Symptoms
It is important to know that in some rare cases, this pathology of the limbs can occur without pronounced symptoms.
The most common symptom of this disease is considered to be intermittent claudication. This symptom is expressed by discomfort or pain in the lower extremities that occurs when walking and disappears when it suddenly stops. Sometimes the patient may not feel severe pain, but at the same time, he may be very bothered by cramps, a feeling of heaviness or severe weakness in the lower extremities. Intermittent claudication is more pronounced when climbing upward. As the disease progresses, intermittent claudication may occur even as the distance decreases.
A critical degree of ischemia of the lower extremities can occur with severe disturbances of the blood supply to the tissues of the lower extremities. As a result of this, the tissues do not receive enough oxygen and nutrients, so sharp pain sensations with pronounced intensity may occur, their localization is noted from the top of the thigh to the very tips of the fingers, even at rest, and intensifies with minimal physical exertion on the patient’s lower extremities.
In the presence of severe ischemia of the upper extremities, the following may be noted:
- dry skin;
- severe decrease in temperature of the extremities;
- paleness;
- the appearance of a pronounced painful trophic ulcer.
In the absence of proper treatment, soft tissue necrosis and gangrene of the upper extremities cannot be avoided.
Diagnostics
In order to diagnose circulatory disorders of the extremities, it is necessary to conduct certain laboratory and instrumental studies. To make a correct diagnosis, the doctor pays considerable attention to the presence of any vascular diseases and the presence of characteristic complaints of the patient. This pathology can be accurately diagnosed using the following laboratory research methods:
- general blood test, blood sugar test;
- coagulograms;
- lipid profiles.
The vascular surgeon resorts to such instrumental methods as:
- MRI of the whole body;
- angiography of the extremities;
- Doppler ultrasound.
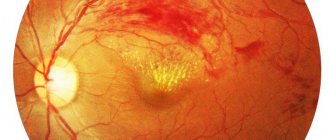
The patient must be examined by an ophthalmologist, who will determine the symptoms of angiopathy and conduct a neuropsychological study in order to identify disorders.
Destruction of the vascular wall
Violation of the integrity of the vessel wall can occur both in pathological conditions of the whole organism (acidosis, hypoxia), and in direct damage to the vessel wall by biologically active agents. The role of such agents is inflammatory mediators in vasculitis (inflammation of the vascular wall).
If the damage progresses, there is leakage (diapedesis) of red blood cells from the blood into surrounding tissues and the formation of hemorrhages.
Clinical picture and symptoms of circulatory disorders
The clinical picture of the disease with different types of its manifestation has its own characteristics; let’s consider some of the symptoms of circulatory disorders:
- Hyperemia. Dilatation of the blood vessels of the body with an excessive increase in blood filling. It is manifested by a change in the color of the skin at the site of damage to the vessel as a result of filling with blood, acquiring a pink-red color. The patient feels pulsation and increased temperature in the affected area;
- Bleeding. The release of blood from a vessel, when its walls rupture, can be external or internal, arterial bleeding is pulsating, bright scarlet in color, venous bleeding is dark red, and with capillary bleeding, pinpoint bleeding from small vessels is observed;
- Ischemia. A reduced supply of arterial blood to the vessels is manifested by a feeling of pain in the affected organ due to a lack of oxygen supply and the accumulation of metabolic products;
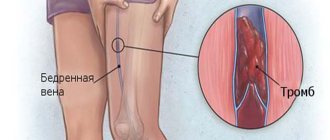
- Thrombosis. A blood coagulation disorder, in which the lumen of the vessel is blocked by a thrombus, there may be complete or partial blockage. The consequence is a slowdown in the outflow of blood from the affected area, with swelling, cyanosis of the skin, and pain;
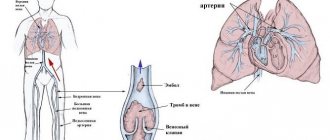
- Embolism. Blocking of the lumen of the vessel with foreign particles such as pieces of adipose tissue, microorganisms, air bubbles. The symptoms are the same as for thrombosis;
- Shock. A clinical condition caused by a decrease in blood supply to tissues due to impaired autoregulation of the microcirculatory system. It manifests itself as destructive changes in internal organs; if blood circulation is disrupted, it can lead to rapid death.
Also often with peripheral damage, the following symptoms of circulatory disorders are observed: pain, tingling, feeling of chilliness and numbness in the extremities, dizziness, tinnitus, memory impairment, weakened vision, sleep disturbance. The symptoms are most pronounced after physical activity, the degree of their manifestation also depends on the severity of the disease.
Intermittent claudication
The most common causes of this condition are atherosclerosis of the arteries of the lower extremities, nonspecific aortoarteritis, thromboangiitis obliterans. Blood flow in the vessels is disrupted due to narrowing of their lumen due to the gradual growth of atherosclerotic plaque or thickening of the walls as a result of a nonspecific inflammatory reaction.
Peripheral circulatory disorders in this case are manifested by the following clinical picture:
- Compensation stage. It is characterized by the appearance of weakness in the legs, cramps and discomfort during physical activity. However, pain appears only when walking a distance of at least 0.5-1 km.
- Subcompensation stage. The patient is forced to stop walking due to pain in the legs after 0.2-0.25 km. The lower extremities undergo some changes due to lack of blood supply: pale, dry, flaky skin, brittle nails, thinned subcutaneous fat layer. The pulsation in the arteries is weakened.
- Stage of decompensation. Walking without pain is possible for a distance of no more than 100 m. Muscle wasting is observed, the skin becomes easily wounded, and numerous cracks and sores appear on its surface.
