I34 Non-rheumatic lesions of the mitral valve
Excludes: mitral (valve): disease (I05.9), insufficiency (I05.8), stenosis (I05.0), lesions specified as rheumatic (I05.), with an unknown cause, but with mention of: aortic valve disease (I08.0), mitral stenosis or obstruction (I05.0)
I34.0 Mitral (valve) insufficiency
I34.1 Prolapse (prolapse) of the mitral valve
Excludes: Marfan syndrome (Q87.4)
I34.2 Non-rheumatic mitral valve stenosis
I34.8 Other non-rheumatic lesions of the mitral valve
I34.9 Non-rheumatic disease of the mitral valve, unspecified
Treatment
TREATMENT Management tactics • Treatment of the underlying disease in secondary MVP • Risk groups for the development of complications (patients with severe systolic murmur, thickened prolapsed mitral valve leaflets, left ventricular hypertrophy, rhythm disturbances, fainting) undergo regular ECG, echocardiography • Prevention of endocarditis is indicated for persons with severe systolic murmur. Treatment of various options • For asymptomatic MVP without signs of mitral valve insufficiency, there is no need for treatment •• The patient should be given recommendations for normalizing lifestyle, optimizing physical activity (a decrease in the tone of the sympathetic nervous system can lead to a decrease in valvular dysfunction) •• EchoCG is recommended — control once every 1–2 years •• It is necessary to avoid drinking strong tea, coffee, alcohol, as well as smoking • For severe MVP •• If there are symptoms of MVP such as tachycardia, palpitations, chest pain, is prescribed — adrenergic blockers in small doses (for example, propranolol at a dose of 30–60 mg/day) •• In case of dilatation of the left atrium and left ventricle, prolongation of the QT interval, a history of fainting, dilatation of the initial part of the aorta, physical activity is prohibited •• Prevention is recommended infective endocarditis using amoxicillin •• For symptoms of embolization, acetylsalicylic acid is prescribed at a dose of 80–325 mg/day •• With significant changes in hemodynamics, increasing symptoms of mitral valve insufficiency, mitral valve replacement or annuloplasty is performed.
Prognosis and complications . Typically, MVP is benign. Complications of MVP most often occur in patients with systolic murmur, thickened, elongated mitral leaflets, or enlarged left ventricular cavity or left atrium. Complications include: • separation of tendon threads • severe mitral valve insufficiency (0.06%) • fibrin deposition on the mitral valve leaflets • cardiac arrhythmias • cerebrovascular pathology (0.02%) • infectious myocarditis (0.02%) • sudden cardiac arrest death (0.06% of cases with severe mitral valve insufficiency). Synonyms • Systolic click-murmur syndrome • Barlow's syndrome • Inflated mitral valve syndrome. Reduction. MVP - mitral valve prolapse.
ICD-10 • I34.1 Prolapse [prolapse] of the mitral valve
Classification
According to this international classification, ICD 10 code lists all existing heart defects.
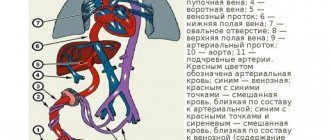
There are quite a few of them. Conventionally, all defects can be divided into two groups, each of which has its own subgroups:
- White. Heart diseases in which mixing of venous and arterial blood does not occur.
- defect of the interatrial and interventricular septum;
- pathologies caused by depletion of the pulmonary circulation;
- defects associated with depletion of the systemic circulation;
- pathologies not associated with hemodynamic disorders.
- Blue. Venous and arterial blood mix.
- defects caused by enrichment of the small circle;
- pathologies caused by depletion of the small circle.
Each of the above groups and subgroups has its own specific code, which helps to determine the type of disease as accurately as possible.
Mitral valve prolapse code according to ICD 10
Includes: conditions classified in I05.0 and I05.2-I05.9, specified or unspecified as rheumatic
Excluded: cases specified as non-rheumatic (I34.-)
Rheumatic mitral:
- functional impairment
- regurgitation
In Russia, the International Classification of Diseases
10th revision (
ICD-10
) was adopted as a single normative document for recording morbidity, reasons for the population’s visits to medical institutions of all departments, and causes of death.
ICD-10
introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997. No. 170
The release of a new revision (ICD-11) is planned by WHO in 2017-2018.
