Rating: No rating
Unfortunately, central nervous system disorders in newborns are not uncommon. Up to 50% of all children are exposed to this disorder to one degree or another.
Today we will talk about perinatal damage to the central nervous system (CNS) in newborns, we will tell you what symptoms this disease is characterized by, what methods exist for diagnosing and treating damage to the central nervous system, and we will also understand what the consequences of this disease may be.
Causes of central nervous system damage in children
The causes of this disease during pregnancy may be:
- hypoxia in the fetus;
- somatic diseases in the mother;
- metabolic disorder;
- poor nutrition;
- unfavorable environmental conditions;
- mother's age is over 35 or less than 18 years;
- acute infectious diseases;
- pathological course of pregnancy;
- the influence of toxins on the body of the expectant mother (smoking, drinking alcohol and drugs).
In some cases, the causes of damage to the central nervous system are injuries and fetal hypoxia during the birth process. Any lesions of the central nervous system can be divided into two types.
Organic damage to the central nervous system
This diagnosis occurs among people of different ages. Organic damage to the central nervous system in both children and adults is characterized by pathological changes in the brain.
Perinatal CNS damage
Diagnosed in newborns. Depending on the period in which this lesion occurred, the following types are divided:
- antenatal (the period of intrauterine development from 28 weeks until birth);
- intrapartum (damage occurs directly during childbirth);
- neonatal (the lesion is diagnosed in the first week of life).
Depending on the causes, this disease is divided into several types.
Hypoxic damage to the central nervous system
Hypoxic, or hypoxic-ischemic, damage to the central nervous system in newborns is characterized by oxygen starvation for one reason or another. It appears in the womb or due to asphyxia during childbirth.
Traumatic
Traumatic, or residual, damage to the central nervous system in children represents residual effects after injuries and structural changes in the brain.
It is very important to diagnose this pathology as early as possible, since brain cells in infants have the ability to recover. Accordingly, terrible consequences can be avoided.
Symptoms of Brain Damage
In the first hours and days after birth, signs of disorders of the cardiovascular system come to the fore, and symptoms of hypoxic damage to the central nervous system begin to manifest themselves later.
If brain damage is caused by pregnancy pathology, the baby may be lethargic and have weakened or completely absent reflexes that a healthy newborn should have. If there is a pathology that occurs during childbirth, the baby does not immediately begin to breathe after birth, the skin has a bluish tint, and the respiratory rate is lower than normal. And in the same way, physiological reflexes will be reduced - based on these signs, oxygen starvation can be suspected.
At an older age, brain hypoxia, if it was not cured in time, manifests itself as a slowdown in psycho-emotional development, up to severe forms of dementia, and motor disorders. In this case, the presence of organic pathology is possible - brain cysts, hydrocephalus (especially often occurs with intrauterine infections). Severe brain hypoxia can be fatal.
Diagnosis of central nervous system lesions in children
An experienced doctor can diagnose central nervous system damage with one look at the child. But to make a final diagnosis, the following research methods are used:
- various types of tomography;
- electroencephalogram;
- Ultrasound of the brain with Dopplerography of blood vessels;
- X-ray of the skull and spine.
These studies are easy to perform even in the youngest patients. Moreover, an open large fontanel in newborns allows one to perform ultrasound of the brain repeatedly and monitor its condition over time.
Also, one of the diagnostic methods is collecting anamnesis and monitoring the symptoms of the disease.
Symptoms of the disease
According to its course, perinatal damage to the central nervous system can be divided into three stages, each of which is characterized by its own symptoms.
Acute period
This period lasts up to one month and is characterized by the following symptoms:
- CNS depression syndrome (hypodynamia, lethargy, decreased reflexes, muscle hypotension);
- CNS hyperexcitability syndrome (restless and often superficial sleep, trembling chin, muscle hypertonicity, convulsions) is less common.
Early recovery period
This period lasts for the 2nd and 3rd months and is characterized by a decrease in the symptoms of the acute period. At the same time, the location of the lesion becomes obvious. This phenomenon is characterized by the following symptoms:
- divergence of the sutures of the skull, increase in head circumference, swelling of the fontanelle;
- impairment of motor activity;
- thermoregulation disorder, marbled skin color, disruption of the gastrointestinal tract.
Late recovery period
The period lasts up to 1 year in children born at term, and up to 2 years in premature children. During this period, static functions and muscle tone are restored. The recovery process depends on the degree of damage during the perinatal period.
Period of residual effects
In most cases, during this period there is a complete restoration of all neurological functions . At the same time, every fifth child experiences serious consequences of neurological dysfunction during this period.