- Stage of destructive changes. In this situation, blood flow in the vessels almost completely stops. The lower extremities become covered with ulcers, and in especially severe cases, gangrene of the fingers develops. Working capacity is sharply reduced.
Of course, impaired peripheral circulation in this pathology develops over a long period of time. It takes a long time before the stage of gangrene occurs, during which the necessary measures can be taken to prevent a complete cessation of blood flow.
Causes of Blood Flow Problems
The composition of peripheral blood in the microvasculature is diverse, since there is not only arterial, but also venous blood. In a healthy body, blood flows through the arteries into the precapillaries, then into the capillaries, through the walls of which exchange occurs. The blood then ends up in the precapillaries, which lead to the venules, and then into the veins.
If there is a violation of blood microcirculation in peripheral vessels, anastomoses appear. This is the name for shunt vessels, which are responsible for the direct connection between the arterial and venous beds, when capillaries blocked by a thrombus are completely or partially excluded from the bloodstream. If this happens in the brain or around the heart, it can very quickly result in death or disability, requiring constant nursing care, medications and other treatments.
In the event of a violation of microcirculation in the tissues of the legs, arms, and other parts of the body, various symptoms characteristic of cell death will be observed for a long time (which ones largely depend on the affected organ)
Therefore, if a person pays attention to the development of a pathological process in time, he has a chance to stop the development of the disease with the help of medications and other means
It should be noted that the causes of peripheral circulatory disorders are the same as those of central circulation (when large vessels supplying the heart, brain and some other important organs are affected). Microcirculation disorders can be caused by the following situations:
- Blockage of blood vessels due to blood clots, which are formed due to clumped platelets or red blood cells.
- Blockage of blood vessels due to an embolus (the so-called particles that are absent in the blood of a healthy person).
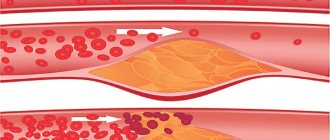
- Atherosclerosis: can cause narrowing of the lumen of blood vessels, their blockage due to detached growth. It causes the formation of blood clots, since cholesterol plaques damage the walls of blood vessels, which leads to microcracks to which platelets, leukocytes, and red blood cells rush.
- Violation of the integrity of the walls of blood vessels.
- High or low blood pressure.
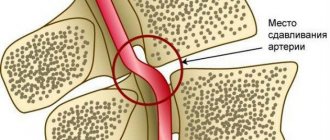
- Compression of the vessel due to the growth and enlargement of the tumor.
- Decreased blood volume (bleeding, dehydration).
- Problems in the functioning of the cardiovascular system.
All these reasons are dangerous for the body. Therefore, regardless of the affected area, you must immediately begin treatment, which is prescribed by a doctor using medications and other means. It should be borne in mind that if the cause of circulatory disorders is the heart, atherosclerosis, changes in blood volume, pathological processes will affect all vessels, both central and peripheral. If a violation of microcirculation causes the clumping of red blood cells, platelets, the appearance of emboli, tumors, pathological processes will develop in the area of origin.
Depletion of peripheral blood flow
Peripheral circulation is blood circulation that occurs within certain organs. Various medical textbooks and other sources use different names for such blood circulation:
- organ;
- fabric;
- local;
- regional.
Thanks to the peripheral blood supply, the necessary volumes of blood and pressure in organs and tissues are provided. In addition, leukocytes contained in the blood actively monitor the condition of organs and the body as a whole, and platelets can quickly solve problems with vascular damage.
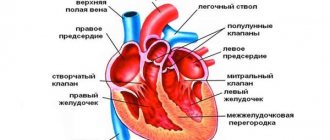
Blood supply occurs thanks to the heart muscle, which pumps the required amount of oxygenated blood from the lungs, and vessels and capillaries carry it to the organs.
Due to the fact that the heart muscle constantly contracts and relaxes, pulsation keeps the blood vessels in good shape. In this way, the required pressure is ensured at a certain moment. Veins carry waste blood away from the organs.
Microcirculation of the peripheral circulation is the link that delivers blood to the organs.
Regional blood circulation occurs in the following vessels, the size of which does not exceed 200 microns:
- Aorta and large arteries. Here, progressive blood flow occurs due to the energy of the stretching walls.
- Small arterioles and arteries. The main function is to determine the resistance value.
- Capillaries. They carry out metabolism between blood and organ tissues.
- Venach. Despite their poor elasticity, they are able to stretch, allowing blood to pass further.
Some concentrated amounts of blood are retained in organ tissues, such as the bone marrow, spleen, or liver. The rest of the blood, ranging from 4 to 6 liters, in percentage terms this is at least 8% of a person’s body weight, is constantly in the process of circulation: from the heart to the organ - through the arteries, from the organ to the heart - through the veins.
When and why do peripheral circulatory disorders occur?
When the system is fully functioning, blood is first transferred through the arteries to the precapillaries, and through the walls of these vessels is transferred to the veins. The exchange process is similar in reverse order.
The most life-threatening condition is blockage of precapillaries by blood clots. If such a process occurs in the heart or brain, then for a person this can cause rapid death or severe disability.
If a similar process begins in the upper or lower extremities, then for a certain period of time it will be accompanied by symptoms of cell death of the affected organ. If you pay attention to the symptoms in time, you can undergo treatment and get rid of peripheral circulatory disorders.
Unfortunately, the causes of violations are situations that a person can avoid if he leads an active lifestyle, eats right and undergoes a medical examination by a doctor on time.