Aortic valve congenital:
Excluded:
- congenital subaortic stenosis (Q24.4)
- stenosis in left-sided hypoplastic heart syndrome (Q23.4)
Bicuspid aortic valve
Congenital aortic insufficiency
Congenital mitral atresia
Atresia or severe hypoplasia of the aortic ostium or valve with hypoplasia of the ascending aorta and a defect in the development of the left ventricle (with stenosis or atresia of the mitral valve).
In Russia, the International Classification of Diseases
10th revision (
ICD-10
) was adopted as a single normative document for recording morbidity, reasons for the population’s visits to medical institutions of all departments, and causes of death.
ICD-10
introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997. No. 170
The release of a new revision (ICD-11) is planned by WHO in 2017-2018.
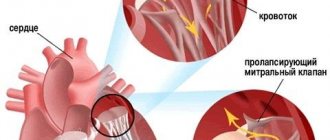
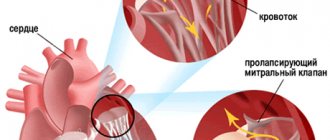
One of the pathologies of the heart and system is MV prolapse. The essence of this disease is that during the contraction of the heart, the valve leaflets bend into the cavity of the left atrium.
Mitral valve prolapse code according to ICD 10 does not apply to diseases that can lead to death.
- 1 Features of pathology
- 2 Classification
Features of the pathology
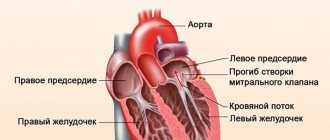
With a healthy heart and circulatory system, oxygenated blood is directed from the pulmonary circulation to the left atrium. Blood then flows through the mitral valve into the left ventricle.
During the contraction of the heart, the blood flow is pushed through the aorta into the systemic circle. Entering the heart, the blood gives all the oxygen to the internal organs and tissues, while taking away carbon dioxide.
After this, the blood flow is directed to the right atrium and ventricle, which constitute the ICC.
The physiology of the functioning of the cardiovascular system is that at the moment of contraction of the heart, the blood completely leaves the left atrium, and the mitral valve leaflets, as a result of their closure, do not allow it to return back.
With mitral valve pathology, part of the blood returns back to the atrium. In this case, such an indicator as the amount of deflection is of great importance. Experts say that if this value is not more than 3 mm, no return flow of blood occurs.
In order to determine the degree of development of prolapse, it is necessary to first find out the amount of deflection of the mitral valve leaflets. The choice of treatment method for MVP depends on this.
Classification
In modern medicine, prolapse, the code of which according to the international classification of diseases is divided into several classes. The following indicators are taken as a basis:
- 1 tbsp. – the index of MC deflection ranges from 3–6 mm. At this stage, there are no major changes in blood circulation. The disease, as a rule, occurs without the manifestation of significant symptoms. In this case, the patient does not need treatment or limitation of physical activity;
- 2 tbsp. – the level of flexion of the mitral valve is not more than 9 mm. Patients with grade 2 prolapse experience symptoms such as short-term pain in the chest, minor attacks of suffocation, headache and rapid heartbeat. Patients diagnosed with stage 2 MVP. Treatment with medications is recommended. Moderate physical activity is allowed;
- 3 tbsp. – this stage of the pathology is characterized by sagging of the mitral valve by more than 9 mm. Symptoms manifest themselves quite clearly and with great frequency. In addition, changes in the anatomy and functioning of the heart and MV are observed. As a rule, the use of drug treatment does not produce any positive results. Therefore, surgical intervention is recommended for the treatment of grade 3 MV prolapse.
- In relation to the time of heart contraction.
- early;
- late;
- holosystolic.
Depending on the class to which the disease belongs, specialists choose one or another course of treatment.
According to statistics, the diagnosis of mitral valve prolapse code according to ICD 10 is made more often in children or adolescents than in adults. Among the reasons that provoke the disease are the following:
- CNS diseases;
- anatomical disorders of connective tissue;
- congenital PS;
- viral diseases;
- poor environmental situation;
- pathologies during pregnancy.
Factors that lead to pathological changes in the mitral valve, as a complication of the current illness, are separately identified:
- lupus erythematosus;
- myocardial infarction;
- congestive heart failure;
- arthritis that develops against the background of rheumatism.
All these factors lead to changes in the connective tissue of the heart muscle, which ultimately provokes the development of MVP.