Hypoxic-ischemic damage to the central nervous system
Perinatal lesions of the central nervous system (PPCNS) are a group of pathologies in which the normal functioning of the spinal cord in newborns is disrupted.
The process can develop for various reasons, one of them is hypoxia, that is, oxygen starvation. The perinatal period includes the last trimester of pregnancy, childbirth and the first week of the baby's life.
During this time, the body experiences stress during the transition to pulmonary breathing, as well as during adaptation to various environmental factors, therefore hypoxic-ischemic damage to the central nervous system is a common diagnosis.
10% of newborns experience oxygen deficiency to varying degrees, especially premature ones. The condition requires urgent medical attention, but in 80% of cases it has a favorable outcome and does not in any way affect the further development of the child.
Mechanism of development of hypoxia
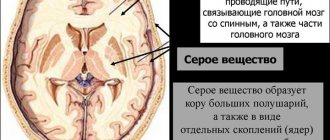
The central nervous system is the brain and spinal cord. These structures are able to function normally only with a sufficient supply of oxygen, which is carried by the blood.
Infants and young children have a significantly higher oxygen requirement than adults, and oxygen deficiency can cause serious delays in physical and mental development.
Damage to the central nervous system of ischemic origin is associated with insufficient blood supply to brain tissue, and therefore there is a gradual death of nerve cells.
Hypoxia is a lack of oxygen in tissues. With perinatal damage, this occurs during pregnancy, during childbirth and in the first days of the child’s life. The condition is reversible, since regeneration processes occur faster at a younger age.
Over time, the harmful effects of oxygen starvation can be neutralized and nerve conduction restored. Ischemia is a more dangerous condition.
This term implies a complete cessation of oxygen supply to cells, which leads to their rapid necrosis.
Causes of central nervous system damage
The main cause of the disease is ischemic hypoxia, that is, damage to the cells of the nervous system due to their insufficient blood supply. The type of violation depends on a number of factors, including the duration of oxygen starvation.
Thus, during acute hypoxia, the stem parts and subcortical structures are damaged, and during prolonged oxygen deficiency, the cerebral cortex is damaged.
The process develops during intrauterine development and immediately after birth, and its causes can be the following factors:
We recommend reading the article: Diseases of the blood vessels of the head
- on the maternal side: various circulatory disorders in the uterus, heavy bleeding, various pathologies of placental development;
- during pregnancy: bad habits, systemic use of certain groups of drugs;
- during childbirth: umbilical cord entanglement, massive blood loss in the mother, low blood pressure and low pulse in the child;
- in the first days of life: heart defects and congenital diseases of the respiratory system, DIC syndrome and other pathologies.
Various pathologies of the cardiovascular system are a trigger for the development of hypoxic-ischemic damage to the central nervous system. A deficiency of oxygen in arterial blood causes a lack of oxygen in the nervous tissue. This is how necrosis (death) of some nerve cells or their groups occurs.
In this condition, a decrease in blood pressure provokes a worsening of the situation and can lead to chronicity of the process and irreversible changes. Due to a slowdown in metabolism, acidosis (oxidation) of cells occurs, which causes swelling.
Ischemic changes often include increased intracranial pressure, as well as pathologies of internal organs (lungs, kidneys, liver).
REFERENCE! Ischemic-hypoxic damage to the central nervous system refers to irreversible changes in brain tissue caused by insufficient blood supply. Less severe disorders are more often classified as hypoxic-ischemic encephalopathy, but the terms can be used interchangeably.
Signs
The clinical picture of ischemic syndrome is individual for each patient. It manifests itself depending on the degree and duration of hypoxia. It is worth noting that the prognosis in childhood is favorable in most cases. The central nervous system has regenerative properties, so complications develop only in the last stages.
The diagnosis can be made already in the first minutes of life, especially if the disease manifests itself in a severe form
The severity of the patient's condition is assessed using the Apgar scale. It includes a number of indicators, including pulse and respiration, skin condition, and the severity of reflexes. Thus, brain damage of hypoxic origin can be diagnosed immediately after birth. There are 3 main degrees of the disease, the third of which is the most dangerous.
1st degree
With hypoxic damage to the central nervous system of the first degree, the symptoms are mild. The child’s general condition is assessed at 6–7 points (the optimal result is considered to be 7–10 points). The clinical picture includes the following signs:
- pale, bluish skin;
- deterioration of muscle tone, tremor;
- restless sleep;
- activation or deterioration of reflexes.
First degree injuries do not pose a danger to the patient. Already during the first week of life, all indicators return to normal, and then the child develops on par with peers.
