Why are they needed?
Each method is important for determining ischemia and distinguishing it from other cardiac disorders.
Examinations are indicated for:
- confirmation of the disease if angina is suspected;
- establishing a diagnosis;
- detection of risks of developing complications from the cardiovascular system;
- assessing the success of therapy;
- prognosis of consequences and complications.
The results obtained allow us to assess the patient’s condition and the stage of the disorder.
Stable angina (tension)
Depending on the threshold of physical activity at which pain occurs, four functional classes (FC) of stable angina are distinguished.
| Function class | Characteristic |
| FC-I | attacks occur rarely, with significant, excessive load |
| FC-II | painful attacks are observed when walking quickly over a distance of more than 300 m or when climbing more than one floor on the stairs. Provoking factors are: cold windy weather, stress, smoking. The first hours of wakefulness are unfavorable, when there is a physiological increase in heart rate, blood pressure, platelet activation, and a decrease in antifibrinolytic ability (circadian rhythm of angina) |
| FC-III | pain when walking a distance of 150-300 m or when climbing one floor of stairs at a normal pace. |
| FC-IV | pain occurs with minimal physical activity, as well as at rest. |
Anamnesis
Before determining coronary heart disease, the doctor must study the medical history. First of all, it is necessary to listen to the patient’s complaints.
With a typical type of angina, a characteristic manifestation is chest discomfort. This is a squeezing, pressing, burning pain that occurs in one place. At rest or after using nitroglycerin, symptoms disappear.
It is necessary to clarify when the pain syndrome appeared and whether the patient was taking medications. A history of pathologies that reduce the level of oxygen in the myocardium should be excluded. For example, fever, hyperthyroidism, excessive emotional stress.
Tests for ischemic heart disease are also prescribed in the following cases:
- tachycardia;
- aortic disease;
- hypertrophic cardiomyopathy.
Concomitant anemia, inflammatory and chronic lung disorders, hypertension, apnea syndrome reduce the supply of oxygen to the body. The specialist questions the patient for bad habits and alcohol consumption.
Recent viral and infectious diseases have an impact on cardiac problems. Genetic predisposition should also be excluded.
Angina pectoris - classification, causes, symptoms, diagnosis, treatment
Angina pain (angina pectoris) is a pathology that is a variant of ischemic heart disease (CHD), and is manifested by cardiac attacks that occur against the background of oxygen starvation of the myocardium.
If pain is initiated by physical activity, then doctors talk about angina pectoris. In cases where chest pain develops during sleep or during rest, we are talking about a pathology of rest.
In addition, there is also stable and unstable angina.
Currently, a variety of classifications are used to fully characterize angina.
In their practice, cardiologists prefer to use its classic versions, which have the only standard around the globe.
New-onset angina pectoris
The diagnosis is made after the first attacks in life, lasting from 4 to 6 weeks. At this time, the patient’s condition is monitored, and after three months a conclusion is made about the transition of new-onset angina to an unstable or progressive form.
In the WHO International Classification of Diseases, the last revision of the classification of IHD was carried out in 1995, but this version is still relevant.
Symptoms of angina pectoris
Stable exertional angina
IHD is not divided into functional classes; instead, the modern classification of IHD involves a more detailed diagnosis, where stable angina pectoris is divided into groups according to such an indicator as the patient’s tolerance to physical activity. There are 4 classes:
- Functional class I - with this diagnosis, daily physical activity is not contraindicated for the patient, and the occurrence of pain in the heart is possible only during prolonged training or other heavy physical activity.
- Functional class II - the load is not fully limited, and an angina attack begins when you need to walk more than 500 meters or climb higher than one flight of stairs;
- III functional class - it becomes difficult for the patient to walk less than half a kilometer or climb to the 1st floor, since these conditions are sufficient for the onset of an attack;
- Functional class IV is called the severe degree of this form of IHD. The slightest load triggers an attack.
Progressive angina pectoris
This type can be discussed in the following cases:
- pain occurs more often and is not associated with physical activity, or occurs with less activity than before;
- the usual doses of medications do not stop the attack;
- other symptoms are noted - nausea and vomiting, a feeling of suffocation may appear;
- the localization of pain changes;
- attacks become longer and more painful for the patient.
It is very important to immediately recognize progressive angina and consult a specialist to prescribe new medications. It is necessary to realize that this form is unstable and refers to a pre-infarction state, therefore, conventional medications may not be enough to stop the attack.
Spontaneous exertional angina
It is also called “vasospastic” or “Prinzmetal” after the name of the scientist who studied it, and the definitions “variant” and “special” are also found.
It is quite rare and is characterized by the unexpected occurrence of coronary artery spasm, not associated with physiological stress. It appears more often at night or early in the morning and does not last long - a few minutes.
The main reason for its occurrence is the presence of atherosclerotic plaques in the patient.
Braunwald classification
The Braunwald classification is used in relation to the unstable form of angina, as a variant of the course of chronic ischemic heart disease. Unstable angina according to Braunwald has three functional classes regarding the main characteristics of pain:
- Class 1 - includes angina pain from tension, angina that has arisen for the first time, a progressive type of the disease and severe forms of the disease in the absence of angina at rest over the past two months.