Most often, problems in the peripheral system provoke:
- thrombosis caused by an increased number of platelets or red blood cells;
- thrombosis caused by a high amount of embolus. Such a substance should not be present in the blood of a healthy person;
- rupture of the vessel walls;
- blood pressure surges;
- hypertension;
- hypotension;
- oncological formations that lead to compression of the vessel;
- dehydration;
- internal bleeding;
- disruptions in the functioning of the heart or vascular system.
Each of the listed reasons can lead to death, therefore, at the first suspicion of improper functioning of the peripheral system, you should consult a doctor for diagnosis and choice of treatment regimen.
How is it regulated?
The speed and volume of peripheral blood circulation is regulated by resistance to blood flow: mainly, this is a change in the lumen of blood vessels as a result of contractions of smooth muscles.
Regulation of peripheral blood circulation is carried out thanks to the coordinated work of the nervous system.
When the nerve fibers that carry the signal from the brain to the organs are excited, the smooth muscles of most arteries contract, due to the function of the endocrine glands.
Certain hormones (adrenaline, vasopressin) begin to be produced at double speed, narrowing the vessels of the periphery, but dilating the vessels of the brain and heart.
This includes the amount of reserve oxygen necessary for the normal functioning of these organs. Due to the interconnection of all organs of the body, these hormones promote increased production of histamine, which subsequently dilates the capillaries, and the substance acetylcholine produced by some nerve endings increases the lumen of blood vessels.
Several factors influence normal blood circulation:
- eating;
- exercise stress;
- fatigue;
- physical activity;
- arterial pressure;
- blood viscosity;
- heart function;
- tone, integrity of blood vessels.
For example, with a prolonged lack of nutrients or poor functioning of the heart muscle, microcirculation slows down.
Signs of violations
Since the causes of malfunctions in the peripheral system can be various factors, the clinical picture for each patient will be individual.
Among the most common signs of violations that should alert everyone are the following:
- The appearance of varicose veins, swelling or swelling of the limb.
- Sharp or dull pain that does not stop for a long time.
- Blue tint of the skin.
- Sudden numbness of a limb.
- With slight hypothermia, pain appears in the hands and feet.
- Cold extremities of the hands and feet.
- Headaches, which may be accompanied by tinnitus and dizziness.
- Memory problems.
You should not self-medicate, as damaged blood vessels can, on the contrary, accelerate the process of destruction. In addition, problems with the peripheral vessels of the lower extremities can provoke weakness and cramps in the legs, causing lameness.
If the disease progresses rapidly, the skin, hair and nails begin to react to the lack of nutrients and oxygen. The skin becomes pale, dryness and flaking appear.
Worth remembering! You can suspect problems in the vessels of the peripheral system of the lower extremities by measuring the pulse. It will be weak, barely noticeable.
Problem solving
The therapy program is determined depending on the disease. If you consulted a doctor at the initial signs of pathology, you can get by with conservative treatment methods.
Surgery is necessary when the blockage of arteries and veins cannot be eliminated with medication. Since impaired blood circulation leads to necrosis of limbs or organs, it is necessary to quickly eliminate the cause of this disorder. The operation is reduced to removing the affected areas of the vessels, their reconstruction and replacement.
Filtration is carried out to eliminate and remove blood clots.
In difficult situations, when the blood supply to vital organs is disrupted, phlebologists and pathologists decide to add vessels to the organ.
Medicines
Drug treatment is quite extensive. Depending on the pathology, it is necessary to use several medications at once.
Treatment goals:
- Achieve blood thinning.
- Eliminate narrowing or dilation of blood vessels.
- Normalize blood pressure.
- Eliminate formed blood clots and other substances.
- Improve the elasticity and strength of blood vessels.
- Get rid of vascular spasm.
However, their use should be discussed with a doctor.
A balanced diet: avoiding some foods and taking others can significantly improve the deplorable state of peripheral circulation.
First of all, you need to give up alcohol, carbonated and sweet drinks. Infusions and teas based on lemon balm, mint and chamomile have a beneficial effect on resolving the problem.
If your blood circulation is impaired, you should avoid the following foods:
- fat;
- fried;
- flour;
- sweet;
- yeast;
- smoked;
- salty.
Fish and chicken also contain a lot of useful substances.
Citrus fruits have a beneficial effect on the condition of blood vessels and the heart.
The daily diet should be divided into 5-6 parts and under no circumstances should you overeat.
Other methods
- Physical activity. 15 minutes of charging three times a day is enough, this will help restore blood supply to the organs. Doctors prescribe certain types of exercise therapy.
- Physiotherapy (hirudotherapy, magnetic therapy). Possible at the initial stage of the disorder.
- Phytotherapy. Traditional medicine is relevant, but self-medication is contraindicated.
Treatment Options
The choice of treatment regimen primarily depends on the cause that provoked pathological changes in the peripheral circulatory system.
First of all, an experienced specialist will prescribe a diagnostic test to see what indicators the blood has at the moment.
Using a general blood test, it is possible to determine the number of platelets, hemoglobin, erythrocytes, and leukocytes.
If the doctor diagnoses an acute disorder, then treatment, in most cases, is surgical. The operation allows the patient to completely remove the blocked vessel in order to restore proper blood flow.
There are extreme cases when the vessel cannot be removed, and the doctor recommends removal of the entire organ. Such an outcome is always a person’s disability.
If the pathological changes are not acute and develop slowly, then doctors first carry out drug therapy. All medications are prescribed only by a doctor, but you must remember that alcohol and smoking cause blood vessels to spasm and work incorrectly. When diagnosing pathologies of peripheral circulation, you need to completely get rid of bad habits.