2nd degree
The second degree of brain damage most often occurs during hypoxia both during pregnancy and childbirth. According to the Apgar scale, the child's condition can be assessed as 5 points. The pathological process is manifested by the following symptoms:
- lack of reflexes;
- increase or decrease in muscle tone;
- pronounced cyanosis of the skin and mucous membranes;
- increased intracranial pressure - this indicator continues to increase, manifested by bulging fontanelles, sleep disorders, involuntary muscle movements;
- autonomic disorders, including arrhythmias, slow heart rate, apnea (stopping breathing), problems with the functioning of the digestive tract.
IMPORTANT! In the first days of a child’s life, it is important to monitor intracranial pressure indicators. With timely treatment, the condition can improve by the end of the first week of life; if it is not treated, the disease progresses.
3rd degree
Third degree damage to the central nervous system is a consequence of gestosis in the second half of pregnancy. The child's condition is complicated by abnormal birth.
A newborn needs resuscitation measures, since he may have no respiratory activity, and pathologies of the cardiovascular system are pronounced.
There are no reflexes, including swallowing, so natural feeding is impossible. Often such patients are diagnosed with renal and liver failure, DIC syndrome (blood clotting pathology).
Stages of disease development and prognosis
There are several stages in the development of the disease. It has been established that treatment is most effective in the first week of a child’s life – it is during this time that the most intensive restoration of functions occurs. Each stage is characterized by a specific clinical picture, and their severity indicates the severity of the pathology.
Acute period
The acute period is considered to be the period from the birth of the child until the first month of life. Regardless of the complexity of his condition, it is better to carry out therapeutic measures at this time in order to avoid long-term consequences. The clinical picture varies but may include the following syndromes:
- hypertensive-hydrocephalic – increased intracranial pressure due to impaired outflow of fluid from the ventricles of the brain;
- convulsive – involuntary muscle contractions;
- vegetative-visceral - the child develops a marbled skin tone, as well as various disorders of the digestive tract, heart and blood vessels;
- apathy – reflexes are slow, muscle tone is reduced;
- increased nervous excitability, which is manifested by an increase or decrease in muscle tone;
- comatose is the most dangerous sign of cerebral hypoxia.
The first improvements should appear within the first week. Treatment is carried out in a hospital, and in severe cases - in the intensive care unit. The main goal is to normalize blood supply to the brain and prevent tissue swelling.
Recovery period
The recovery stage lasts up to a year, in premature babies - up to two years. At first, noticeable improvements appear: reflexes and muscle tone are normalized, tissue cyanosis disappears. However, the disease can occur with exacerbations, especially in the second and third stages.
It is worth remembering that if there is a malnutrition of the brain, a child may experience delays in growth and mental development, but with age these changes will disappear.
At this stage, it is necessary to place emphasis on constant monitoring of the patient, as well as on rehabilitation measures (massage, gymnastics).
Treatment at home is impossible, since the child needs to quickly restore cerebral circulation and be under constant supervision
Outcome of the disease
The patient's further condition can be predicted at one year of age. By this time, differences in growth and development should no longer be noticeable, especially in mild cases. The outcome depends on the timeliness of therapy and the type of disorders caused by hypoxia, and may be as follows:
- complete recovery;
- unfavorable, with progression of the neurological picture;
- disability;
- latent course - symptoms appear with age.
REFERENCE! Even with a favorable outcome, long-term effects such as speech delay, hyperactivity, sleep disturbances and mood swings may persist. In severe cases, hydrocephalus, epilepsy and cerebral palsy may develop.
Diagnostic and treatment methods
Hypoxic-ischemic damage to the central nervous system is detected immediately after birth. At the first stage, a full examination and diagnosis of reflexes is carried out. If brain damage is suspected, further examination includes the following methods:
- neurosonography - ultrasound examination of brain tissue through the fontanelle, possible only in newborns;
- MRI, CT are the most informative ways to determine the state of the central nervous system;
- electroencephalography – diagnostics of brain activity;
- Dopplerography is a study of blood flow activity.
Treatment is selected individually and depends on the stage of the pathology. It is often carried out using conservative methods and involves the use of certain groups of drugs:
- anticonvulsants;
- nootropics – medications to improve blood supply to the brain;
- diuretics to reduce intracranial pressure;
- herbal sedatives (valerian extract) for sleep disorders;
- additional methods according to indications.
During the recovery period, it is useful to attend therapeutic massage sessions and do passive exercises. You may need long-term systematic use of medications to improve cerebral circulation.
Conclusion
Hypoxic-ischemic damage to the central nervous system is a common diagnosis, but it often manifests itself in a mild form.
