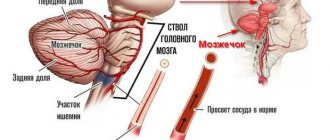
It is difficult to dispute the fact that ischemic stroke is the most common cardiovascular pathology. According to statistics, about 6,000,000 strokes occur every year in the world. They occur several times more often than myocardial infarction. The risk of its development directly depends on age. The older a person is, the more likely he is to have a cerebral infarction. With each subsequent decade it doubles. Is it really that bad? Is there any way to protect your health?
Development mechanism
Acute cerebrovascular accident is formed as a result of the influence of one or more key factors.
Among them:
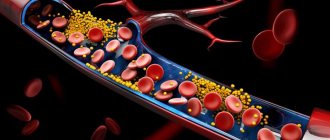
- Atherosclerosis. The scourge of modern man. The disease occurs in two forms. Formation of cholesterol plaques on the walls of arteries. The result of excess circulation of fatty compounds in the bloodstream.
It occurs frequently, the process is determined by nutrition, lifestyle, and to a large extent also by metabolic characteristics. Which are inherited from parents and ancestors going back generations.
Correction is carried out at an early stage, then it is more difficult to cope with the problem.
The second possible form is spontaneous vascular stenosis, arterial spasm.
As a rule, this is the result of an irrepressible craving for smoking and consumption of large amounts of tobacco. Treatment in such a situation comes down to giving up the bad habit and using drugs to normalize microcirculation.
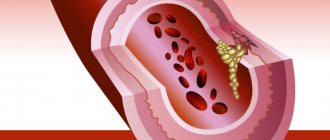
- Thrombosis. The essence remains the same. The lumen of the vessel supplying the brain becomes insufficiently wide. However, the reason is different. If in the first case a plaque forms, which grows gradually, in this situation the cause of the disorder is a blood clot. A blood clot containing fibrin.
Depending on the size, the formation can block part of the artery or completely block it. In the latter case, a hemorrhagic form of cerebral infarction (stroke) may develop. When the vessel ruptures, hemorrhages begin, and a hematoma occurs.
This type of condition is much more dangerous than ischemic. When tissue death occurs as a result of insufficient nutrition.
- Blocking the supply of oxygen to the brain. As a rule, it is observed in cases of poisoning with toxic substances: hydrocyanic acid vapor, carbon monoxide, and under the influence of neurotoxins. All body systems suffer. Often the patient dies before a heart attack occurs. But not always.
Then the process moves progressively. Violation of trophism (nutrition) as a result of small lumen of blood vessels leads to cerebral ischemia.
How pronounced depends on what the hemodynamics (blood flow) is at the moment. The more blood flows in, the less noticeable the abnormalities are. In case of total blockage, rupture of the vessel and heavy bleeding cannot be avoided.
After a disorder of cerebral nutrition and breathing, a period of pronounced clinical symptoms begins. Depending on which area is most affected, focal symptoms develop.
There is always a neurological deficit: problems with speech, vision, hearing or intelligence. The correction is carried out as part of rehabilitation; this process lasts for years.
The end result is permanent disruption of brain activity or death of the patient. A stroke never goes away without consequences. “Correcting” the results of the violation will take a long time and persistently, not always quite successfully.
General characteristics, stages of pathology
The origin of cerebral myocardial infarction is associated with cerebral circulatory failure. There is an increase in such disorders with age, so the pathology is more common in older people.
Cerebral myocardial infarction presents similarly to a stroke, as heart failure leads to neurological problems. In this case, the neurological signs of pathology are more pronounced than typical symptoms of a heart attack.
There are three degrees of severity of the pathology. Each has certain features:
- Mild degree. In this case, the patient may not notice the onset of the disease. Typically, heaviness appears in the eye area, visual acuity decreases, and pulsation is observed in the temples.
- Moderate severity of the pathology is accompanied by speech difficulties; the patient has difficulty moving his tongue. This stage is characterized by a staggering gait, which is called drunken.
- Severe disturbances cause clouding of consciousness, the patient is in prostration, looks in one place and does not notice anything around. Even at this stage, there is no pain in the heart area, so it is difficult to suspect a heart attack.
The infarction is usually localized to the left ventricular type. In this case, congestive wet wheezing may appear in the lungs. They can cause suffocation and subsequent pulmonary edema.
If blood circulation is disrupted according to the right ventricular type, then the heart expands to the right, the liver enlarges, and the lower extremities swell.
The cerebral form of myocardial infarction is diagnosed in 1-1.5% of cases.