For patients, mitral valve prolapse, which develops at stages 1 or 2, does not pose any threat to life.
But if the treatment is chosen incorrectly or is not started as early as possible, there is a high probability of complications developing. To avoid this, you should periodically undergo a medical examination by specialists.
Source: https://helpyourheart.ru/sovety/prolaps-mitralnogo-klapana-kod-po-mkb-10.html
Symptoms
When diagnosing congenital heart disease, the pediatrician and cardiologist must first conduct a conversation with the child’s parents.
In this conversation, it is necessary to establish how the child developed, when the first signs of the defect began to appear, etc. A congenital defect leaves its mark not only on the functioning of the heart, but also on many other signs:
- Body type. Few defects can cause changes in physique. For example, if the functioning of the aorta of the heart is impaired, the child experiences accelerated development of the shoulder girdle. As a rule, such children do not gain weight well, and this is reflected in their physique.
- Covers of the skin. If a patient is diagnosed with a white type defect, his skin is too pale. With a blue defect, cyanosis of the integument is clearly manifested.
- Respiratory system. Due to increased blood flow in the lungs, patients with congenital heart disease often suffer from shortness of breath and have difficulty breathing.
- Digestive organs. The disease also affects the digestive system. For example, there is an increase in the size of the liver. Often, such patients experience vomiting with increased physical activity, which is accompanied by severe pain in the abdominal area.
All these symptoms can appear from an early age, or they can begin to remind themselves at the age of 5–6 years.
Diagnostic methods
| Diagnostic method | Characteristic signs of stenosis | Characteristic signs of deficiency |
| History analysis | Often - previous rheumatism. Complaints about asthenia. | Often - previous rheumatism. Complaints of asthenia may be absent for a long time. |
| Visual inspection | Paleness combined with acrocyanosis and blush. Heart hump. | |
| Auscultation of the heart | Purring sounds in the heart area or diastolic murmur | Systolic murmur. Weakening of the first heart sound. |
| Electrocardiogram | Uninformative in the early stages, sometimes signs of atrial fibrillation are revealed | Not very informative in the early stages |
| Radiography | Change in heart shape, expansion of the pulmonary trunk | Left atrium enlargement, esophageal displacement |
| Ultrasound of the heart with Doppler | Pathological changes in hemodynamics and enlargement of individual chambers of the heart | Abnormal blood flow, changes in the anatomy of the valve apparatus |
| Cardiac catheterization | A very accurate diagnostic method in relation to structural disorders of the valve apparatus. Due to its invasiveness, it is practiced only to clarify the diagnosis before surgery. | |
Find out what is the difference between aortic heart disease. These diseases are similar to each other, but there are also significant differences. You can read about congenital blue heart defects here - this is useful information for all future parents.
Diagnostics
The more methods were used to diagnose congenital heart disease code according to ICD 10, the more accurate and detailed the picture of the disease will be visible.
The following methods are used for diagnosis:
- Electrocardiogram. This method gives excellent results, even in the initial stages of pathology development. Based on the interpretation of the cardiogram results, the cardiologist can accurately determine the intensity of the development of the disease and its danger to the child’s life.
- X-ray. When conducting an X-ray examination in 3 projections, the condition of the lungs and the entire respiratory system can be determined.
- Echocardiography. Allows the cardiologist to obtain the most accurate picture of the patient’s condition.
- Angiography or catheterization. These techniques are more difficult to perform, but they allow you to determine the pressure in the lungs, as well as accurately determine in which direction the blood flow is directed (from the right atrium to the left or vice versa).
All of the above diagnostic methods are used in combination.
Only in this case can an accurate diagnosis be established and an effective course of treatment be chosen. Regardless of whether the defect is congenital or acquired, you must be attentive to your health and the health of your loved ones; if one or more signs appear, immediately contact a pediatrician and cardiologist. Be healthy!