The pathology occurs due to insufficient blood supply to the brain during the period of intrauterine development of the fetus and during childbirth. The majority of children (up to 80%) who had such disorders at birth are no different from their peers.
However, it is dangerous to underestimate the disease, since it can cause dangerous consequences and nervous disorders.
Source: https://icvtormet.ru/bolezni/gipoksicheski-ishemicheskoe-porazhenie-cns
Treatment of the disease
Important! Only a doctor can conduct the necessary examination and prescribe the correct treatment.
Treatment of moderate to severe central nervous system damage is often carried out in an intensive care setting, often using special equipment to support the functioning of vital organs.
In the acute period of the disease, the following treatment methods are used:
- reducing cerebral edema and maintaining the functioning of internal organs;
- reduction in the frequency of seizures;
- restoration of nervous tissue metabolism;
- restoration of oxygen metabolism in cells.
In the recovery period , in addition to the above methods, the following therapy is used:
- stimulant drugs;
- sedative therapy for increased excitability;
- drugs to improve cerebral circulation;
- massage;
- physiotherapy;
- Exercise therapy.
Subsequently, treatment is carried out up to three times a year under the supervision of a neurologist for several years.
Symptoms and treatment of cerebral ischemia in a child
Hypoxic brain lesions with the development of ischemia are observed in 15-30% of full-term newborns. In premature infants, pathology occurs more often - in 40-60% of cases. Often such disorders are harbingers of cerebral palsy (CP), symptomatic epilepsy, and dementia that occurs against the background of organic damage to brain structures.
The listed diseases that arise in the central nervous system lead to childhood disability and are the main cause of social maladjustment.
Of particular importance is the comprehensive diagnosis of ischemic changes that occur in the brain of newborns.
It is advisable to carry out diagnostic studies of the fetal nervous system during pregnancy starting from the antenatal period.
Manifestations of ischemia in infants
Ischemia of brain structures is a disease that is accompanied in newborns by hypoxia (low oxygen content in tissues) or anoxia (lack of oxygen in tissues), which leads to acute oxygen starvation. In 40% of cases, central nervous system lesions in childhood are associated with perinatal pathology.
Prematurity is the leading factor associated with morphofunctional immaturity of brain structures, which increases the risk of cerebral ischemia in premature infants during premature birth. Due to oxygen starvation, necrosis (tissue death) develops, which leads to focal and diffuse structural changes in the brain matter. Depending on the location and nature of the damage, the following are distinguished:
- Multicystic leukomalacia (diffuse damage to the white matter of hypoxic, ischemic etiology).
- Subcortical (subcortical) leukomalacia.
- Ischemic necrosis (focal or diffuse).
Atrophic changes in brain structures are detected during instrumental diagnostics. When conducting an Echo-EG (echoencephalography) study, in 80% of cases, compactions are observed in the periventricular (near the ventricles) region, in 20% of cases the picture is complemented by the expansion of the ventricles and spaces in which the cerebrospinal fluid is located (ducts, subarachnoid space).
Often (about 18% of cases) ischemia that affects the brain in a child occurs without obvious abnormalities in the structure of the brain matter.
An EEG study (electroencephalography) in premature infants in 73% of cases shows the inconsistent nature of the bioelectrical activity of the brain with a predominance of slow, low-amplitude waves, periodically alternating with short-term regular waves.
In 23% of children, various pathological patterns (sample patterns) of the EEG and waves of an epileptic nature in a general oscillatory rhythm are detected. Rarely (3% of cases) the EEG does not show significant deviations from the norm in children with ischemia occurring in the brain.
Main signs of the disease
Ischemic disease affecting the brain in newborns is accompanied primarily by neurological symptoms.
Assessment of the newborn's condition on the Apgar scale of 2-5 points indicates the presence of intrapartum (during childbirth) asphyxia.
In especially severe cases, a coma and severe depression of the central nervous system may develop, which requires immediate resuscitation measures with connection to a ventilator. Other signs:
- Convulsive syndrome.
- Bulbar disorders. Dysfunction of swallowing and sucking.
- Alternation of muscle hypotonia and muscle hypertonicity of the pyramidal, pyramidal-extrapyramidal type.
- Spastic tetraplegia. Partial or complete paralysis of the limbs.
- Spastic tetraparesis. Weakness of motor activity of all limbs as a result of dysfunction of the nervous system.
- Dystonic episodes (spasmodic contraction of muscles of a constant nature) with a characteristic freezing in the posture of an asymmetrical tonic neck reflex.
