop due to many reasons.
Even a simple sneeze or fear can cause extraordinary contraction of the myocardium. The most common culprits of extrasystoles are various heart diseases: coronary disease, cardiomyopathy, congenital and acquired defects, myocarditis, pericarditis, chronic heart failure, etc. Also, supraventricular extrasystole develops with the following factors, conditions and diseases:
- violation of autonomic regulation (autonomous dysfunction syndrome);
- physical and emotional stress;
- neurotic disorders;
- reflex irritation of the cardiac nerves in diseases of the gastrointestinal tract: duodenal ulcer, cholelithiasis;
- presence of bad habits;
- coffee addiction;
- taking pills: antidepressants, psychostimulants to reduce appetite, vasoconstrictor nasal drops, medications for high blood pressure. Even some antiarrhythmic drugs in some cases cause EVE;
- infectious diseases;
- severe diseases of the respiratory system: bronchial asthma, chronic broncho-obstructive pulmonary disease;
- pathology of endocrine organs: Graves' disease, Hashimoto's thyroiditis, diabetes mellitus;
- excess or deficiency of minerals in the body (calcium, magnesium, sodium);
- chest injuries.
In some cases, the cause of the rhythm disturbance cannot be identified. Then a diagnosis of “NVE of unknown etiology” is made.
Classification and types
There are many types of NLEs, divided according to different characteristics.
Depending on the source of the impulse, atrial extrasystoles and extrasystoles (ES) from the atrioventricular (AV) connection are distinguished. Based on the number, they distinguish between single and double. Three or more ES in a row is already considered an episode of tachycardia (also called a “jog”).
In my patients, I often observe such an ECG phenomenon as allorhythmia - the regular occurrence of extrasystoles. There are the following types:
- bigeminy - the appearance of ES on the cardiogram after each normal contraction of the heart (read more about this phenomenon here)
- trigeminy - after every second complex;
- quadrigeminy - after every third complex.
Depending on the cause, the following types of NVEs are distinguished:
- functional - during physical activity, reflex effects;
- organic - for heart diseases;
- toxic - in case of drug overdose;
- mechanical - for injuries.
Single extrasystoles
The most benign variant of NVE, mainly found in healthy individuals, are single supraventricular extrasystoles. They almost always go unnoticed by humans and do not pose a threat to health.
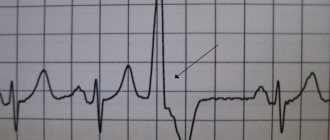
Signs on ECG
Supraventricular extrasystole is very easy to recognize on a cardiogram. Main features:
- extraordinary (extrasystolic) appearance of a pathological deformed P wave and the following unchanged QRST complex;
- the presence of a compensatory pause, i.e. a straight line on the film.
If the P wave has a different shape in different leads, this phenomenon is called polytopic atrial extrasystole. Its detection is highly likely to indicate a heart or lung disease and requires a more thorough diagnosis.
It happens that after an extraordinary P wave there is no QRST complex. This happens when atrial extrasystole is blocked. ES from the atrioventricular junction differs in that the P wave is negative or not recorded at all due to overlap with the T wave.
When taking an ECG at rest, extrasystoles may not be detected. Therefore, in order to “catch” them and find out how often they occur, I prescribe Holter monitoring to my patients. In case of concomitant diseases, a person undergoes a cardiac ultrasound (EchoCG).
After supraventricular ES, the pause lasts less than with ventricular ES.
Symptoms of extrasystole
Often, patients with extrasystole do not feel its symptoms. The signs of this pathology are more pronounced in people suffering from vegetative-vascular dystonia.
With some organic lesions of the heart, extrasystoles can be tolerated even more easily than in the absence of concomitant diseases.
With extrasystole, patients note peculiar tremors, “turnings” of the heart, in other words, sudden interruptions and fading. With functional disorders, general discomfort, weakness, hot flashes, sweating, and lack of air may be observed.
People with atherosclerosis may experience coronary circulatory disorders, dizziness, paresis, and fainting.
Treatment: when, how and with what
Supraventricular extrasystoles are almost always benign. If extraordinary contractions of the heart are single, are not accompanied by any symptoms and do not provoke the occurrence of severe rhythm disturbances, treatment of supraventricular extrasystole is not required. The main thing is to fight its cause.
When EVE worsens the patient's condition, I prescribe drug therapy. The most effective drugs for stopping SE are beta-blockers - Bisoprolol, Metoprolol. If there are contraindications to their use (for example, severe bronchial asthma), I transfer the patient to slow calcium channel blockers - Verapamil, Diltiazem. Read about how extrasystole is treated with medications here.
As for traditional methods, to date there is no convincing evidence of their effectiveness. In my practice, I recommend that patients under no circumstances replace traditional treatment with traditional medicine. But if you have a different opinion, we invite you to read the material here.
If the development of NVE is associated with emotional stress or a neurotic disorder, you can take sedatives and make an appointment with a psychotherapist.
The main criteria for the success of therapy are the cessation of symptoms and normalization of the patient’s condition.
In rare cases, when drug treatment does not have the expected positive effect, surgical intervention is used, in particular, a technique such as radiofrequency catheter ablation. I usually prescribe this operation to young patients, since with age the risk of developing severe complications, including death, increases.
It is extremely rare, for health reasons, that an open access operation is performed, with dissection of the chest and removal of the portion of the myocardium where extraordinary impulses are formed.
Main manifestations
Treatment of symptoms of extrasystole requires an integrated approach to prevent the possibility of relapse of the disease. The disease has characteristic symptoms. It allows you to identify the initial stage of the pathology and prevent further development. The reasons that can cause changes in the condition of heart tissue can vary significantly, but manifestations of such a condition as extrasystole are characteristic. Let's look at them in more detail.
