The pre-stroke condition is a dangerous phenomenon, which, if a person is not provided with first aid, leads to serious consequences and the development of a full-fledged stroke with severe brain damage. If measures are not taken in a timely manner, there is a high risk not only that the person will remain disabled, but also that he will die. Depending on gender, the manifestations of an approaching cerebral infarction are somewhat different, and this must be remembered. You can avoid a stroke only by knowing how the approaching problem manifests itself.
Symptoms
The signs are varied, and it is not easy to understand on your own what is happening. For general reasons, the FAST technique is used.
This is a mnemonic technique aimed at remembering the basic algorithm of actions to identify a pre-stroke condition or actual necrosis of cerebral structures. The measure relates to first aid.
Accordingly, the manifestations will be as follows:
- Face or face. Against the background of brain damage, paresis or paralysis of facial muscles occurs. As a rule, on one side. Defined as skew. You need to ask the patient to smile. If it is impossible or there is severe asymmetry, the symptom is recorded. Most likely, acute ischemia occurs.
- Arm or hand. Pre-stroke can be recognized by weakness of the muscles of the upper extremities. The patient cannot lift both of them above his head at once, much less hold them in this position for a long time.
- Speech. Speech. The speaking process is disrupted. The voice is weak, the phrases are slurred. There may be a complete lack of function.
- Time. Time. An indication that if any of the named signs are detected, an emergency team must be urgently called.
All symptoms of pre-stroke are divided into generalized or general and focal (typical for damage to a specific lobe of the brain).
The first ones occur in patients with cerebrovascular accidents. Everyone, without exception.
- Intense headache. It can be unbearable. Accompanies the victim throughout the acute condition. By nature - baling. Feeling as if someone is hitting the back of the head and parietal area with a hammer. Follows the beat of the heart.
- Weakness, general asthenia. The patient cannot stand on his feet, and a decrease in muscle tone is detected.
- Nausea, vomiting. They are relatively rare. In this case, the episode of gastric emptying does not bring relief. This is not poisoning. Stimulation of special centers of the brain occurs against the background of ischemia and a decrease in the quality of nutrition of the area. The process is reflexive in nature and lasts several minutes.
- Impaired consciousness. By type of fainting. Usually shallow, the patient is easily brought out of syncope.
There are many more focal manifestations. The exact symptoms depend on the location of the lesion.
Frontal lobe
Responsible for creativity, behavioral factors, thinking and its productivity, partly for coordination, and other functions.
Possible signs include:
- Disturbances of mnestic and cognitive processes. The patient is not able to think adequately, there are illogical statements or complete apathy, lack of reactions to the surrounding reality.
This is a common occurrence. May be characterized as stupor. The entire acute period continues.
- Unsteadiness of gait. Inability to walk in a straight line. A typical symptom of neurological abnormalities, but not specific.
- Foolishness in behavior, tearfulness, emotional, affective disorders.
- Numbness or paralysis of the half of the body opposite the source of the lesion.
Parietal lobe
Responsible for the basic mnestic functions of the logical series. Invoice, letter, etc.
- Inability to perform simple arithmetic operations, perceive information on physical media, or write independently.
- Olfactory hallucinations.
- False tactile sensations. Like paresthesia, non-existent touches, goosebumps running all over the body.
These are manifestations of the so-called irritation (irritation) of the cortex, which responds with artificially induced signals.
These impulses move as part of feedback to the nerve endings that the skin is rich in.
Temporal lobes
- Epileptic seizures. Type of tonic-clonic convulsions, loss of consciousness. Episodes may occur more than once during one pre-stroke condition. This is a negative sign.
- Memory impairments of various forms.
- Olfactory hallucinations.
- Complex syndromes such as oneiric stupefaction. It is a complex deception of the senses. The patient sees what is not there, feels false images.
- Violation of the process of analyzing audio information. In particular, it is impossible to perceive and understand the logic of oral speech and the meaning of the interlocutors’ statements.
Occipital lobe
Responsible for analyzing visual information, at the same time, the cerebellum is located here. The disorder and its work develops.
- A typical symptom is the simplest visual hallucinations and illusions. Feeling of flickering, flashes (photopsia), fog, scotomas (areas of loss of perception in the form of black spots).
- Transient blindness. Temporary total loss of vision.
- Dizziness, uneven gait. Disorientation in space.
Brain stem
Lesions in this area pose the greatest danger to the patient’s life, even outside of a stroke, because important body functions are weakened.