- Hyperkinesis (involuntary movements of one or a group of muscles) with athetosis (involuntary twitching) of the hands.
- Muscle rigidity. Stiffness, hardness of muscles.
- Sleep disturbance, frequent crying.
It is worth paying attention to abnormal muscle tone and tremor of some parts of the body - chin, hands. Infanib scale score 12-20 points. Spasticity rating according to the Ashworth scale is 3-4 points. Damage to the structures of the nervous system is manifested by characteristic syndromes:
- Increased neuro-reflex excitability.
- Vegetative-visceral dysfunction (neuroendocrine regulation disorder).
- Muscular dystonia (spasmodic muscle contractions).
Statistics show that signs of cerebral ischemia developing in the brain in newborns are often neurological in nature. The intensity and severity of neurological symptoms depends on the nature and extent of damage to brain structures.
Perinatal damage to brain structures is more pronounced in premature babies (suppression of central nervous system activity - 18%, convulsive readiness - 19%, hypertensive-hydrocephalic syndrome - 9%).
In infants of later gestation (33 weeks), vegetative-visceral disorders are more pronounced (in 44% of cases).
In full-term children, increased neuro-reflex excitability is more often observed, developing against the background of muscle hypertonicity (in 31% of cases).
Degrees of pathology in newborns
There are 3 degrees of ischemic damage to brain structures. Ischemia of the 1st degree in brain tissue in newborns is manifested by hyperactivity, sleep disturbance, loss of appetite, causeless, frequent crying, and increased muscle tone.
Symptoms of grade 2 ischemia in the brain tissue of a newborn include convulsive syndrome, increased intracranial pressure with accompanying symptoms.
There is protrusion of the fontanel, involuntary throwing back of the head, frequent crying, uncontrolled movements of the eyeballs, hydrocephalus (an abnormal increase in the diameter of the head).
Reflexes are sluggish, breathing and heart rate periodically slow down.
Stage 3 ischemia is characterized by severe depression of central nervous system functions, up to acute pulmonary failure, absence of reflexes, and coma.
Reasons for development
Ischemia in brain tissue develops as a result of oxygen starvation; all cases of pathology are associated with impaired blood flow caused by blockage or severe narrowing of the vascular lumen. Main reasons:
- Somatic diseases of infectious etiology in the mother.
- Bad habits of the mother (smoking, alcohol abuse).
- Birth injuries sustained by the fetus.
- Malfunctions of the endocrine system in the mother.
- Unfavorable course of pregnancy (toxicosis, threatened miscarriage, premature, complicated birth).
Infants who suffered from diseases during the perinatal period are susceptible to the development of ischemic lesions: pulmonary and heart failure, parasitic infestations, brain tumors, blood clotting disorders, and other pathologies of the hemostatic system.
Treatment methods
Timely diagnosis of disorders and treatment will help to avoid serious consequences of cerebral ischemia in newborns. Complex neurorehabilitation includes:
- Drug therapy using drugs with neuroprotective effects.
- Massotherapy.
- Passive therapeutic exercises.
- Applications of ozokerite in the extremities.
- Dry immersion. Without the use of an aquatic environment, conditions of partial weightlessness are created, similar to those in which the fetus lives during intrauterine development. An effective rehabilitation measure that allows you to reduce neurological symptoms and stabilize some hemodynamic parameters.
- Physiotherapy (laser therapy, magnetic therapy).
- Music therapy.
Therapy with pharmaceutical agents is aimed at eliminating convulsive syndrome, eliminating the consequences of hypoxia and cerebral edema. Correction of psychomotor functions will be performed using drugs:
- Vitamins of group B1, B6.
- Medicines based on L-carnitine (Elkar, Levocarnitine). They normalize metabolic processes at the cellular level and have an antihypoxic effect.
- Neuroprotectors based on amino acids and neuropeptides (Actovegin). They improve the relationship between neurons, stimulate reparative (restorative) processes in the central nervous system.
- Angioprotectors. They improve the condition of vascular walls, increase the tone of smooth muscles, and prevent the penetration of calcium ions through cell membranes.
- Nootropic (Glycine, Phenotropil, Gliatilin). Increases the resistance of brain structures to hypoxia. Accelerate the utilization of glucose, stimulate the exchange of nucleic acids, accelerate the synthesis of proteins, ATP, RNA.
- Anticonvulsants.
- Muscle relaxants. Restores normal muscle tone.
For mild forms of pathology, it is recommended to do professional massage, therapeutic exercises, physiotherapeutic and water procedures, and rehabilitation treatment can be carried out without the use of any pharmaceuticals.
