In Latin there is a word compensatum, which means “to balance.” Compensatory pause is a term that characterizes the diastolic pause that occurs after a heart rhythm disturbance. In terms of time, such a pause is extended. Its duration is equal to two pauses normal for heart rhythm.
A compensatory pause occurs after the ventricular extrasystole and lasts until the next independent contraction.
Reasons for the occurrence of a compensatory pause
After a ventricular extrasystole, a refractory period is observed, characterized by the fact that the ventricle does not respond to the next impulse emanating from the sinus. This leads to the fact that the ventricle contracts not after the first, but after the second sinus impulse. There are cases when the heartbeat is very rare, the end of the refractory period is observed after the extrasystole and before the next sinus impulse. Such changes in heart rhythm can lead to a lack of compensatory pause.
Heart rhythm can be nomotopic or heterotopic. Their simultaneous presence in a person is called parasystole, which can often cause compensatory pauses.
Another reason for their appearance may be extrasystolic allorhythmia, which is a serious pathology associated with impaired circulatory function and heart rhythm.
Extrasystole and compensatory pause? Heart Treatment – MedZabota
Extrasystole is a form of cardiac arrhythmia characterized by premature extraordinary contractions of the heart as a whole or its parts, caused primarily by the re-entry mechanism (re-entry of excitation) or increased oscillatory activity of the cell membranes of various atypical cardiomyocytes that form the conduction system of the heart.
Extrasystole belongs to the category of the most common forms of arrhythmia.
Single episodic extrasystoles can occur even in practically healthy people (there is evidence that extrasystoles occur in 70-80% of people over 50 years of age) under conditions of stress, drug use, abuse of strong coffee, alcoholic beverages, smoking, etc.
Such extrasystole, as a rule: a) is manifested by a feeling of a strong ular (heartbeat) into the chest from the inside, caused by vigorous contraction of the ventricles after a compensatory pause, a feeling of cardiac arrest, anxiety, lack of air; b) is functional in nature (such exgrasystole is sometimes called idiopathic); c) does not require the use of special antiarrhythmic drugs, since it stops on its own after eliminating the factors provoking it.
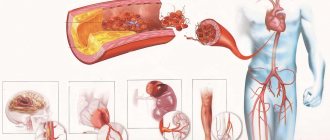
In terms of clinical manifestations and negative consequences, extrasystoles of organic origin are of greatest importance. For a variety of severe heart damage in conditions of the development of hypoxia, dystrophy, myocardial necrosis, as well as cardiosclerosis, etc.
pathogenetically significant electrical heterogeneity is formed in electrically excitable cardiac structures, which determines the occurrence of arrhythmias, including exgrasystole.
The stroke volume of the heart during extrasystole decreases; Moreover, the earlier the extrasystole occurs during the period of diastolic filling, the lower its hemodynamic efficiency.
Therefore, repeated, fairly frequent (more than 6-8 per minute) extrasystoles are characterized by a noticeable decrease in cardiac output, which can lead to a decrease in coronary and cerebral blood flow, i.e., to the development, for example, of angina (especially in patients with coronary artery disease) or fainting, paresis in transient cerebrovascular accidents.
The pathogenetic basis of extrasystole is considered to be the appearance of ectopic foci of increased activity, localized, as a rule, outside the sinus node - in various parts of the conduction system. The extraordinary impulses that arise in this case spread throughout the heart muscle, causing premature contractions of cardiomyocytes in the atria and/or ventricles during the diastole phase.
Based on the localization of ectopic foci of excitation, ventricular (62.6%), atrioventricular (from the atrioventricular junction - 2%), atrial extrasystoles (25%) and various variants of their combination (10.2%) are distinguished. In extremely rare cases, extraordinary impulses come from the physiological pacemaker - the sinoatrial node (0.2% of cases).