- Class 2 - represented by angina at rest, as well as a subacute form of the disease, which last appeared within a month, but not in the last 2 days before the examination.
- Class 3 – angina at rest and the acute form of the disease, as well as angina pectoris at rest, which occurred in the last 2 days.
Regarding the main factor that provoked the development of the attack, angina pectoris according to Braunwald is divided:
- Class A is a disease that occurred secondary, regardless of the coronary factor, and was provoked by diseases such as anemia, hypoxia, intoxication of bacterial, viral, toxic origin.
- Class B – primary angina pain itself, provoked by coronary circulatory disorders.
- Class C – angina pectoris, which arose after acute forms of coronary artery disease (myocardial infarction) for two weeks after their development.
Analyzes
Laboratory blood tests help determine the presence of factors that increase the risk of developing cardiovascular pathologies and their causes.
List of laboratory diagnostics:
- general blood test (special attention is focused on determining hemoglobin);
- biochemical;
- lipid spectrum;
- glucose level;
- determination of creatinine content.
If signs of coronary artery disease are detected, they may additionally refer you for a blood draw for troponins. If you suspect the presence of a disease, it is necessary to examine the level of hormones. Additionally, a glucose load test is performed.
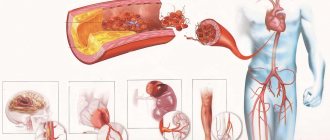
Myocardial infarction
Myocardial infarction is a form of ischemic heart disease that develops as a result of prolonged ischemia and is characterized by necrosis of individual areas of the heart muscle. The classification of IHD divides this form into two broad groups.
Transmural infarction (large focal), in which the entire muscle layer of one of the walls of the heart muscle is affected. More dangerous than other types of IHD. The mortality rate of patients still remains high - up to 30% of all hospitalized;
Small-focal infarction has a significantly more favorable prognosis and is characterized by less damage to the heart muscle. In the case of this form of coronary artery disease, small foci of necrotic heart tissue are noted, but they can also develop into a more extensive lesion and transform into a large-focal infarction.
How does myocardial infarction occur?
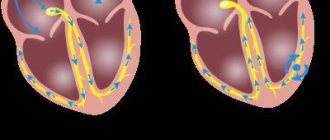
ECG and Echo KG
Diagnosis of coronary heart disease necessarily consists of an ECG. At rest there are no characteristic indicators. Therefore, a recording is made when pain occurs. In this case, a horizontal downward displacement of the ST segment will be observed.
If the ECG is performed at rest, the graph will display the consequences of a myocardial infarction that the patient has suffered in the past. Disturbances in cardiac rhythm and conduction are also detected. The data obtained are important for diagnosis and proper therapy.
Echocardiography for ischemic heart disease is prescribed mainly to verify its presence, and not other diseases. Diagnostics is indicated for:
- extraneous noise;
- heart failure;
- suffered a heart attack.
Partially modifiable risk factors for coronary heart disease
Pathological conditions that contribute to the development and progression of atherosclerosis include:
- Dyslipidemia – high levels of cholesterol, saturated fats, decreased levels of high-density lipoproteins.
- Hypertension – high blood pressure leads to myocardial hypertrophy, which impairs coronary blood flow.
- Diabetes mellitus – insulin deficiency causes an increase in glucose and cholesterol levels in the blood.
- Blood coagulation disorders - increased fibrinogen and platelet aggregation rate accelerate thrombus formation.
- Obesity is the most dangerous abdominal obesity, as it is combined with impaired insulin sensitivity, increased blood pressure and cholesterol levels in the blood.
- Infections – the development of atherosclerosis was noted after suffering from herpes, chlamydia, cytomegalovirus disease, as well as in the presence of persistent foci of infection (tonsillitis, periodontitis).
We recommend reading about post-infarction cardiosclerosis. You will learn about the causes and symptoms of the disease, classification, complications, diagnosis and treatment. Read more about the complications of myocardial infarction here.
Load tests
One of the examination options is an ECG. When the patient is at rest, changes are not displayed.
To do this, use different loads to achieve heart rate. Therefore, an ECG test with physical activity is recommended. This method is considered the initial one in the diagnosis of angina pectoris.
It is carried out in stationary conditions on an exercise bike. The load is added gradually, and the diagnostician monitors the indicators on the monitor. If characteristic symptoms occur, the test is considered positive.
If it is not possible to conduct a test, diagnosticians perform transesophageal electrical stimulation. During the procedure, a thin probe is inserted into the esophagus. With its help, the myocardium is stimulated with electrical impulses, which lead to an increased heart rate.
Another technique is stress echocardiography. With the development of ischemia, a decrease in the myocardium is initially observed, and then changes are observed in the curve. The method is considered informative, but technically complex.
Initially, they do the usual tests for ischemic heart disease, and then check for increased heart rate using medications and equipment - a bicycle ergometer, a treadmill.
Diagnostic measures
After analyzing the patient's complaints and compiling a medical history. Then you need to undergo general blood and urine tests. A preliminary diagnosis of IHD can be confirmed or excluded by doing a blood test for cholesterol plaques. Then the cardiologist refers you to complex hardware diagnostics.