- Irregularity of breathing, cardiac activity. Dangerous arrhythmias and cessation of muscle structure (asystole) occur.
- Deep fainting (falling into a coma).
Symptoms before a stroke are nonspecific - headache, nausea, disturbances in the functioning of the sensory organs, confusion, and fainting. They are identical to those with a full-fledged stroke, only they last somewhat less.
Symptoms of the pre-stroke condition last for about several hours, or at most a day. Less is possible, more is never. This is the basis for revising the diagnosis.
First signs
To prevent a vascular catastrophe in the brain, it is necessary to know the first signs of a pre-stroke condition. Both men and women are susceptible to circulatory disorders in the central nervous system, but the initial manifestations of the pathological process differ.
| Signs in men | Signs in women |
| Feeling of uncertainty in determining one's position in space. | Severe megrenous pain. |
| Ringing, whistling and buzzing in the head. | Decreased intensity of facial activity. |
| Auditory distortion. | Lack of normal nerve conduction in the facial muscles. |
| Incoherent speech. | Decreased strength and motor activity of the limbs on one side. |
| Impaired ability to concentrate. | Impaired ability to speak, with preserved understanding of someone else's speech. |
| Temporary memory loss. | Disorder of the visual neurosensory system. |
| Decreased perception of various stimuli. | Temporary damage to the extraocular muscles. |
| Impaired motor functions. | Disorder in the visual system. |
| Difficulty maintaining balance. | Violation of the vestibular apparatus. |
| Overflow of blood vessels on the face. | Vomiting reflex. |
| Manifestation of hyperhidrosis. | Paroxysmal involuntary muscle contractions. |
| Breathing with wheezing. | Self-perception disorder. |
| Fluctuations in body temperature. | Syncope syndrome. |
| Nervous excitement. | Sagging corner of the mouth. |
| Feeling of approaching death. | Feeling of mental unsettlement. |
| Amentive disorder. | |
| Lightening of the face caused by changes in the tone of skin vessels. | |
| High blood pressure numbers. | |
| Sharp piercing pain in the head. |
What to do at home
First aid must be provided to the patient. Or to yourself, if the condition took you by surprise and there is no one nearby.
The first aid algorithm at home is as follows:
- The first warning signs should be grounds for calling an ambulance. Moreover, if at least one sign is present according to the FAST method.
It helps determine the pre-stroke condition by muscle tone, innervation of the facial muscles and ability to speak. The main functions of the central nervous system are assessed.
- Before the doctors arrive, you need to open the window to provide fresh air. This is a way to partially restore normal gas exchange. Accordingly, the risk of transforming the condition into a full-fledged stroke is reduced.
- Sit down and relax. It is not recommended to take medications unless a possible emergency has been discussed with your doctor. In this case, you need to take the prescribed pills.
- Measure blood pressure. In the setting of a pre-stroke, blood pressure levels are usually below normal. Insignificant. With severe disturbances, the tonometer readings drop further. The level assessment is repeated every 20 minutes.
- Move as little as possible. It is not recommended to lie down, so as not to disrupt the already fragile hemodynamics. Do not raise your arms and legs high, so as not to increase peripheral blood flow due to a drop in cerebral blood flow.
- Calm down. Nerves and negative emotions lead to the release of adrenal hormones and catecholamines, which have a vasoconstrictor effect. Tissue trophism will weaken and only get worse.
Upon arrival, doctors will tell you about your condition. Brief and to the point. Next, the issue of transportation to the hospital is resolved.
There are no options, because sensible medical workers will not risk leaving the patient in place. A stroke is possible; it will not be possible to distinguish it “by eye” from transient ischemia.
Under no circumstances should you refuse. Is it dangerous.
Prevention
To avoid the development of a pre-stroke condition, you need to follow a few simple recommendations:
- completely give up addictions;
- If possible, avoid physical and emotional stress;
- exclude from the diet fatty and spicy foods, sweets and salty foods, smoked foods and preservatives, carbonated drinks and strong coffee;
- donate blood once every three months to determine the level of cholesterol in the blood;
- enrich the diet with products that contain large amounts of pectin, vitamins and microelements beneficial to the body;
- maintain blood pressure levels no more than 140 per 90 millimeters of mercury;
- if necessary, restore body weight to normal;
- be outdoors every day;
- prevent hypothermia and overheating of the body;
- promptly treat diseases of the cardiovascular system;
- Take medications only as directed by your clinician.
The main preventative measure is to undergo a full medical examination every year.