There are bigeminy - a rhythm with alternation of normal systole and extrasystole, trigeminy - alternation of two normal systoles with an extrasystole, quadrigeminy - the following extrasystole after every third normal contraction. Regularly recurring bigeminy, trigeminy and quadrigeminy are called allorhythmia.
Group (or volley - more than two per minute) extrasystoles can transform into more dangerous rhythm disturbances: atrial flutter, paroxysmal tachycardia, and, among other things, ventricular fibrillation, which increases the risk of sudden death.
According to the number of ectopic foci of excitation, extrasystoles can be either monotopic (with one foci) or polytopic (with several foci of excitation).
The development of extrasystole is caused by a violation of the ratio of sodium, potassium, magnesium and calcium ions in myocardial cells, which negatively affects the conduction system of the heart.
Some general concepts and terms that are used to describe extrasystoles:
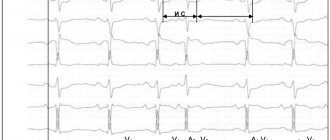
Coupling interval is the distance from the next P-QRST cycle of the main rhythm preceding the extrasystole to the extrasystole.
With atrial extrasystole, the coupling interval is measured from the beginning of the P wave of the cycle preceding the exgrasystole to the beginning of the P wave of the extrasystole; with ventricular extrasystole and from the AV junction - from the beginning of the QRS complex preceding the extrasystole to the beginning of the QRS complex of the extrasystole.
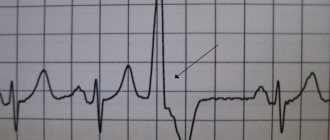
Early extrasystoles
This is the name for extrasystoles, the initial part of which is layered on the T wave of the P-QRST cycle preceding the exgrasystole of the main rhythm cycle, or is spaced from the end of this T wave by no more than 0.04 s. The identification of early exgrasystoles has important prognostic significance due to their low hemodynamic efficiency.
Compensatory pause
This is the name given to the distance from the exgrasystole to the following P-QRST cycle of the main (for example, sinus) rhythm. A compensatory pause is one of the diagnostic criteria for exgrasystoles, which reflects the preparation time for the next sinus impulse, i.e.
the process of depolarization that determines the development of the cardiac cycle, similar to the one that preceded the extrasystole. During the compensatory pause, cardiomyocytes are in a state of refractory. There are incomplete and complete compensatory pauses.
An incomplete pause is slightly longer than the normal R-R interval (RR); characteristic of atrial and nodal extrasystoles. It includes the time required to reach the ectopic signal of the sinus node, “discharge” it and prepare the next sinus impulse.
A complete compensatory pause is equal to twice the interval
Atrial (supraventricular) extrasystole
Electrocardiographic signs:
Atrial extrasystole:
1. premature appearance of the cardiac cycle (PQR5T complex);
2. deformation or change in the polarity of the P wave of the extrasystole; deformation occurs when the ectopic focus is localized in the middle parts of the atria;
3. the shape of the QRS complex of the extrasystole (its width is no more than 0.10 s) is similar to the sinus QRS complex;
4. the presence of an incomplete compensatory pause, which, as a rule, is longer than the RR interval.
Atrioventricular (nodal) extrasystole
Electrocardiographic signs:
Atrioventricular extrasystole:
1. premature appearance of the QRS complex (width no more than 0.10 s), similar in shape to the sinus complex;
2. the P wave is negative before the QRS complex, after the QRS it is absent or negative; the negativity of the P wave is associated with the retrograde spread of excitation to the atria from the nodal extrasystole, the absence of the P wave is due to its overlap with the QRS complex;
3. the presence of an incomplete compensatory pause
Right ventricular extrasystole:
1. premature appearance of an extended (more than 0.10 s) and deformed QRS complex;
2. discordance of the ST interval and T wave relative to the QRS;
3. absence of a P wave before the extrasystole;
4. the presence of a complete compensatory pause.