Drug therapy will be aimed at:
- improved blood flow;
- stimulation of blood microcirculation;
- to dilate blood vessels;
- elimination of blood clots.
In some cases, your doctor may order a test of your immune system. If it is this system that causes a malfunction in the periphery, the doctor recommends medications to restore its functioning.
For peripheral circulation disorders in the lower extremities, the specialist recommends medications that can restore the firmness and elasticity of the walls of the venous vessels.
Most often, therapy is complex, which necessarily involves the use of venotonics and lymphotonics, as well as phlebotropic drugs.
Additional techniques help to eliminate the problem with blood vessels perfectly.
When choosing any treatment option, the specialist focuses on the importance of diet. A consultation with a nutritionist is required; a list of foods that are recommended and prohibited for consumption during treatment is compiled. Basically, this list of recommendations will also be necessary as a preventive measure.
Peripheral blood circulation is an important link in the coordinated work of the whole organism. The slightest deviations in the operation of this system will immediately affect the condition of all organs and internal systems. By carefully listening to manifestations that are unusual for the body, you can consult a doctor in the early stages, undergo treatment and return to a full life.
Prevention
In most cases, peripheral circulatory disorders can be prevented or its negative consequences can be significantly reduced.
It is necessary to undergo complete examinations in the clinic in a timely manner, and if there is the slightest deviation from the norm, contact a specialist.
An active lifestyle, quitting smoking and alcohol-containing products can significantly strengthen blood vessels and have a beneficial effect on the overall health of the body.
Conclusion
Peripheral blood circulation is one of the components of a complex system of providing all organs and tissues of the body with oxygen and nutrients.
https://www..com/watch?v=6YsjJ-v_U
The situation can be avoided or corrected; you just need to seek help from a phlebologist and other highly specialized specialists.
Source: https://moeserdce.net.ru/obednenie-perifericheskogo-krovotoka/
Main causes of the disease
Scientists have identified the main risk factors that provoke cerebral circulatory failure:
- genetic inheritance;
- congenital or acquired thin and fragile blood vessels;
- vascular diseases (atherosclerosis, etc.);
- increased blood viscosity;
- disturbances in the functioning of the heart (defects, changes in its rhythm, etc.);
- high blood pressure;
- disorders in the musculoskeletal system;
- diabetes;
- overweight;
- excessive abuse of alcohol and tobacco products;
- taking a certain group of medications (hormonal contraceptives or drugs that change the rheological properties of the blood);
- nervous tension or stress;
- increased physical activity;
- duration of adherence to depleting diets.
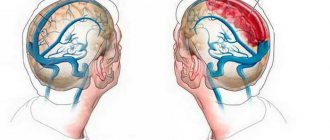
Cerebrovascular accidents occur equally among men and women. However, in older people this pathology is diagnosed much more often. This is due to the emergence of chronic diseases that cause disruption of natural blood circulation. Vascular genesis can provoke:
- Transient disorders;
- Complete or partial blockage of blood vessels;
- Rupture of blood vessels and severe hemorrhage in the brain.
How to improve blood circulation in the head using alternative methods
To strengthen the vascular system and establish smooth blood flow, specialists prescribe an effective course of acupuncture. This treatment is not suitable for all patients, and is most often prescribed in the early stages of the disease. Acupuncture activates the work of all internal processes associated with vascular circulation, normalizes the state of the nervous system and helps strengthen the immune system.
Prevention of diseases of the circulatory system will also include:
- cold and hot shower;
— extreme sports;
— hardening;
- massage
You can start by improving your body’s health today, by accustoming your loved ones, including small children, to a new life. Hardening, walks in the fresh air, proper nutrition are habits that will help you be strong and healthy from early childhood.
Treatment with angioprotectors
The main therapy is carried out in accordance with the clinical manifestations (angina pectoris, encephalopathy, nephropathy or angiopathy of the extremities). To treat microcirculation disorders, a group of drugs called angioprotectors is used. Regardless of the chemical structure, all these medications have common characteristics:
- relieve arterial spasm;
- improve vascular permeability;
- normalize blood fluidity;
- increase the strength of vascular walls;
- reduce tissue swelling;
- accelerate metabolic processes in the walls of capillaries, venules and arterioles.
These include: Troxevasin, Detralex, Etamsylate, Calcium Dobesylate, Trental, Aescusan, Corvitin, Emoxipin, Quercetin, Lysine aescinate and their analogues.
In addition, complex therapy may include drugs that improve blood composition and metabolic processes in tissues:
- antiplatelet agents (Aspirin, Curantil);
- antihypoxants (Actovegin, Neoton, Cytoflavin);
- antioxidants (Mildronate, vitamins E and C).
Microcirculation disorders arise due to the presence of internal or external obstacles to the movement of blood through small vessels, impaired permeability of vascular walls, and blood thickening. Depending on the predominance of damage to internal organs, ischemic processes manifest themselves in the form of angina, heart attack, stroke, kidney disease or vascular disease of the lower extremities. Treatment requires the use of drugs from the group of angioprotectors.
Levels of the circulatory system
Conventionally, all blood supply to organs and systems of the body can be divided into three levels:
- Systemic circulation is formed by large vessels that transport blood throughout the body.
- Organ blood circulation is formed by medium-diameter vessels that provide blood supply to individual organs depending on their need for oxygen. For example, the brain is supplied with blood very abundantly, since it needs a lot of energy, and therefore oxygen.
- Microcirculation - includes the smallest vessels that are in direct contact with cells and tissues.