Possible consequences of the disease
Common (78% of cases) consequences of cerebral ischemia in newborns are disorders of auditory and visual afferentation (the continuous flow of nerve impulses from the sensory organs to the nervous system).
Frequent complications of ischemic brain damage in newborns: cerebral palsy, epilepsy, ischemic stroke, which lead to disability and death (7-28% of cases).
Against the background of oxygen starvation, dementia, sensorineural deafness and cortical blindness can develop.
Damage to the central nervous system in newborns - video
From this video you will learn about the nuances of central nervous system damage and methods of treating this disease. To summarize, I would like to note that changes due to this pathology are completely reversible if treatment is started on time, namely in the first weeks of the baby’s life. Don't ignore the first symptoms. If any suspicious signs of this disease appear, immediately contact a neurologist for consultation.
Have you encountered CNS damage in your children? What treatments were you prescribed? What was the result? Tell us about your experience in the comments.
We recommend reading:
- Glomerulonephritis in children - symptoms, treatment Hemangioma in newborns - signs and treatment The child is often sick - what to do Miliaria in children - causes, symptoms and treatment
Damage to the central nervous system of hypoxic-traumatic origin in newborns
Etiology. The most common causes of damage are oxygen deficiency (hypoxia, asphyxia), various infections and intoxications. Less commonly, the direct cause may be mechanical damage to the brain in the intrapartum period.
Early diagnosis of the nature of cerebral damage in a newborn is very difficult. The variety and similarity of clinical manifestations of dysfunction of the central nervous system, the tendency of the brain to generalized reactions, the dynamism of the process, changing symptoms over several hours, layers of birth stress complicate the diagnostic capabilities of the doctor. In the acute period of the disease, it is often difficult to differentiate the infectious-inflammatory process, the consequences of mechanical intracranial trauma and asphyxia; it is difficult to establish whether certain symptoms are the result of a major hemorrhage or are caused by impaired cerebral hemodynamics, cerebral edema.
In clarifying the cause of dysfunction of the central nervous system and in making a leading diagnosis in the first days of a child’s life, anamnesis data are important. A detailed analysis of the mother’s health status, the characteristics of the course of pregnancy and childbirth makes it possible to clarify the nature of the damaging factor and determine the degree of risk of damage to the fetus.
Damage to the nervous system in newborns is characterized by a wide range of clinical and morphological changes - from mild functional disorders in hemolytic circulation disorders to severe symptoms of brain damage and vital functions in diffuse edema and intracranial hemorrhage.
Terminology. There is no generally accepted classification of CNS lesions in newborns yet. In recent years, the term “perinatal encephalopathy in newborns with central nervous system lesions” has become widespread in medical practice.
The most famous is the clinical classification of lesions of the nervous system in newborns and young children, developed by Yu. A. Yakunin et al.
According to the International Classification of Diseases, adopted by the 21st World Health Assembly for the Ninth Revision, in the perinatal period, the causes of damage to the central nervous system in children can be “asphyxia” (hypoxia) and “birth trauma”. To ensure possible earlier prediction and determination of pathogenetic therapy in the perinatal period, it is important to clarify the leading syndrome of the acute period, identifying the so-called “syndromic diagnosis”. In this regard, when making a diagnosis, the above classification can be used with the following changes: in the early neonatal period, the leading cause of damage to the central nervous system is indicated - “asphyxia” or “birth injury”, then the form of the disease is noted according to severity and the leading clinical syndrome; for example, with a predominantly hypoxic genesis of CNS damage, the diagnosis may be as follows:
- Asphyxia. Mild form of central nervous system damage. Acute period. Violation of hemocerebrospinal fluid dynamics. Syndrome of increased neuro-reflex excitability.
- Chronic intrauterine hypoxia, asphyxia during childbirth. Severe form of central nervous system damage. Brain swelling. Convulsive syndrome.
- Chronic intrauterine hypoxia. Moderate form of central nervous system damage. Violation of hemocerebrospinal fluid dynamics. Hypertensive-hydrocephalic syndrome.
For mechanical birth trauma:
- Birth trauma of the central nervous system. Moderate form. Violation of hemocerebrospinal fluid dynamics. Hypertension syndrome. Convulsive syndrome.
- Birth trauma of the central nervous system against the background of chronic intrauterine hypoxia. Severe form. Intracranial hemorrhage. Coma.
Clinic. Currently, depending on the severity of the damage, there are 3 clinical forms of central nervous system damage in newborns: mild, moderate and severe. The acute period of the disease lasts 7-10 days.