Characteristic ECG manifestations of extrasystoles
Characteristic ECG manifestations of extrasystoles are:
a) premature appearance of the P wave or QRST complex is a sign of shortening of the pre-extrasystolic coupling interval: with atrial extrasystoles, the distance between the P wave of the main rhythm and the P wave of the exgrasystole, with ventricular and nodal extrasystoles - between the QRS complexes of the main rhythm and the QRS extrasystoles;
b) pronounced deformation, expansion and high amplitude of the extrasystolic QRS complex during ventricular extrasystole;
c) absence of the P wave before the ventricular extrasystole;
d) complete compensatory pause after ventricular extrasystole.
Source: https://medzabot.ru/ekstrasistola-i-kompensatornaya-pauza-lechenie-serdcza.html
Types of compensatory pauses
There are two types of compensatory pauses:
- Full.
- Incomplete.
A complete compensatory pause after ventricular extrasystoles appears as a consequence of the fact that the passage of an extraordinary impulse through the atrioventricular node is not observed. The charge of the sinus node is not destroyed.
The next sinus impulse reaches the ventricles at the time when an extraordinary contraction occurs in them. This period is called the refractory period. The ventricles respond only to the next sinus impulse, which is equal in time to two cardiac cycles.
This means that the time indicating the intervals before and after the extrasystoles is equal to two normal intervals R - R.
An incomplete compensatory pause is characterized by the appearance of excitation in the ectopic focus. The impulse reaches the retrograde sinus node, after which the charge formed in it is destroyed. At this moment, another normal sinus impulse is formed. This means that the interval that appears after the extrasystole is equal to one normal R-R interval and the time during which the extrasystolic impulse travels from the ectopic focus to the sinus node. That is, this situation suggests that the distance from the sinus node to the ectopic focus affects the pause after the extrasystole.
The location of the ectopic focus and the atrioventricular node affects the interval of atrial extrasystole P – Q. The location of the node near the focus significantly shortens P – Q.
What is extrasystole
Extrasystole is one of the variants of heart rhythm disturbance (arrhythmia), in which premature contraction of the entire heart or one of its parts occurs. The patient feels it as a feeling of freezing, a jolt in the chest. Frequent extrasystole may be accompanied by lack of air, pain in the heart, fainting, etc.
Causes of extraordinary heart contractions
- Functional extrasystole. It occurs as a consequence of a vegetative reaction in response to stress, smoking, alcohol, caffeine in practically healthy people. Such cases occur occasionally in 10-15% of people aged 20-30 years and are registered in 80-90% of people over 50 years of age.
- Extrasystole of organic origin. Occurs as a result of direct damage to the heart muscle due to necrosis, cardiosclerosis (replacement of connective muscle tissue) with chronic ischemic heart disease, after acute myocardial infarction, myocarditis or cardiomyopathy, with congenital and acquired heart defects, mitral valve prolapse and various minor anomalies of the heart muscle, endocrine disorders (for example, thyrotoxicosis, thyroiditis, diabetes mellitus),
- Often, extrasystole develops during heavy physical exertion (in manual workers, professional athletes participating in competitions at the limit of their capabilities) due to developing myocardial dystrophy. Physical overexertion provokes the appearance of extrasystole in people with organic diseases of the cardiovascular system. But with functional arrhythmias that have developed against the background of acute or chronic stress, uniform moderate physical activity of an aerobic nature, on the contrary, can suppress extrasystole.
- Toxic extrasystole occurs against the background of prolonged fever, with poisoning with cardiac glycosides, after taking certain stimulants of the central nervous system, antispasmodics, hormonal agents and even antiarrhythmic drugs (the so-called “proarrhythmic side effect”).
Mechanism of formation of extrasystoles
Extrasystole occurs due to the appearance of foci with increased activity, which form outside the sinus node (in the atria, AV node, ventricles) and cause the development and spread of extraordinary impulses throughout the heart muscle.