The most common signs of incipient heart tissue damage include the following:
- the appearance of pain in the chest area, especially on the left side;
- noticeable interruptions in the rhythm of heart contractions, which lead to discomfort and pain in the chest. With frequent such manifestations, disturbances in hemodynamics are likely to occur, which becomes a danger to the functioning of the circulatory system;
- frequent noticeable disruptions in the rhythm of heart contraction.
The listed manifestations may be accompanied by an increase in fatigue, regardless of the amount of physical or psychological stress received. There may also be a persistent feeling of lack of air, and the patient may be not only indoors, but also outdoors. The reasons for this are the irregular contractions of certain parts of the heart, the deterioration of the pace and rhythm of this process.
Since it is not easy to remove the manifestations of arrhythmia and tachycardia, the patient’s condition should first be diagnosed in order to identify what causes this pathological condition of the heart. After all, a well-designed treatment regimen allows not only to minimize symptoms and manifestations, but also to completely eliminate them, as well as eliminate the possibility of side effects.
Important! Since the causes of extrasystoles can be varied, for successful treatment it is necessary to take into account the individual characteristics of the patient, his age and susceptibility to the chosen medicinal effect. Extrasystole, the symptoms and treatment of which are interrelated, requires an integrated approach - it is this approach that guarantees tangible results and the possibility of quickly improving the patient’s well-being.
Why are supraventricular extrasystoles dangerous and what are their consequences?
Extraordinary supraventricular extrasystoles themselves do not pose a threat to human life and often go unnoticed. However, they can provoke the appearance of more severe rhythm disturbances: supraventricular tachycardia, atrial fibrillation and flutter, which lead to a sharp decrease in blood pressure, deterioration of blood supply to the myocardium and an increased risk of blood clots in the heart. A combination is often observed .
Long-term polytopic and blocked ES are considered the most unfavorable.
The consequences of supraventricular extrasystole are determined by the presence of: coronary heart disease, chronic heart failure, etc. The rhythm disturbance itself almost does not cause any complications.
Possible complications
Frequent group extrasystoles entail a decrease in cardiac output, and therefore a decrease in blood circulation volume by 8–25% (both cerebral, coronary, and renal). They can also develop into more dangerous forms of arrhythmia:
- atrial leads to atrial flutter;
- ventricular ones cause ventricular paroxysmal tachycardia.
Important: in patients with atrial overload, even single extrasystoles over time can provoke attacks of atrial fibrillation.
It is noteworthy that the systolic rhythm with multiple extraordinary heart impulses can not only accelerate (tachycardia), but also slow down (bradycardia). Heart rate in this situation decreases to 30 times/minute - this is a life-threatening phenomenon, since it is associated with conduction disturbances and a significant risk of myocardial blockade.
The most dangerous type of extrasystole - complicated ventricular - can cause death.
Expert advice
Despite the fact that most often EVEs are relatively harmless, if they occur frequently and are accompanied by symptoms (feelings of freezing, interruptions in heart function, dizziness, feeling of lightheadedness), you should consult a doctor to find out the cause, including examination for cardiac problems. and other diseases. I try to explain to my patients that eliminating the causative factor is of no small importance in the treatment of EVE. Therefore, I give recommendations for lifestyle changes: you need to quit smoking, try to avoid severe stress, and significantly limit the consumption of alcohol and coffee. If a person develops signs of EVE while taking medications, be sure to tell the doctor about it. Reducing the dosage or changing the medication often helps get rid of extrasystoles.
Clinical case
A 33-year-old man came to see me with complaints of rapid heartbeat, periodic sensations of “fading” and interruptions in heart function over the past 3 weeks. He does not take any medications on his own. Doesn't smoke, doesn't drink alcohol. A general examination revealed a high heart rate (105 beats per minute) and increased blood pressure - 140/80 mmHg. Art. During the conversation, I noticed the patient’s uncharacteristic irritability and bulging eyes. When questioning about the presence of diseases in relatives, the man noted that his father suffered from Graves' disease. Holter ECG monitoring was prescribed. Sinus tachycardia, atrial extrasystole of the bigeminy type, and a large number of single extraordinary contractions (967) were detected. A referral was issued to an endocrinologist to check the thyroid gland. On the recommendation of a specialist, an ultrasound examination was performed and blood was taken for hormonal tests. The results obtained: diffuse enlargement of the thyroid gland, decreased TSH levels, increased concentrations of free T4, high titers of antibodies to the TSH receptor. Diffuse toxic goiter was confirmed . Mercazolil therapy was prescribed with subsequent monitoring of hormone levels. To slow down the heartbeat and combat extrasystole, beta-blockers (Bisoprolol) are recommended.
The use of folk remedies
Non-traditional treatment methods are an addition to the main therapy. Advantages of treating extrasystole with folk remedies:
- naturalness of “home medicine”;
- mild effect on the body;
- availability of plant raw materials.
There are many simple and proven recipes that are used for extrasystole. You can normalize the functioning of the heart muscle with the help of decoctions and tinctures based on medicinal plants.
Dry valerian root
The plant restores normal myocardial function, has a positive effect on blood vessels, relieves insomnia, suppresses anxiety, and calms. To treat the disease, an infusion is used: crushed root (4 tsp) pour 1 tbsp. water. The composition is kept in a water bath for 30 minutes. The resulting product is consumed 1 tbsp. up to three times a day.
Important! To suppress attacks, you can use a ready-made tincture of valerian, which is sold in pharmacies.