Blood and vessels
Peripheral blood vessels are small arteries, veins, as well as the microcircular bed, represented by vessels whose diameter does not exceed 200 microns, as well as capillaries. It is in the microcircular bed that the exchange of gases, liquids, nutrients, and waste products occurs between blood and cells. Therefore, the role of blood is very important for the functioning of the entire body, and disruption of blood flow leads to the fact that cells do not receive enough elements necessary for their development. But there is a delay in decay products that poison the tissue.
If we talk about what blood is, then it is worth noting that it is a liquid tissue that consists of plasma, as well as blood cells, most of which are red blood cells. This is due to the fact that they are a kind of trailer containing hemoglobin. This is a complex protein that contains heme, which has the ability to easily attach gases to itself, as well as quickly part with them. It also gives the blood a red color. Thus, thanks to hemoglobin, tissues can receive oxygen and release carbon dioxide to red blood cells.
Leukocytes circulating in the blood are important. They monitor the health of the body, destroying pathogenic organisms that attack it from the outside
White blood cells also produce antibodies to destroy damaged or dying cells in the body.
Platelets are activated at the slightest tissue damage, both outside and inside the body, and rush to the site of damage to eliminate the breakthrough
Therefore, platelets are an important part of the coagulation system
Plasma is the liquid part of blood, most of which is water. It also contains various proteins, amino acids, carbons, fats, lipids and other elements, without which cells would not be able to grow and develop. There are billions of them, and thanks to them, various processes occur in the body.
Plasma moves through large and small vessels. In the arteries there is blood rich in nutrients, in the veins it is saturated with decay products and carbon dioxide given off by cells. She carries them through organs that rid the blood of toxins and cleanse them of carbon dioxide (liver, spleen, kidneys, lungs).
Structural features
The microvasculature has a different structure, depending on the organ in which it is located.
For example, in the kidneys, the capillaries are collected into a glomerulus, which is formed from the afferent artery, and from the glomerulus of capillaries itself the efferent artery is formed. Moreover, the diameter of the incoming one is twice as large as the outgoing one. This structure is necessary for the filtration of blood and the formation of primary urine.
And in the liver there are wide capillaries called sinusoids. Both oxygenated arterial and oxygen-poor venous blood enter these vessels from the portal vein. Special sinusoids are also present in the bone marrow.
Symptoms
General symptoms of the disease include painful attacks, changes in the shade of the fingers, the appearance of ulcers, cyanosis, swelling of blood vessels and the area around them, fatigue, fainting and much more. Every person who has ever encountered such problems has repeatedly complained to the doctor about such manifestations.
If we analyze the disease according to the location of the lesion and its symptoms, then cerebral circulation disorders do not manifest themselves in any way at the first stage. Signs will not bother the patient until there is a strong blood supply to the brain. The patient also begins to exhibit the following symptoms of circulatory disorders:
- pain syndrome;
- impaired coordination and visual function;
- noise in the head;
- decreased level of performance;
- insomnia;
- impairment of the quality of the memory function of the brain;
- numbness of the face and limbs;
- failure in the speech apparatus.
Symptoms of cerebrovascular accident
If there is a circulatory disorder in the legs and arms, then the patient experiences severe lameness with pain, as well as loss of sensitivity. The temperature of the extremities is often slightly reduced. A person may be bothered by a constant feeling of heaviness, weakness and cramps.
What is the danger of the disease
This pathology causes many complications. Vascular diseases occupy one of the leading places in mortality in all countries. Lost tissues and structures in the brain cannot be restored. The consequences of an advanced disease can be:
- Ischemic stroke (cerebral infarction), accompanied by nausea, dizziness, tinnitus, vomiting due to cessation of blood supply to one of the parts of the brain. Speech, motor, emotional and volitional functions suffer and the functioning of internal organs is disrupted.
- Hemorrhagic stroke (hemorrhoidal), is provoked by blood thrown into the brain cavity from ruptured vessels. Pressure increases, the brain contracts, the structures of the foramen magnum are damaged, and blood circulation in the brain is disrupted. In terms of mortality, hemorrhoidal stroke occupies a leading place.
- Transistor ischemic attack, characterized by paralysis of the limbs, drowsiness, damage to motor, visual, and speech functions. Blood circulation is restored with medications that improve brain function.
Problems with peripheral blood flow lead to chronic poor circulation. The patient is diagnosed with intellectual retardation and dulling of mental abilities. The patient becomes irritable, sometimes aggressive, restless, and has absent-mindedness.
Symptoms
Symptoms of circulatory disorders of the lower extremities depend on the type and depth of vascular damage.
Clinical manifestations of venous insufficiency
Symptoms and signs of acute deep venous thrombosis:
- bursting pain;
- persistent swelling of the lower leg or entire limb;
- the skin becomes glossy and a venous pattern appears on it;
- pain is felt on the inside of the limb along the thrombosed vein;
- when dorsiflexing the foot, pain occurs in the shin;
- the diseased limb is colder than the healthy one.
With chronic venous circulation disorders, symptoms increase gradually. At the compensation stage, which can last for years, they are practically absent. An external sign is convoluted, protruding veins. At the next stage, the legs become swollen, begin to tire quickly, bursting pains and night cramps appear in them. At the stage of decompensation, itching, severe swelling of the feet and legs, severe varicose veins, acute pain and trophic changes in the skin (pigmentation, thinning, hair loss) occur. Further, progressive venous insufficiency leads to disruption of tissue trophism and necrosis. As a result, trophic ulcers are formed.
