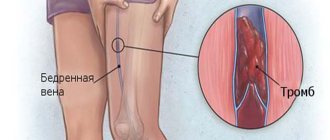
The disease pelvic thrombophlebitis is inflammatory changes in the venous wall, accompanied by the formation of a blood clot. The pelvic veins, common, external, internal iliac and their branches are affected. As the disease progresses without proper treatment, there is a high probability of instant death due to a detached blood clot entering the pulmonary artery. Women at risk are during pregnancy, childbirth, and abortion.
Inflammation of the pelvic vessels and the formation of blood clots are very dangerous, because carries the threat of rapid, unpredictable death.
The main causes of the disease
The following factors can cause thrombosis of the pelvic and iliac veins:
- previous injuries or surgeries in the pelvic area;
- long bed rest;
- the use of oral contraceptives that can disrupt the endocrine system;
- pregnancy;
- childbirth and the postpartum period;
- tumor in the pelvis;
- insufficiency of venous valves;
- presence of hemocoagulation;
- aneurysm.
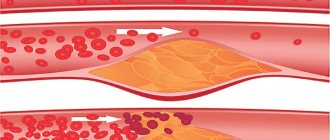
However, for the disease to occur, the presence of Vikhrov’s triad is necessary:
- structural disorders of the venous walls;
- slow blood flow;
- increased blood clotting.
Symptoms of thrombophlebitis
Pelvic vein thrombosis has the following symptoms:
Inflammation of the pelvic vessels is accompanied by swelling, weakness, fever, and changes in skin color.
- swelling of the limb, accompanied by painful sensations;
- cyanosis of the skin;
- strengthening of the subcutaneous vein pattern;
- impaired joint mobility;
- weakness;
- adynamia;
- increased body temperature;
- tenesmus, dysuric phenomena.
The disease has a mild onset, which makes diagnosis difficult. The patient feels mild pain in the sacral and lumbar region, as well as in the lower abdomen. If the thrombus completely blocks the iliac vein, the pain is sharp in the groin area, and swelling of the lower limb is observed due to inflammation. Depending on the area of the affected vessel, swelling can spread to the genitals, abdomen, and buttocks. The skin becomes pale, with a pronounced purple pattern. If pelvic thrombosis is accompanied by severe inflammation, the patient feels chills, fatigue, and body temperature rises to 39 degrees. Nausea, vomiting, and diarrhea are observed. Symptoms of pelvic vein thrombosis are accompanied by damage to the affected organs.
The main symptom of thrombophlebitis of the pelvic veins is a dull pain in the area of the bladder, anus and genitals.
Forms of pathology
Inflammation of the pelvic vessels differs in the intensity of the disease.
Symptoms of the acute course of the disease occur suddenly and are accompanied by a sharp deterioration in well-being. The local skin temperature increases, the pain changes its localization and is bursting in nature. The saphenous veins become overfilled with blood due to a disruption in the outflow of venous blood to the leg, but the influx of arterial blood remains. If these symptoms are present, the patient should urgently consult a phlebologist for medical help, as there is a risk of developing thromboembolism, which is characterized by the separation of the formed blood clot and blockage of the vessel.
In the chronic course, the patient is bothered by aching pain during significant physical exertion, but the symptoms disappear after rest. If you do not undergo the examination on time, there is a risk of developing complications, such as thrombosis of the great vessels, deep vein thrombophlebitis, and chronic venous insufficiency.
What will happen after the operation?
Typically, patients feel dramatic relief after surgery and note a decrease in pain (Fig. 6). Sometimes continued minimal pain therapy is required. The main task of the patient in the postoperative period is to normalize stool: soft stool causes much less pain during bowel movements than dense stool. As a rule, patients return to their normal lives 2-3 days after surgery, sometimes the very next day.
a)
b)
Rice. 6. View of the anus before (a) and immediately after removal of the external hemorrhoid (b). Before the operation, the patient rated the pain level as 8 out of 10, immediately after the operation it was 4 out of 10.
Diagnostic methods
The most common and informative diagnostic tool is duplex ultrasound angiography. The method is based on visualization of the lumen of the veins, assessment of the diameter and degree of occlusion of the vessel, as well as the extent and size of the thrombus. If the results of angiography are not informative enough, venography is performed - an X-ray examination with a contrast agent. Using this method, filling defects in the lumen of the vein are detected, which may indicate the presence of non-occlusive thrombosis. In difficult cases, magnetic resonance venography may be performed.