For extrasystoles to occur, two simultaneous processes are necessary. Firstly, this is the re-entry of an excitation wave in areas of the myocardium or the conduction system of the heart (re-entry wave).
This requires the presence of two conductive paths with different speeds of impulse conduction and, accordingly, with different periods of “rest” (refractory period). First, a normal impulse is generated, which propagates along two paths.
Then an extraordinary ectopic impulse arises, which follows the same paths, but since the conductors need at least minimal rest (and one of them has a longer rest period), this impulse goes along the path with a shorter refractory period, and first, a blockade occurs.
That is, the essence of this mechanism is that there is some kind of additional impulse, and it goes around in a circle, spreading into the surrounding tissues, causing their excitation. And as long as this focus exists, it will generate impulses instead of the sinus node.
Secondly, in addition to the pathological impulse and blockades, for the occurrence of extrasystole, increased activity of the cell membranes of individual sections of the atrioventricular junction (sinus node), atria or ventricles is necessary.
Classification of extrasystole
- Atrial extrasystoles: premature contractions of the entire heart, the impulse of which comes from the atria.
- Extrasystoles from the atrioventricular junction: an electrical impulse originating in the atrioventricular node and propagating in two directions: up to the atria and down to the ventricles.
- Ventricular extrasystoles are the most common variant of extraordinary cardiac contraction (60-70% of cases).
Based on the number of alternations of normal and extraordinary contractions, they distinguish between bigeminy (after each normal cardiac contraction an extraordinary impulse occurs), trigeminy (an extrasystole follows after two normal heart contractions) and quadrigymeny (an interruption after three normal impulses).
In addition, there are paired (2 in a row), group (3 or more in a row) ecustrasystoles, monotopic (one pathological focus of activity) and polytopic (several ectopic foci). Based on the number of observed interruptions per minute, rare (less than 5), medium (6-15) and frequent (more than 15 per minute) extrasystoles are distinguished.
Symptoms (signs)
A single extrasystole may very often go unnoticed and not cause any subjective sensations.
With multiple extrasystoles, patients complain of interruptions in the work of the heart, describing it as a feeling of “turning over, freezing, stopping the heart in the chest.”
Functional extrasystole is accompanied by a feeling of heat, a rush of blood to the face, redness, sweating, discomfort and a feeling of anxiety.
Frequent, group and early extrasystoles cause disruption of the blood supply to the heart muscle, brain and other organs, which can be accompanied by attacks of dizziness, fainting, the appearance and intensification of pain in the heart, neurological disorders (paresis, paralysis, speech impairment).
Diagnosis of extrasystole
Correct assessment of extrasystole is possible only on the basis of a comprehensive examination, including analysis of the patient’s complaints and medical history, objective examination data (pulse in the peripheral arteries and auscultation of the heart), instrumental examination and functional tests (ECG, treadmill test and VEM, Holter monitoring, ultrasound of the heart , transesophageal ECG, etc.). Until now, electrocardiographic examination is the main method for detecting arrhythmias in general and extrasystoles including.
To establish an accurate diagnosis, the following ECG criteria must be present:
Atrial extrasystoles:
- Premature appearance of an altered or unchanged P wave and the following QRS complex
- Change in polarity (depending on which lead, it can be either positive or negative) or shape of the extrasystolic P wave (two-humped)
- Presence of unchanged extrasystolic QRST complex
- The presence of a complete or incomplete compensatory pause
- Shortening of the RR interval before extrasystole.
Extrasystole from the atrioventricular junction:
- Premature, extraordinary appearance of an unchanged QRS complex
- Negative P wave
- Incomplete compensatory pause
- Shortening the PQ interval.
Ventricular extrasystole:
- The appearance of a modified (deformed and widened) extraordinary QRS complex. Is the most important diagnostic criterion
- The location of the T wave and ST segment is opposite to the direction of the main wave of the ventricular complex
- There is no P wave before the extrasystole
- Full compensatory pause.