Manifestations of venous insufficiency
Symptoms of arterial insufficiency
Acute and chronic disturbance of blood supply in arterial insufficiency is manifested by general clinical symptoms:
- the temperature of the affected limb decreases;
- the skin acquires a marbled color, becomes pale, and when changing from a horizontal to a vertical position, the pallor is replaced by a crimson color;
- Below the site of arterial blockage, the pulse cannot be felt, but above this site it intensifies;
- a symptom of empty superficial veins appears;
- tactile and pain sensitivity decreases;
- limb function is impaired until complete failure.
Acute arterial occlusion is manifested by additional symptoms. Their severity depends on the caliber of the affected vessel. Patients complain of acute pain below the site of artery blockage, numbness and weakness of the limb. With thromboembolism, the patient’s general condition worsens, an increase in heart rate, cyanosis of the lips and mucous membranes, increased breathing are observed - a state of shock occurs. If the patient is left without medical care, limb ischemia and gangrene rapidly develop.
Chronic arterial obstruction is classified according to the stages of the disease with a specific clinical picture. At the first stage (functional compensation), there is intermittent claudication, pallor and coldness of the skin on the affected leg, a long-lasting white spot after pressing, pain when walking 0.5–1 km.
The stage of subcompensation is manifested by transient symptoms of ischemia - when walking 200–300 m, pain appears, and at rest it disappears. Patients complain of coldness and paleness of the feet. At the third stage, blood circulation is decompensated. It is difficult for the patient to walk even 25 m, hair falls out, the skin dries out, the nails on the affected leg become deformed, and the pulsation in the foot disappears. Foci of necrosis appear on the fingers. The fourth stage is the appearance of ulcers and foci of dry gangrene, the pain becomes intense, the foot swells and turns blue.
Peripheral circulation disorders: thrombosis and embolism
Violation of central and peripheral circulation develops for various reasons. However, the clinical picture of this condition is recognizable and typical in all cases. In surgical practice, this is a fairly common problem, including many pathological conditions that in one way or another affect blood flow.
Causes of circulatory disorders
Various situations can interfere with the normal movement of blood through the vessels:
- The lumen of the vessel is impassable. This is possible if it is blocked (for example, by a blood clot or atherosclerotic plaque) or narrowed (stenosis).
- Pathological changes in the wall (hypertrophy in arterial hypertension).
- Compression of a vessel from the outside (for example, by a tumor).
- Damage to the vascular wall.
- Changes in the rheological properties of blood.
- Decrease in circulating blood volume (during bleeding, dehydration).
- Decreased blood pressure (shock, heart failure).
- Pathology of the heart (defects, heart failure), in which the volume of blood emitted during systole decreases.
All these situations can affect the blood flow of both main and peripheral vessels.
In case of problems with the heart, hemodynamic disorders, changes in the volume of circulating blood, pathology of the clotting mechanisms, blood circulation will be disrupted at all levels - from large vessels to the smallest. Local disorders (stenosis, thrombosis, hypertrophy of vascular walls) are reflected directly in the area where they occurred.
The causes of peripheral circulatory disorders are, in principle, the same as central ones. However, when talking about the pathology of blood flow in the periphery, we primarily mean local disorders of blood circulation.
Peripheral circulatory disorders in surgery are primarily situations associated with local cessation of blood flow: thrombosis, embolism, vessel compression, atherosclerosis. All of these conditions (with the possible exception of atherosclerosis) are emergencies requiring immediate assistance.
Peripheral circulatory disorders: symptoms
What is the manifestation of local cessation of blood flow? Tissues that find themselves without adequate blood supply begin to experience ischemia, because now they do not receive the oxygen necessary for normal functioning. The stronger the nutritional deficiency, the faster cell death occurs. In the absence of the necessary help, gangrene develops (i.e., death of tissues deprived of blood supply).
Violation of the peripheral circulation of the lower extremities is the most striking example. Blood flow disorders in this case can develop suddenly or gradually.
Intermittent claudication
The most common causes of this condition are atherosclerosis of the arteries of the lower extremities, nonspecific aortoarteritis, thromboangiitis obliterans. Blood flow in the vessels is disrupted due to narrowing of their lumen due to the gradual growth of atherosclerotic plaque or thickening of the walls as a result of a nonspecific inflammatory reaction.
Peripheral circulatory disorders in this case are manifested by the following clinical picture:
- Compensation stage. It is characterized by the appearance of weakness in the legs, cramps and discomfort during physical activity. However, pain appears only when walking a distance of at least 0.5-1 km.
- Subcompensation stage. The patient is forced to stop walking due to pain in the legs after 0.2-0.25 km. The lower extremities undergo some changes due to lack of blood supply: pale, dry, flaky skin, brittle nails, thinned subcutaneous fat layer. The pulsation in the arteries is weakened.
- Stage of decompensation. Walking without pain is possible for a distance of no more than 100 m. Muscle wasting is observed, the skin becomes easily wounded, and numerous cracks and sores appear on its surface.
- Stage of destructive changes. In this situation, blood flow in the vessels almost completely stops. The lower extremities become covered with ulcers, and in especially severe cases, gangrene of the fingers develops. Working capacity is sharply reduced.
Of course, impaired peripheral circulation in this pathology develops over a long period of time. It takes a long time before the stage of gangrene occurs, during which the necessary measures can be taken to prevent a complete cessation of blood flow.
Arterial thrombosis and embolism
In this case, acute disturbances of the peripheral arterial circulation occur, which in a matter of hours can lead to the development of gangrene of the limb if timely assistance is not provided.
A thrombus in an artery can form on an atherosclerotic plaque, in the area of inflammation of the vessel wall or its damage.
An embolus is a blood clot brought by a blood stream from another part of the vascular bed.