Classification
Cerebral infarction and stroke are no different (they are equivalent concepts), therefore the classification will be the same. The pathological process can be divided on two grounds.
The first and most applicable in clinical practice is the type of disorder, its fundamental features.
- Ischemic type. Occurs especially often. The essence is a malnutrition of a particular area without signs of vascular destruction. However, this does not mean at all that ischemic cerebral infarction is a harmless phenomenon.
Depending on the area of the lesion, it can be fatal or make the patient disabled, eking out a vegetative existence.
- Hemorrhagic form. Mainly, it develops in people prone to the formation of blood clots in the body or in people with hypertension. The basis is the same: acute nutritional disorder of cerebral structures.
The difference is different. The integrity of the blocked artery is compromised. It ruptures and profuse bleeding begins. This is deadly.
An additional damaging factor arises. The space in the skull is extremely limited. Large volumes of liquid connective tissue lead to compression of the brain as a result of the formation of a hematoma.
If it is not eliminated promptly, the risk of death increases significantly.
The second way to classify cerebral infarction is to determine the extent of the lesion.
Then there are three more forms:
- Finely focal. As the name suggests, one area of nerve tissue is affected, usually small. Symptoms are limited to manifestations of local neurological deficit.
Any one area of higher nervous activity is affected. Most often not completely. For example, speech in certain aspects, vision and others.
A special case is lacunar cerebral infarction. When many small dead areas form throughout the cerebral structures.
- Intermediate form. Accompanied by the same lesion at the level of a small lesion, but the area of deviation is larger. Structural changes are more dangerous, the clinical picture is broader.
This is the main type of cerebral infarction, and doctors and patients encounter it most often.
- Finally, the extensive form. The lesion affects significant areas of cerebral structures.
In the vast majority of cases, the patient dies or remains deeply disabled with severe neurological deficits. There is no talk of any legal capacity.
There are isolated cases of more or less high-quality recovery after such massive damage to nerve tissue. At the level of statistical error.
Both classifications are used to code the diagnosis and more thoroughly describe the essence of the pathological process.
This allows you to plan treatment tactics in each specific case, based on known factors.
Symptoms
The clinical picture depends on the extent of the lesion and the location of the cerebral infarction.
There are two large groups of manifestations. The first is general. The second is local or local.
If we talk about generalized points:
- Inability to properly navigate in space. The person takes a forced position lying on his side. This is the only way to partially correct the negative feeling.
- Headache. Usually extremely intense. Pulsating. But the location of the discomfort does not always correspond to the area where tissue death occurred. The symptom does not go away on its own until the acute phase of the pathological process is over or medical care follows.
- Impaired coordination of movements. Normally, the cerebellum “cuts off” excess activity. Therefore, everyone moves plastically and changes the nature of their motor skills depending on the situation.
With the development of a cerebral infarction, cerebral tissues receive chaotic signals. Simply put, the body has no time to solve problems such as ensuring coordination of movements. When the cerebellum itself is damaged, the symptom is even more pronounced.
- Nausea, vomiting. Usually at the beginning of an emergency. This can be dangerous, especially if the patient is unconscious.
- Fainting. These are even more alarming symptoms. Because with almost a 100% guarantee they indicate critical violations that progress rapidly.
These symptoms are present in every patient without exception. Depending on the severity, variations are possible.
Focal manifestations are more variable. In total, several functional areas of cerebral structures are distinguished.
Frontal lobes
Defeat leads to behavioral and intellectual impairments. To be more specific:
- Foolishness, frivolity, inappropriate cheerfulness or, on the contrary, a depressive mood. Inappropriate reactions to stimuli. In this case, the patient himself is not aware of the problem. Sudden changes in emotional state are possible.
- Paralysis, paresis. One-sided.
- Intellectual deficit. The patient cannot perform complex actions, the speed of thinking decreases. And in an advanced case, a critical defect is discovered when a person becomes helpless.
- Epileptic episodes with loss of consciousness and convulsions.
- Loss of ability to speak.
Temporal lobes
They are responsible for the perception of verbal information, partly memory, and some other aspects.
- Hearing loss on one or both sides. Happens frequently.
- Hallucinations. Like the voices in your head. At the same time, the patient clearly realizes the illusory nature of such a manifestation.
- Aphasia. Loss of speech function.
- Epileptic seizures. As with damage to the frontal lobe. They may also be longer.
- Memory problems. Focal symptoms of such localization are characterized by various amnesias. This is a hallmark of damage to the temporal part of the brain.
Parietal lobes
They control tactile sensations, as well as some intellectual functions and feelings.