In mild forms of the lesion, clinical manifestations are based on transient disturbances of hemolytic circulation, which are associated with short-term hypoxic effects and the influence of birth stress. Cerebral disorders in most cases are caused by mild complications during labor, surgical interventions, and short-term acute fetal hypoxia. The duration and depth of damage to the fetus can be approximately determined by changes in the fetal cardiac activity during labor, the presence of meconium in the amniotic fluid, and a decrease in the pH value of the fetal blood.
The condition of such children at birth is usually not severe. The Apgar score is 6-7 points, due to impaired development of external respiration, cyanosis of the skin, and decreased muscle tone. Primary resuscitation measures, as a rule, turn out to be highly effective and permanently restore vital functions. Symptoms of cerebral disorders appear and may increase during the first 24-48 hours of postnatal life. Usually these are mild, unstable neurological symptoms in the form of general cerebral functional disorders, manifested by a syndrome of increased neuro-reflex excitability. The general condition of such children in the first days is moderate. Sleep disturbances, emotional motor restlessness, small-amplitude tremor of the upper and lower extremities, chin, spontaneous Moro reflex, and episodic horizontal nystagmus are noted. Children may experience regurgitation in the first hours after birth. Congenital unconditioned reflexes are revived with rapid depletion, some reflexes are depressed. Muscle tone is little changed and can be characterized by intermittent muscle dystonia. The functions of thermoregulation, sucking, and swallowing are preserved.
The mild form of the lesion is characterized by the rapid disappearance of clinical pathological symptoms. In most cases, persistent improvement in the condition of children is observed by the 4th-5th day of life.
Moderate damage to the central nervous system is usually observed in children with a combination of unfavorable course of the ante- and intranatal periods of development. The history reveals a variety of damaging factors during pregnancy associated with maternal diseases, occupational hazards, malnutrition of the pregnant woman, negative emotional reactions, various somatic and acute infectious diseases. During the period of childbirth; Women in labor develop weakness of labor forces, incoordination of labor, untimely rupture of amniotic fluid. Some children are born with the help of special obstetric techniques and surgical interventions (extraction by the pelvic end, obstetric forceps, vacuum extraction of the fetus, etc.). These complications contribute to longer-term fetal oxygen deficiency, metabolic disorders, and mechanical damage to the fetal brain. During childbirth, deafness of the fetal heart sounds, prolonged constant tachycardia or arrhythmias of cardiac activity are noted, which indicates the depletion of its compensatory adaptation mechanisms.
At birth, children in this group have Apgar scores ranging from 4 to 5 points. Suppression of reflex irritability, decreased muscle tone, and widespread cyanosis of the skin are noted. Children need respiratory resuscitation and correction of homeostasis. In the early post-resuscitation period of life, they require special therapeutic measures to normalize vital functions.
A dysfunction of the central nervous system is detected immediately after initial resuscitation or a short “light interval”. In most cases, the condition of children is severe, with a predominance in the first hours and days of life of general depression or the development of intracranial hypertension syndrome. With general depression, muscle tone is reduced or increased, and its asymmetry in the upper and lower extremities is possible. In the dynamics of the disease, muscle hypotension can often be replaced by dystension or hypertension. The child sometimes has no spontaneous movements for several days. There is inhibition of many innate unconditioned reflexes. Along with this, vegetative-visceral disorders are also observed in the form of periodic respiratory arrests, tachy- or bradycardia, gastrointestinal dyskinesias, and disturbances in thermoregulation (hypothermia in the first days of life) are often noted. Children suck sluggishly, often regurgitate, especially in the first hours after birth. They often have a reduced reaction to painful stimuli. Local neurological symptoms in most cases are absent or may be unstable in the form of differences in palpebral fissures, spontaneous large-scale horizontal nystagmus, and strabismus.
The clinical picture of hypertension syndrome is dominated by symptoms of increasing motor restlessness, hyperesthesia of the skin, and intermittent sleep of the child. Small-amplitude tremor of the chin and limbs is observed, sharply increasing with irritation. Symptoms of intracranial hypertension are bulging fontanelles, Graefe's and "setting sun" signs, and horizontal nystagmus. In children, short-term clonic convulsive twitching of the facial muscles or atypical convulsions in the form of automatic chewing movements, “pedaling” of the feet, and vasomotor disturbances are possible. These convulsive attacks are short-term, inconsistent, but they are characterized by their uniformity and recurrence in the same child. Convulsive seizures are more often detected during examination of the child, his swaddling and external irritations
The basis of the clinical symptoms in children with moderate damage to the central nervous system, according to most researchers, are edematous-hemorrhagic changes in the membranes and substance of the brain with dyscirculatory vascular paralysis and pinpoint diapedetic hemorrhages. In this case, the disease often occurs with liquor hypo- or normotension.