As a result, the lumen of the vessel is completely blocked, blood flow stops, tissues begin to experience ischemia, and if this situation persists for a long time, they die (gangrene develops).
Clinic of acute peripheral circulatory disorders
The most rapid change in symptoms is observed with embolism, because in this case the cessation of blood flow occurs suddenly, leaving no opportunity for compensatory changes.
The first two hours the patient experiences severe pain in the limb. The latter becomes pale and cold to the touch. There is no pulsation in the distal arteries. Gradually the pain decreases, and along with it the sensitivity is muffled until complete anesthesia.
The motor functions of the limb also suffer, eventually developing paralysis. Very soon, irreversible changes in tissues and their death occur. With thrombosis, the picture is, in principle, the same, but the clinical development is not so rapid. The growth of a blood clot takes a certain time, so the blood flow is not immediately disrupted.
In accordance with Savelyev’s classification, there are 3 degrees of ischemia:
- Characterized by sensitivity disorders.
- Movement disorders are added.
- At this stage, tissue necrosis begins.
Peripheral circulation disorders: treatment
Tactics depend on the severity of ischemia and the rate of development of irreversible changes in tissues. Acute peripheral circulatory disorders require surgical treatment. In case of gradual deterioration of blood flow during the stages of compensation, a good result can be achieved with conservative therapy.
Surgeries for acute blood flow disorders
Conservative treatment in this case is ineffective, because it is not able to completely destroy the blood clot and eliminate the obstruction to blood flow. Its use is possible only in cases of severe concomitant pathology, provided that compensatory reactions are sufficient.
After stabilizing the patient’s condition, an operation is performed to remove the blood clot from the lumen of the vessel. Blood flow is restored as follows. A Fogarty catheter is inserted into the lumen of the affected artery above the blockage, with the help of which the blood clot is removed.
To insert a catheter, surgical access is carried out at the level of the bifurcation of the femoral artery (if the lower limb is affected) or the brachial artery (if the upper limb is affected).
After performing an arteriotomy, the Fogarty catheter is advanced to the site of blockage of the vessel by a thrombus, passed through the obstruction, after which it is inflated and removed in this state. The inflated balloon at the end of the catheter captures and carries the clot along with it.
If thrombosis occurs in the area of an organically changed vessel wall, there is a high probability of relapse. Therefore, after restoration of blood flow, it is necessary to perform a planned reconstructive operation.
If the situation has been neglected and gangrene of the limb has developed, amputation is performed.
Therapy for obliterating arterial diseases
Conservative treatment is prescribed in the early stages of the disease, as well as in the presence of contraindications to surgical treatment methods. Basic principles of therapy:
- Elimination of factors that provoke arterial spasm: smoking, alcohol, hypothermia.
- Prescription of antispasmodics.
- Analgesics for pain relief.
- Reducing blood viscosity by prescribing antiplatelet agents and anticoagulants.
- A diet aimed at reducing blood cholesterol levels.
- Statins to normalize lipid metabolism.
- Treatment of concomitant diseases that have a detrimental effect on blood vessels: hypertension, diabetes, atherosclerosis.
However, the most effective method of treatment remains reconstructive surgery - bypass surgery (creation of a bypass anastomosis), stenting (installation of a stent in the lumen of a vessel).
Let's sum it up
Impaired peripheral circulation can be due to various reasons. It is important to remember that long-term or acute blood flow disorders can lead to irreversible changes in tissues and result in gangrene.
To prevent vascular disorders, it is necessary to maintain a healthy lifestyle, proper nutrition, giving up bad habits, as well as timely treatment of diseases that contribute to the development of angiopathy.
Source: https://FB.ru/article/253710/narushenie-perifericheskogo-krovoobrascheniya-tromboz-i-emboliya
Treatment
A stroke requires emergency medical attention. In case of stroke, treatment is aimed at maintaining the functioning of all important organs. When blood circulation to the brain is impaired, treatment includes breathing support, reducing brain swelling, normalizing blood pressure, and requires monitoring in a hospital. Subsequently, the causes that caused the acute disorder are eliminated, and the impaired functions of the urinary tract are restored.
Chronic cerebrovascular accident requires qualified treatment with drugs to improve brain function. All medications are selected separately taking into account:
- Identified causes of the disorder.
- Stages, type, duration, features of the course of the disease.
- Patient's age and weight.
- Results of diagnostic examinations.
If the disorder is accompanied by cephalalgia, nausea, and dizziness, potent medications are used to relieve unpleasant symptoms and alleviate the patient’s condition. The doctor prescribes:
- Vasodilators, relaxing blood vessels, increasing the lumen.
- Antithrombotic drugs are prescribed for atherosclerosis, thrombosis, and plaque formation.
- Nootropic pharmacological agents that improve urinary function by affecting the metabolic processes of brain structures and tissues.
”alt=””>
A disorder that worsens the blood circulation of the spinal cord and brain is eliminated with supportive therapeutic courses. The patient takes medications daily in the dosage and according to the schedule determined by the doctor. If the disorder is not severe, sedatives are prescribed - mixtures with valerian, motherwort, hawthorn, lemon balm, herbal remedies Sedistress, Novopassit.
Improving blood flow without medications
In the initial stage, cerebral circulatory disorders can be restored without medication. The body has a positive effect:
- Dietary supplements based on plant extracts, minerals, vitamins. Homeopathic medicines that affect human self-regulatory processes. Immunity and metabolism are restored more actively when using homeopathy.
- Manual therapy improves blood flow and eliminates anatomical disorders that affect poor circulation.
- Massage is an effective remedy for cervical osteochondrosis. If there is a suspicion of thrombosis, the procedure is not prescribed.