Treatment of extrasystole
In the presence of rare extrasystole of a functional nature and the absence of any complaints about the state of health, drug treatment is not indicated.
The occurrence of interruptions in the functioning of the heart due to neuropsychic factors (acute or chronic stressful situations) requires normalization of the work and rest regime.
A good effect in this case is achieved by the inclusion of moderate aerobic physical activity (walking, jogging, breathing exercises), taking into account the level of fitness and with constant monitoring of the frequency and uniformity of the pulse before, during and after exercise.
Herbal sedatives based on valerian, motherwort, peony, lemon balm, hawthorn, St. John's wort, psychotherapeutic effects, including neuromuscular relaxation, autogenic training are used in the treatment of functional extrasystole. Proper nutrition is of great importance by including in the diet foods rich in potassium and magnesium (dried apricots, prunes, jacket potatoes), as well as selenium (buckwheat porridge, sea fish, lentils and peas, olives, walnuts).
If extrasystoles occur against the background of some disease (hypertension, ischemic heart disease, myocarditis, heart defects, thyrotoxicosis), then first of all, therapy for the underlying disease is required, and if there is no effect, symptomatic treatment of the extrasystoles. In this case, at first you can use sedatives, tranquilizers and antidepressants, potassium and magnesium preparations, various metabolic and vegetotropic agents.
With frequent (more than 5 per minute and more than 200 per day), group extrasystoles, it is necessary to prescribe antiarrhythmic drugs. For ventricular extrasystoles, amiodarone (cordarone), rhythmonorm, atenolol, concor are more often used; for supraventricular extrasystoles - isoptin, sotalol, etc.
The selection of a specific drug and their combination, dosage and frequency of administration is carried out individually by the attending physician under the control of ECG and Holter monitoring.
In any case, antiarrhythmic drugs should not be taken continuously, but only during the period of deterioration of the condition, followed by a gradual reduction in dosage until complete withdrawal.
If drug treatment in maximum therapeutic doses and drugs of different classes is ineffective, surgical intervention is prescribed.
Currently, minimally invasive surgical interventions, such as catheter radiofrequency ablation, are increasingly being performed.
In this case, a catheter with an electrode that generates special high-frequency pulses is brought through one of the peripheral vessels to the source of extrasystole in the heart. Then a radiofrequency pulse is applied, and the pathological focus is cauterized and destroyed.
Sometimes, with frequent and life-threatening extrasystole, cardioversion (defibrillation) can be used, which in some cases makes it possible to restore the disturbed rhythm. If all of the above treatment methods are ineffective, an electrocardiostimulator may be installed.
With timely detection of extrasystole and correctly selected treatment tactics, in most cases it is possible to achieve a significant improvement in well-being, restore performance and maintain an active lifestyle for a long time.
Source: https://medblog.by/zabolevaniya/chto-takoe-ekstrasistoliya/
How does such a phenomenon threaten human health?
A compensatory pause is a cause for concern, and its occurrence always negatively affects the pumping function of the heart. This condition can appear after emotional excitement, drinking a lot of coffee, nicotine abuse, or sleep disturbances.
Of particular danger are compensatory pauses resulting from signals in the area of ischemic and infarct zones. Such cases, judging by statistical data, often lead to the development of spontaneous ventricular fibrillation, which, in turn, ends in the death of the patient.
A compensatory pause may be evidence of serious illnesses:
- heart defect,
- myocarditis,
- ischemic disease,
- myocardial infarction,
- arterial hypertension,
- chronic heart failure.
Treatment
In order to get rid of compensatory pauses, it is important to cure the underlying disease that provoked them. For this purpose, beta-blockers, sedatives and tranquilizers are used, with the help of which extrasystoles are reduced. Drugs based on quinidine cope well with arrhythmia.
In addition, sometimes it is necessary to seek the help of a psychotherapist.