Pre-stroke condition is a series of symptoms, the appearance of which indicates the approach of a stroke. If a person is not provided with timely medical care, severe brain damage can occur. This condition is most often observed in older people.
Diagnostics
It is already carried out in stationary conditions. The main specialist is a neurologist. To begin with, the general condition of the patient is assessed.
As necessary, the patient is removed from an acute situation and primary care is provided.
Then they wait for stabilization of well-being and restoration of hemodynamics. At the end of the critical phase, you can begin the examination.
The events are:
- Oral survey. When did the disturbances begin, what sensations did the patient experience, what is the situation now. Anamnesis collection. Pathologies, family history, bad habits, lifestyle in general.
- Measurement of blood pressure and heart rate. Usually both indicators are within normal limits at the end of the acute phase. These are routine techniques. They allow you to put forward hypotheses regarding the condition and help determine the vector of further management.
- Daily monitoring according to indications. Makes it possible to diagnose cardiac pathologies and arterial hypertension.
- Electrocardiography. Used to clarify the nature of functional disorders of cardiac structures.
- EEG. Evaluates brain activity.
- MRI. According to indications, if there is a need to identify suspected damage to cerebral tissue. Distinguish the pre-stroke condition from necrosis.
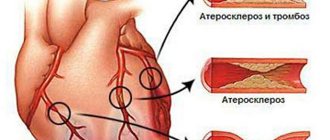
- Biochemical blood test. Doctors are mainly interested in low- and high-density lipid levels. Simply put, these are cholesterol levels slightly expanded from those in the general clinical study. Used to diagnose atherosclerosis.
- Dopplerography of neck vessels, including the vertebrobasilar region, carotid artery, cerebral structures. Duplex scanning. Used to determine blood flow speed and nutrition quality. Perhaps the main technique in diagnosing the causes of a pre-stroke condition.
For what purpose is such an extensive arsenal of activities used? The main task is far from identifying the consequences of pathology. Although this is important. Doctors are trying to find the origin factor. That is, what provoked acute ischemia, because the next step in the progression of the disease is a stroke.
Adaptation
The key to normal continuation of life is adaptation to new conditions and a new self after a stroke. It covers all aspects of the patient’s life. He needs to learn to move again, take care of himself, believe in his own strength, and sometimes he needs to learn to think and speak again.
Emotions
The worst thing that relatives of a stroke survivor can face is his reluctance to recover, depression, despondency, and disappointment.
A person stops seeing the future, suffers from pain, discomfort, and considers himself a burden. Often, experiences of disappointment are replaced by aggression towards oneself and loved ones. Suicide attempts are possible. This range of feelings and emotions is possible if a person is aware of what is happening to him.
Treatment
It is carried out using several methods. There are three tasks. Relieve symptoms and residual signs, eliminate the root cause and prevent relapses.
Drug correction involves the use of the following drugs:
- Antihypertensives if there is a stable increase in blood pressure. ACE inhibitors, beta blockers, calcium antagonists, centrally acting agents, diuretics with a mild potassium-sparing effect.
- Statins. For the rapid removal of cholesterol and the elimination of already formed plaques, provided that they have not hardened due to calcium salts. Atoris as the main one.
- Anticoagulants and antithrombotic. Eliminate blood clots. They are not allowed to form. Restore the fluidity and rheological properties of liquid connective tissue. Heparin or Aspirin-Cardio.
- Angioprotectors. Protects blood vessels from destruction.
Other medications as indicated. If medications are ineffective or obviously ineffective, surgical treatment is prescribed.
It is mainly needed for advanced atherosclerosis, vascular defects, such as congenital anomalies or aneurysms, and other processes.
The tactics are selected by the doctor. Open interventions are now used less and less often, preferring endoscopic operations. Therefore the risks are minimal.
A radical change in lifestyle is shown. Refusal of smoking, alcohol, psychoactive substances, and independent uncontrolled use of any drugs.
Walking for 2 hours a day or more is recommended, but the main thing is not to overexert yourself. Limit salt intake to 7 grams per day. Get at least 7 hours of quality sleep per night.
It makes sense to adjust your diet. Less fat, more protein and vitamins. A standard treatment table No. 10 will do. You need to approach adapting it to yourself creatively so that the diet does not turn into a routine chore.
Attention:
Traditional methods are not effective. This is a waste of energy, time, disappointed hopes and a loss of a precious moment to start therapy.