Treatment of thrombophlebitis of the pelvic and iliac veins
Drug therapy
Patients with acute thrombophlebitis undergo immediate hospitalization. In the hospital, the patient is given antithrombic therapy using hemorheological active drugs, anticoagulants, and NSAIDs. The first group of drugs is prescribed to reduce blood viscosity, stimulate blood microcirculation, reduce the clumping of red blood cells, leukocytes, and platelets.
Hemorheological drugs help cope with inflammation of the pelvic vessels and blood clots.
Hemorheological drugs:
- "Reopoliglyukin";
- "Trental";
- "Courantil";
- "Troxerutin";
- "Detralex";
- "Eskuzan."
Prescribing anticoagulant therapy prevents blood clotting and promotes a therapeutic effect. A contraindication is a duration of illness of more than 20 days. The use of low molecular weight heparin reduces the likelihood of remission of blood clots by up to 50% within 3 months after completion of treatment. To combat inflammation in the affected area and relieve pain, NSAIDs are prescribed. The main drugs are derivatives of Ketoprofen and Diclofenac.
Surgery
The indication for surgery is blockage of blood vessels, and use is necessary to restore blood circulation in the damaged vein. In case of chronic thrombophlebitis, surgical manipulations are not advisable. If a patient has been diagnosed with an embolic thrombus, surgical intervention is mandatory.
The following operations apply:
- plication of the inferior vena cava;
- thrombectomy;
- endovascular manipulation;
- ligation of the main veins.
Mode correction
You cannot stay in bed for a long time. This is due to immobility of the limb, which contributes to the progression of thrombosis due to slower fluid circulation in the vessels. After 10 days, if there is no risk of thromboembolism, it is recommended to apply a compression bandage to the leg and perform light therapeutic exercises. Gymnastics helps improve venous outflow.
Risk factors
Postpartum thrombophlebitis has a higher percentage of its occurrence in certain clinical situations. The doctor’s task is to identify such factors and prescribe timely prevention in the form of drug treatment, wearing compression garments, certain physical activity, etc.
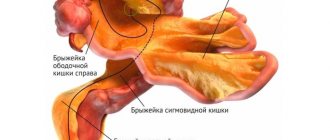
Pregnancy and childbirth
The period of gestation and the birth of the baby are independently provoking moments for the development of thrombophlebitis. This is due to rheological changes in the blood, as a result of which it becomes more viscous, especially on the eve of childbirth. The increasing size of the uterus puts pressure on nearby vessels, which disrupts the outflow of blood from the lower extremities, contributing to its stagnation, the progression of varicose veins and the formation of blood clots. All this is favored by hormonal levels.
Varicose veins of the legs
All women who had any, even minor manifestations of varicose veins before or during pregnancy, have an increased risk of blood clots after childbirth. Ideally, it is better to operate on varicose veins before planning conception, since in most cases, during pregnancy, all symptoms worsen, especially in the third trimester.
Throughout pregnancy, such women are recommended to wear compression garments of the required compression class. The choice should be made together with your doctor.
Particular caution should be exercised if they or close relatives have a history of thrombophlebitis, especially deep veins. In such cases, treatment is supplemented with drugs that normalize blood clotting.
All pregnant women with manifestations of varicose veins should undergo an ultrasound examination of the vessels of the legs to identify blood clots in them. Detection of such blood clots makes it possible to take all possible measures to prevent the progression of the disease. In some cases, special vena cava filters are placed over the pathological area, so the blood clot cannot migrate further.
Massive blood loss
Physiological during childbirth is a loss of up to 10% of the total volume of circulating blood. This is about 500 ml. Massive blood loss causes activation of the coagulation system, which should prevent its progression. In some situations, a breakdown occurs at this stage, causing DIC syndrome. In this case, blood clots begin to form in all vessels and organs. To prevent this, blood loss should be replenished in a timely manner.
In case of injury
During any surgical intervention (whether it is suturing ruptures or the process of cesarean section), the risk of blood clots sharply increases due to tissue trauma and activation of the blood coagulation system. The larger the volume, the higher the risk. For example, if we compare a caesarean section without and with removal of the uterus, then in the second case the likelihood of thrombosis will be many times greater.