For ischemic heart disease and angina pectoris, the following diagnostic measures may be recommended to the patient:
- Ultrasound of the heart (echocardiography) – prescribed to determine the extent of damage to the heart arteries;
- coronary angiography - done with the aim of tracing processes in blood vessels, studying the dynamics of blood circulation, as well as assessing the condition of their internal walls;
- Holter ECG. This study consists of round-the-clock monitoring of the heart using a special device (the patient wears a portable recorder that records the state of the organ under various loads);
- Computed tomography - is done to clarify the diagnosis if the clinical picture of angina pectoris is similar to signs of other pathologies;
- A running test is a study that allows you to study the body's response to various types of physical activity.
Computer research
This examination is based on an x-ray examination of the heart. Usually performed on men and women aged 45-55 years. They also refer patients with atypical pain syndrome and questionable stress test results.
allows to exclude myocarditis, cardiomyopathy.
Coronary angiography is the main method for diagnosing ischemia. In addition, it provides the opportunity to determine effective therapy. Taking into account the results, a treatment method is prescribed - medication or surgery.
The essence of the procedure is to introduce a contrast agent into the bloodstream, which does not pass through blockages in the heart and blood vessels. Test results for coronary artery disease are necessary for a cardiologist.
Modifiable risk factors for coronary artery disease
Half of all diseases are caused by an unhealthy lifestyle, and for the cardiology group this figure is even higher. Therefore, removable risk factors for coronary artery disease are the most promising category; their elimination significantly reduces the incidence of damage to the heart and blood vessels.
There are reasons that do not directly depend on the person (genetics, ecology, age, level of medicine), but after eliminating bad habits, you can transfer the disease to a milder form and avoid complications.
Eating habits
The basis for the violation of fat metabolism in the body is the consumption of foods that contain large amounts of cholesterol and other saturated fats. These are primarily animal products:
- fatty varieties of lamb, pork, beef;
- offal (brains, liver, kidneys, lung, heart);
- sausage, frankfurters and sausages;
- eggs;
- butter, heavy cream;
- canned fish in oil, mackerel, carp;
- semi-finished meat products, ready-made minced meat.
Their consumption leads to the accumulation of cholesterol in liver cells. This reduces the formation of special receptors that capture fats from the blood. Therefore, atherogenic lipids remain in the vascular bed and are fixed on the walls of the arteries. Reducing the proportion of fatty meat in the diet helps slow down the blockage of the lumen of the vessel, and, consequently, increase the length and quality of life.
In addition, you need to include in your daily menu foods that help remove excess saturated fatty acids from the body and prevent fatty liver degeneration. These include dietary fiber contained in vegetables and fruits, bran and cereals, as well as unsaturated fats from vegetable oils, fish, and seafood. The healthiest combination is boiled fish with herbs and a salad of fresh vegetables with vegetable oil.
Smoking
The condition of blood vessels and the blood coagulation system is negatively affected not only by nicotine, but also by a huge number of chemical compounds from tobacco smoke. Their action is manifested in this way:
- stimulation of adrenaline receptors;
- increased need of myocardial cells for oxygen;
- increased excitability of the heart muscle;
- rhythm disturbance and risk of muscle fiber fibrillation;
- decreased transport and absorption of oxygen due to the combination of hemoglobin with low concentration of high-density lipoproteins in the blood;
- high risk of blood clots.
Quitting smoking or reducing the number of cigarettes smoked helps normalize blood flow and nutrition of the tissues of the heart, brain, limbs, and restores lung and kidney tissue.
Stress
The release of adrenal hormones into the blood when exposed to a psycho-emotional stimulus is most dangerous for people whose reaction belongs to behavioral type A. It is also called coronary, since the risk of atherosclerosis and heart attack in such individuals increases even at a young age. Main features:
- desire to compete and dominate;
- intolerance to other people's opinions;
- cruelty, aggressiveness, outbursts of anger;
- constant rush, lack of time.
Neutralizing such character traits often requires the help of a psychologist, mastering relaxation techniques, and allocating sufficient time in the daily routine for rest.
Alcohol
Although there is evidence of the benefits of moderate consumption of alcoholic beverages for the condition of blood vessels, they cannot be recommended for the prevention of atherosclerosis due to
for such an effect on the body:
- increased blood pressure;
- risk of cardiac arrhythmia and sudden cardiac arrest;
- addiction with the need to increase the dose.
The maximum dose of ethanol is 30 g per day no more than 2 times a week. This amount is contained in a glass of wine or 70 g of spirits. It should be borne in mind that alcohol has a stronger effect on women, so you need to control the amount of alcohol taken even more carefully.
Lack of movement
The incidence of myocardial ischemia with low levels of physical activity is two times higher than in those who lead an active lifestyle. The optimal activities for the prevention of coronary artery disease should be:
- frequency per week – 4 or 5 times;
- regular, without long breaks;
- duration 30 minutes (5-10 minutes are allocated for warm-up and final recovery);
- heart rate 50 - 70% of maximum (220 minus age);
- in case of heart disease, the activity level is determined after exercise tests during an ECG.