Clinics for treatment with the best prices
Price
Total: 1242in 75 cities
| Selected clinics | Phones | City (metro) | Rating | Price of services |
| Trinity City Hospital | +7(495) 851..show Appointment +7(495) 851-06-01+7(499) 638-34-32+7(495) 851-02-76 | Troitsk | rating: 4.4 | 4290ք |
| GoldenMed in Mytishchi | +7(495) 152..show Appointment +7(495) 152-58-54+7(495) 703-03-03+7(495) 984-01-01 | Mytishchi | rating: 4.3 | 5600ք |
| GoldenMed in Lyubertsy | +7(495) 320..show Appointment +7(495) 320-44-78+7(499) 519-35-88+7(495) 703-03-03+7(495) 984-01-01 | Lyubertsy | rating: 4.2 | 5600ք |
| Euromedical clinic on Sirenevy Boulevard | +7(499) 519..show Appointment +7(499) 519-33-83+7(499) 519-33-73+7(495) 126-38-25 | Moscow (metro station Pervomaiskaya) | rating: 4.3 | 5750ք |
| GoldenMed in Krasnogorsk | +7(495) 152..show Appointment +7(495) 152-58-54+7(495) 703-03-03+7(495) 984-01-01 | Krasnogorsk | rating: 4.3 | 5800ք |
| St. Andrew's Hospitals in Korolev | +7(499) 519..show Appointment +7(499) 519-37-02+7(499) 519-35-88+7(495) 518-92-70+7(495) 518-92-72 +7(495) 518-92-80+7(495) 518-92-81 | Korolev | rating: 4.4 | 6100ք |
| Bioss on Khoroshevskoye Shosse | +7(495) 162..show Record +7(495) 162-61-28 | Moscow (metro station Begovaya) | rating: 4.6 | 6150ք |
| ProfMedLab on Presnensky Val | +7(499) 519..show Appointment +7(499) 519-36-96+7(499) 969-21-10+7(495) 125-30-32 | Moscow (metro station 1905 Goda Street) | rating: 4.3 | 6300ք |
| Miracle Doctor on Shkolnaya 11 | +7(495) 109..show Appointment +7(495) 109-70-70+7(495) 638-70-70 | Moscow (metro station Ilyich Square) | rating: 4.4 | 6410ք |
| Miracle Doctor on Shkolnaya 49 | +7(495) 109..show Appointment +7(495) 109-70-70+7(495) 638-70-70 | Moscow (metro station Rimskaya) | rating: 4.5 | 6410ք |
Source
Lost validity - Archive
Also: systolic click-murmur syndrome, Barlov syndrome, sagging valve syndrome, waving mitral leaflet syndrome.
RCHR (Republican Center for Health Development of the Ministry of Health of the Republic of Kazakhstan)
Version: Archive - Clinical protocols of the Ministry of Health of the Republic of Kazakhstan - 2007 (Order No. 764)
ICD categories: Mitral valve prolapse (I34.1)
Reasons for development
Factors that can provoke the birth of a child with a congenital pathology of the development and functioning of the heart can be divided into two large groups:
- Genetic. In this case, we are talking about point gene changes or specific chromosome mutations.
- Ecological. This group includes quite a few factors. Among the main ones are the influence of ion radiation on a pregnant woman and her contact with pesticides. Smoking and drinking alcoholic beverages also fall into this group. If a woman has suffered any infectious or viral diseases during pregnancy, they can also provoke the development of congenital heart disease in the child.
Often the factors that lead to heart pathology can be combined.
Causes
Etiology. MVP can be primary or secondary • Primary MVP •• A disease inherited in an autosomal dominant manner with myxomatous deformation of the mitral valve leaflets •• MVP is also observed in patients with Marfan syndrome and other congenital connective tissue diseases, such as Ehlers-Danlos syndrome, elastic pseudoxanthoma, osteogenesis imperfecta •• In the occurrence of MVP, exposure to toxic agents on the fetus on the 35th–42nd day of pregnancy may also be important • Secondary MVP can occur with: •• IHD (ischemia of the papillary muscles) •• rheumatism (post-infectious sclerotic changes) • • hypertrophic cardiomyopathy (disproportionally small left ventricle, change in the location of the papillary muscles).
Pathogenesis • Primary MVP •• Myxomatous degeneration of collagen leads to excessive accumulation of mucopolysaccharides in the middle spongy part of the mitral valve leaflets and its hyperplasia, which causes the appearance of break areas in the fibrous part of the valve.