Moreover, some “grandmother’s recipes” carry potential dangers. You should not resort to such dubious methods of treatment.
The total duration of therapy and rehabilitation is 3-6 months. Then it is important to follow simple rules of prevention to prevent relapse. Including diet, giving up bad habits, minimal physical activity, avoiding stress and mastering relaxation techniques.
Causes
The main one was and remains atherosclerosis. This is a narrowing or blockage of blood vessels with cholesterol plaques. It can be easily eliminated only in the early stages; in advanced stages, surgery is required.
In second place is hypertension. With high, persistent performance.
Impairment of the pumping function of the heart is slightly behind. The myocardium is not able to contract with the required force, hence the lack of nutrition of all organs and systems in the systemic circulation.
Other reasons are much less common.
Risk factors
They do not directly cause the onset of a pre-stroke condition, but they increase the likelihood of it almost three times, and even more (depending on the specific moment).
- Smoking.
- Old age 60+. The pathology also occurs in persons slightly younger, minus 10 years.
- Being male.
- A history of cardiovascular diseases, as well as endocrine diagnoses.
- Unfavorable family history, burdened heredity.
- Alcohol abuse, drug addiction.
- Inadequate sleep.
- Unbalanced diet.
- Acclimatization, moving to another geographical region with different weather and temperature conditions.
- Menopause in women, as well as menopause in the stronger sex. Hormonal changes, attenuation of the body’s basic reproductive functions.
The patient can correct most of the factors presented on his own. Apart from age.
But in this case, it is enough to regularly consult with a neurologist and other specialists. According to indications.
How long do you live after a stroke?
Depressing statistics concern how many people live after a hemorrhagic stroke. Approximately 70% of those who have suffered this form of the disease die in the first month.
The prognosis for life after an ischemic stroke is somewhat more favorable. Up to 30% of patients die from it in the first thirty days.
Moreover, about 40% die in the first three days. Almost all of them are in a severe comatose state after a stroke and die without regaining consciousness. The main causes of death are cerebral edema, their displacement and a large area of damage. The rest die from respiratory problems, pneumonia, kidney dysfunction, blood poisoning, arterial blockage, and heart complications.
For reference. In approximately 25% of patients, life expectancy after a stroke can reach 10 years, in 50% - 5 years.
Trigger factors
They act as direct triggers.
- Consumption of alcohol in any quantity.
- Smoking. Due to a sharp spasm of cerebral vessels, basilar, carotid arteries.
- Stress, intense mental stress.
- Excessive, inappropriate physical activity. With little or insufficient training.
- Sharp tilt. Patients with possible pathologies of the cardiovascular system need to exercise extreme caution. All movements are smooth, gradual. It’s better not to bend at the waist at all, but to squat if you need to lift something.
- Acute pain syndrome.
All points are subject to evaluation. Their independent correction is possible.
Possibility of recovery
The prognosis for quality of life and how many years people live after a stroke are influenced by a large number of factors. Among them are localization, volume, degree of damage. The more extensive it is, the more severe the consequences will be.
Recovery will take longer if the patient was in a coma , paralyzed or lost sensation. Severe neurological manifestations that appear in the first week after the blow leave virtually no chance of recovery.
It is believed that the prognosis is unfavorable in those patients who have suffered a stroke caused by atherosclerosis or embolism.
The chances of full recovery are low in patients suffering from diabetes, severe heart disease, smokers and alcohol addiction.
The chances of rehabilitation are less for older people.
If medical care for a stroke was received almost immediately after the stroke, the likelihood of a quick and complete restoration of function is high. If there is a delay in providing assistance, there may be no chance of their return.
It is noted that in approximately 60-70% of cases, patients cannot work or move normally. After this period, clear manifestations of neurological disorders remain in 40% of people. After the first year from the moment of the attack - in 25%.
For reference. An important point in determining the prognosis is the restoration of lost motor functions during the first three months from the moment of the stroke. If the motor activity of the hand does not return even to a minimal extent a month after the blow, the prognosis for recovery is unfavorable.
The prognosis worsens with recurrent stroke . According to statistics, it occurs in approximately 30% of patients within five years after the first case. At risk are patients with chronic cardiovascular diseases. Moreover, after an ischemic stroke the prognosis is better than after a hemorrhagic stroke.
Despite the large number of objective factors that reduce the likelihood of rehabilitation, those that allow the patient to recover, if not completely, then at least partially, are distinguished.
These factors include care, proper nutrition, positive emotions, and movement. They allow a person to get used to a new life.