People who are obese need to reconsider their diet and visit a nutritionist to select an appropriate diet. It is advisable to include in your diet foods that improve blood circulation in the brain, such as:
- Seafood.
- Fish.
- Porridge.
- Legumes.
- Dairy products.
- Vegetables.
- Fruits.
- Blueberry.
- Green tea.
Dishes should contain olive, corn, flaxseed or sunflower oil.
If blood vessels are clogged and blood flow is impaired, it is necessary to avoid foods rich in cholesterol. It is necessary to completely exclude:
- Refined sugar.
- Products made from premium flour.
- Smoked meats.
- Fatty foods.
- Seasonings.
- Nutritional supplements.
- Carbonated drinks.
- Alcohol.
A complete list of permitted and prohibited foods is given by a neurologist or nutritionist.
Breathing exercises aimed at enriching the blood with oxygen are useful. The first sessions should be carried out by a specialist. Without his instructions and the necessary preparation, classes can be dangerous. You can normalize the functioning of the cardiovascular system with yoga, Pilates, and swimming.
Treatment with traditional methods
Alternative medicine is an excellent way to relieve unpleasant symptoms in combination with medications.
- Poor blood circulation in the brain, accompanied by tinnitus and dizziness, is treated with alcohol tincture of red clover. The inflorescences are filled with alcohol or vodka until the flowers are completely covered. After this, the clover is allowed to brew for 3 weeks in a cool, dark place. Drink the medicine before meals, 1-2 tsp.
- Sweet clover has a positive effect on blood clots. It improves circulation, thins the blood, and prevents plasma thickening. Brews like tea.
- The outflow and inflow of blood is improved by meadowsweet inflorescences and horse chestnut tincture.
Plants should be used for treatment after consultation with a doctor. Many herbs, if prepared and taken incorrectly, can cause excessive bleeding.
Diagnosis and treatment
Treatment of peripheral circulation disorders of the lower, upper extremities and other places largely depends on the cause that provoked the development of the pathological process and the nature of the damage. Therefore, before making a decision, the doctor prescribes tests to find out peripheral blood counts. Then the doctor draws up a treatment plan.
The analysis will allow you to find out the number of leukocytes, platelets, erythrocytes, hemoglobin, elements found in the plasma, and their ratio to each other. If necessary, immunophenotyping of cells is carried out, that is, it is determined whether there are CD antigens on the surface of leukocytes to determine the nature of certain diseases (for example, in cytology, analysis helps to determine certain types of tumors, the state of the cardiovascular system, and the musculoskeletal system). Thanks to this, the doctor will be able to understand the nature of the disease, as well as in which direction to prescribe other studies.
Against the background of acute circulatory disorders in the vessels of the lower and upper extremities, heart, brain, and other organs, in most cases it requires surgical intervention. Before this, be sure to do all the necessary tests to determine the cause of the disease.
The operation is needed because the use of medications is unable to completely destroy the clumped platelets or red blood cells that have clogged the vessel. After restoration of blood flow, in order to prevent relapse, planned reconstructive surgery is necessary. As a last resort, if possible, the affected organ is removed. In this case, the person is given a disability, and he himself often needs nursing care.
Against the backdrop of a slowly developing pathological process, good results can be achieved with the help of medications and other therapies. To improve the situation, you must give up bad habits that cause vasospasm (alcohol, smoking). For the same purpose, hypothermia should be avoided.
Medicines and other means aimed at improving blood flow and microcirculation should be prescribed by a doctor. He also draws up a treatment plan based on the results of blood and plasma cell tests. An analysis of the number of platelets, red blood cells, hemoglobin, leukocytes, and other plasma cells, as well as ultrasound, x-rays and other examinations will help him determine the nature of the pathological process.
If the analysis shows that circulatory problems are observed due to vasoconstriction, the doctor may prescribe drugs that dilate blood vessels, as well as drugs that improve blood microcirculation. Against the background of increased blood viscosity, the doctor, having ordered tests, finds out the cause (if necessary, prescribes immunophenotyping of cells), draws up a treatment regimen, prescribing drugs and agents aimed at thinning it.
Disruption of microcirculation, which appears in the early stages of atherosclerosis, is a reason to prescribe drugs aimed at dissolving cholesterol plaques and improving blood microcirculation. You will also need to adhere to a special diet with a minimum amount of animal fats. To avoid making mistakes in choosing foods, the diet is prepared by a nutritionist.
Surgeries for acute blood flow disorders
Conservative treatment in this case is ineffective, because it is not able to completely destroy the blood clot and eliminate the obstruction to blood flow. Its use is possible only in cases of severe concomitant pathology, provided that compensatory reactions are sufficient. After stabilizing the patient's condition, an operation is performed to remove the blood clot from the lumen of the vessel.
Blood flow is restored as follows. A Fogarty catheter is inserted into the lumen of the affected artery above the blockage, with the help of which the blood clot is removed. To insert a catheter, surgical access is carried out at the level of the bifurcation of the femoral artery (if the lower limb is affected) or the brachial artery (if the upper limb is affected). After performing an arteriotomy, the Fogarty catheter is advanced to the site of blockage of the vessel by a thrombus, passed through the obstruction, after which it is inflated and removed in this state. The inflated balloon at the end of the catheter captures and carries the clot along with it.
If thrombosis occurs in the area of an organically changed vessel wall, there is a high probability of relapse. Therefore, after restoration of blood flow, it is necessary to perform a planned reconstructive operation.
If the situation has been neglected and gangrene of the limb has developed, amputation is performed.