Local replacement of the elastic fibrous tissue of the valve leaflet with a weak and inelastic spongy structure leads to the fact that during systole, under the influence of blood pressure from the left ventricle, the leaflet bulges towards the left atrium (prolapses) •• In the occurrence of primary MVP in Marfan syndrome, it is also important dilatation of the annulus fibrosus of the mitral valve - it does not decrease by 30% in systole, as is normal, which leads to protrusion of one or both leaflets into the cavity of the left atrium • Secondary MVP occurs as a result of thinning and elongation of the tendon threads or their separation or dilatation of the fibrous ring. Lengthening of the tendon threads, separation of part of them lead to the fact that the leaflet is not held in place and begins to prolapse into the left atrium • If the mitral valve leaflet is excessively bowed, mitral regurgitation may occur with dilatation of the left atrium and left ventricle. It should be noted that MVP can be combined with prolapse of other valves: tricuspid valve prolapse in 40% of cases, pulmonary valve prolapse in 10%, aortic valve prolapse in 2%. In this case, in addition to mitral valve insufficiency, manifestations of insufficiency of the corresponding valve will occur. There is often a combination of MVP with other congenital anomalies of the heart - ASD, additional conduction pathways (usually left-sided).
Symptoms
When diagnosing congenital heart disease, the pediatrician and cardiologist must first conduct a conversation with the child’s parents.
In this conversation, it is necessary to establish how the child developed, when the first signs of the defect began to appear, etc. A congenital defect leaves its mark not only on the functioning of the heart, but also on many other signs:
- Body type. Few defects can cause changes in physique. For example, if the functioning of the aorta of the heart is impaired, the child experiences accelerated development of the shoulder girdle. As a rule, such children do not gain weight well, and this is reflected in their physique.
- Covers of the skin. If a patient is diagnosed with a white type defect, his skin is too pale. With a blue defect, cyanosis of the integument is clearly manifested.
- Respiratory system. Due to increased blood flow in the lungs, patients with congenital heart disease often suffer from shortness of breath and have difficulty breathing.
- Digestive organs. The disease also affects the digestive system. For example, there is an increase in the size of the liver. Often, such patients experience vomiting with increased physical activity, which is accompanied by severe pain in the abdominal area.
All these symptoms can appear from an early age, or they can begin to remind themselves at the age of 5–6 years.
Symptoms (signs)
Clinical picture and diagnosis. • During chronic mitral regurgitation, three periods are conventionally distinguished: compensation, pulmonary venous hypertension and right ventricular failure. • Complaints •• During the compensation period, an asymptomatic course can be observed for several years •• When clinical symptoms appear in patients, the most common complaints are shortness of breath (98%), fatigue (87%), hemoptysis (15%) •• With severe regurgitation there are symptoms of compression of the recurrent laryngeal nerve by the enlarged left atrium (the most common of them is Ortner's syndrome - hoarseness of voice), and during the period of right ventricular failure - by the pulmonary trunk •• In patients in the third stage - symptoms of stagnation in the systemic circulation (edema, enlarged liver, Plesch's sign, swelling of the jugular veins).
• Peripheral symptoms are due to small output syndrome - see Aortic valve insufficiency. • Valve symptoms •• Mesosystolic click occurs with mitral valve prolapse, separation of chords or papillary muscle •• Weakening of the first tone •• Systolic murmur over the apex of various timbres, carried out to Botkin’s point and the left axillary region; its intensity depends on the volume of regurgitation •• The most specific sign of a mitral regurgitation murmur is intensification or appearance during tests that reduce the volume of the left ventricle (Valsalva maneuver, orthostatic test), or in a clinostatic position when turning to the left side due to the closer location of the apex of the heart to the chest •• Systolic flutter over the apical region - with high velocity (usually a thin jet) of regurgitation •• Coombs' murmur occurs due to relative stenosis of the mitral valve due to an increased volume of blood expelled from the left atrium.
• Symptoms associated with enlargement of the chambers of the heart • Increase in the boundaries of relative dullness to the left, up and to the right (with dilatation of the right sections) • Popov's symptom - different degrees of filling of the pulse in the radial arteries. • Symptoms of the underlying disease (rheumatism, Marfan syndrome, cardiomyopathy).
Diagnostics
The more methods were used to diagnose congenital heart disease code according to ICD 10, the more accurate and detailed the picture of the disease will be visible.
The following methods are used for diagnosis:
- Electrocardiogram. This method gives excellent results, even in the initial stages of pathology development. Based on the interpretation of the cardiogram results, the cardiologist can accurately determine the intensity of the development of the disease and its danger to the child’s life.
- X-ray. When conducting an X-ray examination in 3 projections, the condition of the lungs and the entire respiratory system can be determined.