- Loss of smell on one side.
- Inability to identify an object by touch with eyes closed. Even a well-known one.
- In especially severe cases, the patient does not perceive his own body as a single whole. For example, an arm or some segments of it may appear to be missing.
- Loss of ability to handle numbers and read.
Occipital lobes
The visual analyzer is located here. Higher nervous activity is the main “guarantor” of the ability to see. The eye itself cannot process data.
Symptoms corresponding to:
- Mice in sight. Dots flying back and forth. In large quantities.
- Blackouts, scotomas. They look like black spots around the periphery of the picture. Closing part of the review.
- Problems with focusing on the desired point. Double vision.
- A sharp drop in visual acuity.
- Complete loss of ability to see. Usually, even with a large area of damage, it is possible to restore at least part of the function through rehabilitation.
- Impaired perception of the size of an object, distances to it.
Extrapyramidal system
Represented by the cerebellum. Mostly problems arise with motor activity. Motor skills are uncoordinated, the patient cannot normally navigate in space due to severe dizziness.
Limbic system
When this area is damaged, a person loses the ability to learn, and there may be a complete loss of sense of smell.
Brain stem
The defeat is almost always fatal. There are problems with breathing and cardiac activity. Thermoregulation is disrupted. Even minor dysfunctions in this area often result in the death of a person.
Key symptoms are assessed by doctors during the initial examination. This allows us to better understand the nature of the violation.
A cerebral infarction is not different from a stroke in this aspect; the processes are also identical in other respects.
How to treat
After the initial symptoms of ischemic stroke appear, treatment should begin within the first 6 hours. During this time, there is no time for tissue necrosis to form, so the chances of complete recovery are higher. Complex treatment is used:
- Basic therapy is prescribed to maintain the vital functions of the body - control of breathing and cardiac function, thermometry, reduction of cerebral edema, measures to prevent bedsores, congestive pneumonia, and genitourinary tract infections.
- Specific therapy. The blood clot is dissolved using special medications. To curb the growth of blood clots and prevent complications, treatment with anticoagulants is prescribed. Neuroprotectors are prescribed to restore damaged neurons.
Treatment after the causes of stroke have been addressed is aimed at eliminating neurological symptoms and helping to form new neural connections. For this purpose, the patient is prescribed amino acids, nootropic drugs, piracetam, and a course of therapeutic massage or physical exercise is prescribed.
Important information: What are the prognosis for recovery after ischemic stroke of the brain stem?
In some cases, ischemic stroke can be treated surgically. The operation is prescribed in order to:
- remove cholesterol plaque from the carotid artery;
- increase the lumen of blood vessels;
- dissolve the clot with medicine that is dripped through a catheter inserted into the affected vessel.
Therapy can only follow diagnosis, and only a doctor can establish an accurate diagnosis. For this reason, the sooner the patient gets to a medical facility, the faster the doctor will conduct the necessary examination and tell you how to treat and restore the patient, which will increase the chances of returning to a full lifestyle.
Causes
Development factors are standard and almost always repeated:
- Atherosclerosis. It has already been said about it. Blockage of blood vessels with cholesterol plaques or narrowing of the arteries, impaired blood flow and, as a result, acute death of nerve tissue.
- Toxic damage accompanied by a disorder of cellular respiration. It is relatively rare. But this is also possible.
- Thrombosis. Blockage of a vessel by a blood clot.
- A jump in blood pressure. Accompanied by critical overload and often rupture of the blood supply structure. It is considered one of the most common reasons. Almost always adjacent to atherosclerosis.
- Fragility, insufficient elasticity of the walls of blood vessels. For example, against the background of diabetes or other disorders.
There are a huge number of risk factors: obesity, smoking, alcohol consumption, insufficient or excessive physical activity. And others.
A specialist in neurology must understand the entire array. It is also possible to attract a doctor whose field of activity is in the field of heart and vascular diseases.
First aid
You need to act quickly even if you suspect a cerebral infarction.
The algorithm is simple:
- Call an ambulance. There is no way to help on your own.
- Make the patient sit down. Turn your head to the side. Raise your legs a little and place them on a bolster. This will allow you to adjust hemodynamics. And changing the position of the neck will prevent choking on vomit in the event of loss of consciousness.
- It is important that the patient calms down. Emotional reactions will only make things worse. You can't move.
- Open a window or window to ensure normal ventilation of the room.
- Giving any drugs is prohibited. Because the condition may worsen.
- Eating and drinking are also prohibited. Possible fainting and loss of stomach contents. Is it dangerous.