Woman's age
It has been proven that the risk of thrombophlebitis increases with age. The limit is 35 - 40 years, after which any surgical intervention is accompanied by the prescription of anticoagulant therapy (counteracts excessive clotting).
Obesity, smoking
A woman's metabolic disorder, leading to excess weight, also entails a risk of thrombosis. This is due to physical inactivity, especially during pregnancy. Also, with obesity, the walls of blood vessels are injured by metabolic products and contribute to the formation of blood clots. Smoking aggravates the whole situation: nicotine affects the rheological properties of the blood, increasing its viscosity.
Often in the third trimester of pregnancy, women, especially those with risk factors, develop gestosis. The pathology is characterized by a triad of symptoms: swelling, increased blood pressure and impaired renal function. The formed elements of blood also undergo changes. All this leads to an increase in the risk of trorobophlebitis several times compared to healthy women.
Diseases of the cardiovascular system
Also risk factors are all diseases of the heart and blood vessels. Of particular danger are arrhythmias, artificial valves, defects, etc.
Presence of cancer
Any malignant tumor increases the risk of thrombosis. At the current level of development of obstetrics and gynecology, women with oncology often successfully carry a pregnancy, but it is always necessary to be wary of hypercoagulation. Today, it is not uncommon to give birth after surgery on the cervix, after melanoma, etc.
Prolonged bed rest
Physical inactivity, including in the postpartum period, increases the likelihood of thrombophlebitis due to stagnation of blood in the veins of the legs. Prolonged bed rest may be prescribed after major ruptures or surgeries and other complications.
Read also: Thrombophlebitis after injection
Hereditary thrombophilias
Currently, various types of genetic diseases are increasingly being identified, which can cause infertility, miscarriage at different stages, as well as thrombotic complications. All these diseases are combined into the group of hereditary thrombophilias. Timely diagnosis and treatment – prevention of dire consequences.
Prevention
To prevent inflammation of the pelvic vessels, you need to improve your lifestyle, eat right, and give up bad habits.
To prevent thrombosis, it is recommended to adhere to proper nutrition, healthy sleep, exercise, and get rid of bad habits. Particular attention should be paid to the condition of blood vessels after childbirth. When the first symptoms of the disease occur, you should consult a doctor for diagnosis and timely treatment.
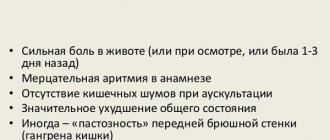
Is it always necessary to treat acute thrombosis of the external hemorrhoid?
The choice of treatment method for this disease is one of the most controversial issues in general proctology. Like hemorrhoids, acute thrombosis does not turn into cancer, does not cause deadly complications, but can significantly affect the patient’s quality of life; the pain syndrome is often described as “unbearable”, with which it is “simply impossible to live.”
Our Clinic has adopted a patient-centered approach to choosing a treatment method for acute thrombosis of external hemorrhoids: the doctor, together with the patient, determine how severe the symptoms are, how much the patient’s quality of life suffers, taking into account his employment, and choose a treatment method.
Acute thrombosis of the external hemorrhoid can be treated promptly (perform surgery), conservatively (take pills and use topical ointments and/or suppositories) or not treat at all, but choose a wait-and-see approach. Research and practical experience show that surgical treatment allows you to get rid of the manifestations of the disease in a shorter time; conservative treatment also allows you to get rid of the manifestations of the disease, but over a much longer time. The absence of any treatment also ends with recovery, the timing of which differs only slightly from the timing of intensive conservative treatment. The determining factor in the choice of treatment method is the patient’s choice and his assessment of the severity of the pain syndrome, therefore, the patient’s opinion is crucial for the choice of tactics. If the patient assesses the pain as unbearable, or he urgently needs to return to work, fly to another city or country, it is more reasonable to choose surgical treatment in the scope of removing the hemorrhoidal node or evacuating the blood clot from the node. Surgical treatment usually leads to faster relief of unpleasant symptoms. If the pain syndrome allows the patient to live fully in this condition or the patient is not ready for surgical intervention, it is possible to carry out conservative treatment aimed at reducing the pain syndrome and accelerating the process of organizing and resolving the blood clot.