- Echocardiography. Allows the cardiologist to obtain the most accurate picture of the patient’s condition.
- Angiography or catheterization. These techniques are more difficult to perform, but they allow you to determine the pressure in the lungs, as well as accurately determine in which direction the blood flow is directed (from the right atrium to the left or vice versa).
All of the above diagnostic methods are used in combination.
Only in this case can an accurate diagnosis be established and an effective course of treatment be chosen. Regardless of whether the defect is congenital or acquired, you must be attentive to your health and the health of your loved ones; if one or more signs appear, immediately contact a pediatrician and cardiologist. Be healthy!
Forecast
The prognosis for a patient with mitral valve prolapse depends on the course of the pathological process, its severity and the degree of regurgitation. The main role is played by timely diagnosis and compliance with specialist recommendations.
Mild cases are often not even detected and are not life-threatening. It is enough for the patient to be regularly examined and observed by a doctor. More severe forms have a less favorable prognosis. They are characterized by rapid development of complications and irreversible changes. The degree of recovery depends on the effectiveness of treatment and timely elimination of the causative factor.
Clinical picture and treatment for mitral valve prolapse
Mitral valve prolapse (ICD-10 code - 134.
1) is a common pathology of the cardiovascular system, in which the heart valve leaflets are forced into the left atrial cavity during systole.
According to cardiologists, this pathology does not pose a particular danger to the patient’s life, but in the presence of concomitant diseases it may have an unfavorable prognosis.
This condition is also known as Barlow syndrome or click and noise syndrome. This pathology was first described in 1887 as a previously unknown phenomenon of clicking during systole.
And only from 1963 to 1968 an angiographic study was carried out, which explained the nature of the origin of the auscultatory phenomenon that arose as a result of sagging of the heart valves during ventricular contraction.
Etiology and pathogenesis
To understand what prolapse is and the mechanism of development of this pathology, it is necessary to understand the normal functioning of the heart. From the pulmonary circulation, represented by the vessels of the lungs, blood enriched with oxygen enters the left atrium.
From here, through the mitral valve, which consists of two leaflets, it follows into the left ventricle of the heart and is pushed into the mouth of the aorta, from where it enters the systemic circulation.
The blood flows back to the heart, giving oxygen to the tissues and taking carbon dioxide instead, but this time it enters the right atrium and right ventricle (pulmonary circulation).
Physiologically, the blood is completely squeezed out of the left atrium during systole, and the mitral valve prevents its return. When the mitral valve prolapses, some of the blood is re-thrown into the atrium. This process is called regurgitation. It has been proven that if the deflection of the mitral valve leaflets does not exceed 3 mm, then there is no re-reflux of blood.
Reasons for development
As practice shows, the diagnosis of mitral valve prolapse is diagnosed more often in children and adolescents than in adult patients. The incidence of MVP is influenced by diseases of the nervous system, connective tissue, and congenital malformations of the cardiovascular system. This pathology can be detected in patients of different age categories, but most often these are schoolchildren over the age of 7 years.
Based on the type of development, mitral valve prolapse is divided into primary and secondary. Primary (idiopathic) MVP develops as a result of congenital pathology.
The cause of such anomalies can be viral diseases, gestosis of pregnancy, and an unfavorable environmental situation.
As a result of exposure of a pregnant woman to unfavorable factors, the fetus develops connective tissue dysplasia, which leads to prolapse of the mitral valve leaflets.
https://www.youtube.com/watch?v=pJjA8B2O7e4
Secondary (acquired) mitral valve prolapse develops as a complication of other systemic diseases. These may be systemic lupus erythematosus, congestive heart failure, myocardial infarction, coronary heart disease, rheumatoid arthritis. The frequency of development of secondary MVP is also significantly influenced by the initial inferiority of connective tissue.
Clinical manifestations
The clinical picture of mitral valve prolapse (ICD-10 code - 134.1) can differ significantly in each patient, it all depends on the degree of valve insufficiency.
With mitral valve prolapse, there are no specific symptoms of the disease, but there are a number of clinical signs that allow one to suspect mitral valve insufficiency:
- frequent headaches that appear in the morning;
- disruptions in the functioning of the heart, manifested by arrhythmia;
- causeless feeling of anxiety and fear;
- pain in the left side of the chest in the area of the heart, which is not eliminated by Nitroglycerin;
- feeling of lack of air;
- increased sweating;
- prolonged low-grade fever not associated with inflammatory diseases;
- weakness and malaise.