- It is necessary to constantly monitor blood pressure, heart rate, and breathing.
Upon arrival of the ambulance, report the victim's condition briefly and clearly. If possible, help with transportation and accompany the person to the hospital.
Diagnostics
In an acute condition, there is no time for a full examination. A visual assessment, routine neurological examination, testing of basic reflexes, and a brief questioning of the patient if he is conscious are necessary.
As a rule, everything is obvious. After providing first aid and stabilizing the situation, you can move on to searching for the causes of the pathological process.
The list of events is approximately as follows:
- Measures blood pressure and heart rate over 24 hours. Daily monitoring.
- Blood tests: general, biochemical, sugar.
- Urine examination.
- ECG and ECHO. Assessment of the functioning of the heart and blood vessels.
- Dopplerography of the arteries of the brain and neck. Duplex scanning.
- If necessary, a lumbar puncture is performed. To collect cerebrospinal fluid and examine it for blood.
- Electroencephalography. Detecting brain activity in specific areas.
If necessary, the list is expanded.
Everything you need to know about cerebral infarction
Cerebral infarction is a life-threatening condition also known as ischemic stroke. It develops as a result of an acute circulatory disorder, in which blood either flows poorly to certain parts of the brain or stops flowing altogether. The danger of the disease is that if the situation is not corrected within 7 minutes, then irreversible changes occur in the affected parts. The consequences can be very different.
In most cases, untimely assistance to a patient leads to his death. The gray matter that forms the cerebral cortex is the most sensitive to oxygen starvation.
But it is this part that is responsible for performing the most complex functions in the body.
- Atherosclerosis. Blocked blood vessels combined with high blood pressure can lead to a stroke.
- Damage to the carotid or vertebral artery. This cause is diagnosed in half of all cases of brain disease.
- Surgery on the heart or blood vessels.
Treatment
Therapy is strictly in a hospital setting. A group of medications is prescribed:
- Antiplatelet agents for ischemic lesions. Aspirin and its analogues. Related, but more powerful remedies based on heparitis and other substances are possible. Pentoxifylline. Restore blood flow and nutrition.
- Nootropics. Glycine, Phenibut. Accelerate regeneration.
- Cerebrovascular. Piracetam. Actovegin. To stabilize the supply of nerve fibers with necessary substances.
- Antihypertensive. If there is an increase in blood pressure. Beta blockers (Metoprolol), calcium antagonists (Diltiazem), diuretics are mandatory (Furosemide, if necessary - Mannitol). To reduce the load on the brain and prevent swelling.
The hemorrhagic form requires removal of the hematoma. Promptly.
In the future, everything is decided by rehabilitation and its quality. Recovery takes from 12 to 24 months. The most active reorientation of the brain occurs in the first year. Then the results are not so noticeable.
Read more about rehabilitation after a stroke in this article.
Lifestyle correction is indicated: quitting smoking, alcohol, limiting salt (up to 6 grams), sugar, eliminating fatty foods from the diet. Also optimizing physical activity.
Recovery
Motor functions of the limbs are corrected by special physical exercises, massage, and acupuncture. Exercises for recovery after a heart attack are conducted on simulators under the supervision of an instructor.
Speech is corrected by a speech therapist in individual lessons. Special devices are used to restore swallowing functions, which activate the work of the laryngeal and pharyngeal tissues and muscles.
The victim must drink aspirin and take statins throughout his life. To restore brain activity, Tanakan, Cavinton, Bilobil are recommended.
A psychotherapist will help you overcome psychological barriers. It will take several sessions. Any experiences or stress are dangerous for the patient. He should be surrounded by care and support from family and friends.
Consequences
The main consequence of cerebral infarction is persistent focal neurological deficit. With the right amount of effort, it is possible to carry out a correction and get rid of the problem. Mostly.
There is also a high probability of death and severe disability. Cerebral infarction caused by thrombosis of the cerebral arteries or other causes almost always recurs without correction.
Each next episode is harder than the previous one. The risks of death are becoming higher. Therefore, therapy must be comprehensive.
Complications
Negative consequences are especially typical for elderly patients and include the development of the following diseases:
- pneumonia;
- development of bleeding stomach ulcers;
- heart problems (heart attacks, irregular heartbeat, etc.);
- paralysis or decreased muscle mobility;
- dysarthria;
- dysphagia;
- motor, sensory or amnestic aphasia;
- memory impairment;
- problems with thinking;
- incontinence;
- cerebral edema;
- loss or deterioration of vision;
- epilepsy;
- recurrent stroke;
- bedsores;
- depression;
- thrombosis;
- depression.