In the dynamics of the disease against the background of treatment, stabilization of the child’s vital functions occurs quite quickly, usually no later than the 6-7th day of life.
Most children with a moderate form of central nervous system damage are discharged home on the 10-12th day of life as their condition normalizes. This group of children should be under clinical supervision of a local pediatrician and neurologist. In cases where symptoms of intracranial hypertension persist during treatment, the child should be transferred to a specialized neurological department on the 7-10th day of life.
A severe form of central nervous system damage is the result of a combination of damaging factors during pregnancy and childbirth. Long-term chronic oxygen deficiency can be caused by severe forms of toxicosis (nephropathy, eclampsia), arterial hypertension in a pregnant woman, widespread edema, and significant proteinuria. As a result of this pathology, severe disturbances occur in the uteroplacental circulation and gas exchange between the mother and the fetus, which leads to a general delay in fetal development and intrauterine malnutrition. Along with chronic disorders, a severe form of central nervous system damage can be caused by acute pathology during childbirth (premature placental abruption, rupture of umbilical cord vessels, prolapse of the umbilical cord loop, uterine rupture during childbirth, massive blood loss during placenta previa, incorrect insertion of the presenting part of the fetus during childbirth, difficulties when removing the head and shoulder girdle of the fetus, etc.).
Children are born in a state of hypoxemic shock with severe! hemodynamic disorders. The Apgar score at birth does not exceed 3 points. Lack of breathing, impaired cardiac activity, atony and suppression of reflexes are noted. Newborns need respiratory and cardiac resuscitation, restoration of hemodynamics and metabolism. Newborns who have suffered severe intrauterine hypoxia develop post-asphyxia syndrome, the main manifestations of which are pulmonary, cardiovascular and cerebral disorders. After primary resuscitation and restoration of cardiac activity and external respiratory function, the child continues to have vascular insufficiency, respiratory disorders and insufficiency of adrenal cortex function against the background of severe depression of the central nervous system. The children are in a comatose state. They are inactive, moan weakly, there is no cry or it is weak, monotonous, sometimes aphonic. The child does not respond to painful and tactile stimuli. The skin is gray-cyanotic, cold to the touch, and general hypothermia is noted. Pronounced cyanosis around the eyes, mouth, cyanosis of the hands and feet. Breathing is uneven, shallow, with long pauses. Heart sounds are muffled, bradycardia is often observed, and a systolic murmur is heard over the heart area.
Symptoms of bulbar and pseudobulbar disorders with impaired sucking and swallowing may be observed. Lesions of individual cranial nerves are manifested by facial asymmetry, sagging of the lower jaw, ptosis, strabismus, etc. This condition is characteristic of diffuse cerebral edema or intracranial hemorrhage under the tentorium cerebelli. With hemorrhages over the tentorium cerebelli, the child’s severe anxiety, persistent yawning, forced positioning, and general stiffness due to increased muscle tone in various muscle groups predominate. Character! a sharp short or low-pitched cry. The palpebral fissures are wide open, the gaze is fixed, the pupils are wide or narrowed, motionless, exophthalmos and rotatory nystagmus are noted. Children lie with their heads thrown back due to a paradoxical redistribution of muscle tone. Sometimes heads; can be turned to one side. In this group of newborns, frequent repeated convulsive seizures are noted with a predominance of the tonic component with the shutdown of the respiratory muscles and attacks of secondary asphyxia. Unilateral seizures may also be observed, indicating subdural hemorrhages, which occur predominantly in full-term newborns. Convulsive syndrome is not always detected in the early stages of the disease and can appear only with the development of hydrocephalus.
The severity of clinical symptoms is due to generalized cerebral edema and intracranial hemorrhages. With asphyxia, subarachnoid hemorrhages are most often observed, clinically causing acute meningeal-hypertensive syndrome. Hemorrhages are often found in the substances of the brain, perivascularly in the cerebral cortex and in the medulla oblongata. With massive intracranial hemorrhages, especially with subtentorial localization, diffuse cerebral edema, compression of subcortical-stem formations occurs with a sharp disruption of vital functions and the development of cerebral coma.
Intensive therapy is indicated for children with severe central nervous system damage after initial resuscitation. Their prognosis is often unfavorable. In surviving newborns, the unstable condition persists until the 8-10th day of life; loss of sucking function and impaired swallowing are noted. These newborns require long-term therapy in a specialized neurological department and must be transferred at the age of 7-10 days from the maternity hospital to the hospital.