Separately, it is necessary to highlight MVP in pregnant women, which most often has a favorable prognosis for both the pregnant woman and the fetus. Drug therapy is necessary in exceptional cases when there is a risk of developing fetal hypoxia. Mitral valve prolapse in pregnant women is characterized by the following symptoms:
- vegetative-vascular disorders (arrhythmia, chills, profuse sweating);
- vascular dysfunctions (swelling, numbness and low temperature of the extremities);
- psychopathic disorders (frequent mood swings, feelings of anxiety and fear).
Collapse may be common in pregnant women with similar symptoms. Collapse is a sharp decrease in blood pressure until complete loss of consciousness. In such a condition it is necessary:
- Lay the patient down and unfasten the clothes on the chest, ensuring free access to fresh air.
- Raise your legs higher than your body to increase blood flow to the brain.
- Wet your face with cold water.
- Bring ammonia on cotton wool to your nose.
Collapse should be the reason for an unscheduled visit to the leading doctor.
Features of diagnosis and treatment
Mitral valve prolapse grade 2, like grade 1, is most often diagnosed accidentally during a general medical examination. The first step in diagnosing the disease is collecting anamnesis, symptoms and an objective examination of the patient.
During auscultation, an experienced cardiologist will immediately suspect MVP by the presence of characteristic clicks. Their intensity usually increases if the patient is in a horizontal position, while in a vertical position there is a decrease in the intensity of the noise.
If necessary, additionally prescribe:
- Echocardiography, which will show the mitral valve, prolapse of the valves into the atrium cavity and pathological blood flows.
- ECG – disturbance of cardiac conduction, changes in the final part of the ventricular complex.
- FKG.
- Ro-graphy of the chest cavity and heart.
It is also necessary to undergo a series of laboratory tests, which are based on studying the composition of blood and urine. It is imperative to do a detailed blood test and examine its biochemical composition.
Mitral valve prolapse is differentiated from other diseases in the following clinical circumstances:
- acquired or congenital heart defects;
- other cardiopathy, which is accompanied by reflux of blood into the left atrium;
- the presence of genetic pathologies;
- infective endocarditis;
- heart failure.
Treatment of mitral valve prolapse directly depends on the degree of valve insufficiency and the individual characteristics of the patient.
To reduce symptoms that bother patients, the following is indicated:
- for rapid heartbeat - B-blockers, which normalize the heart rate (Atenolol, Propranolol);
- vitamins of groups B and PP, which not only normalize the functioning of the nervous system, but also have a positive effect on the functioning of the heart (Neurovitan, Neurobex);
- adaptogenic drugs that also have a positive effect on the functioning of the cardiac system and the whole body (ginseng tinctures, Eleutherococcus tinctures);
- at 1-2 degrees of PMC - drugs containing magnesium (Magne B6).
In the third degree of insufficiency (the mitral valve bends up to 10 mm or more), surgical intervention is indicated, which is performed to sew in the valve leaflets or replace it with prosthetics.
The decision to perform surgical intervention is made by a cardiologist in cases where there is no positive dynamics of the disease, as well as in the serious condition of the patient.
When carrying out drug treatment of mitral valve prolapse, it is necessary to change the patient’s lifestyle.
First of all, he must give up bad habits (drinking alcohol, smoking, taking drugs).
You should also switch to a healthy balanced diet, engage in feasible sports, walk more, avoid stressful situations, and also control the correct balance of work and rest.
Patient prognosis
For the patient, the diagnosis of “mitral valve prolapse” (ICD-10 code - 134.1) is in most cases favorable, but at an advanced stage or in the absence of adequate treatment, a number of complications can arise:
- neurological disorders that can lead to cerebral infarction;
- mitral valve insufficiency caused by reverse blood flow;
- heart failure;
- infectious myocarditis;
- arrhythmias.
If you are diagnosed with MVP, do not panic; this pathology is highly treatable. Only therapy must be carried out under the supervision of a highly qualified cardiologist, who will individually select treatment and provide a detailed rehabilitation plan. And also undergo regular preventive examinations at least once a year.
Finding the nearest clinic Find the clinic closest to your home in your city
Source: https://asosudy.ru/serdce/mitralnuj-klapan