Characteristics of the disease
PE is not an independent pathology. As the name suggests, this is a consequence of thrombosis.
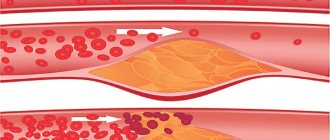
A blood clot, breaking away from its place of formation, rushes through the system with the bloodstream. Often blood clots occur in the vessels of the lower extremities. Sometimes localized in the right side of the heart. The thrombus passes through the right atrium, ventricle and enters the pulmonary circulation. It moves along the only paired artery in the body with venous blood - the pulmonary artery.
A traveling thrombus is called an embolus. It rushes towards the lungs. This is an extremely dangerous process. A blood clot in the lungs can suddenly block the lumen of the branches of the artery. These vessels are numerous in number. However, their diameter decreases. Once in a vessel through which the blood clot cannot pass, it blocks blood circulation. This is what often leads to death.
If a patient has a blood clot in the lungs, the consequences depend on which vessel is blocked. An embolus disrupts the normal blood supply to tissues and the possibility of gas exchange at the level of small branches or large arteries. The patient experiences hypoxia.
Content
Pulmonary embolism is considered an emergency condition that threatens human life, which is not an independent disease, but develops against the background of other pathologies.
There are plenty of reasons why thrombosis in the lungs can occur, but regardless of the etiological factor, this condition is extremely dangerous for human life and in 85% of cases leads to death. With the development of thromboembolism, a blockage of blood vessels appears in the lumen of the pulmonary artery, which partially or completely blocks the blood flow to the internal organs and systems. People over 50 years of age, as well as those with a history of pathologies of the heart and blood vessels, are at risk for developing this condition.
Blood clot in the pulmonary artery
The survival rate for a blood clot in the lungs is quite low, since death can occur instantly.
Important! In order to reduce the likelihood of developing a blockage, people who are at risk should periodically visit a cardiologist and undergo the necessary examinations.
Severity of the disease
Blood clots in the lungs occur as a result of complications of somatic diseases, after birth and surgical conditions. The mortality rate from this pathology is very high. It ranks third among the causes of death, second only to cardiovascular diseases and oncology.
Today, pulmonary embolism develops mainly against the background of the following factors:
- severe pathology;
- complex surgical intervention;
- injury received.
The disease is characterized by a severe course, many heterogeneous symptoms, difficult diagnosis, and a high risk of mortality. Statistics show, based on post-mortem autopsy, that blood clots in the lungs were not diagnosed in a timely manner in almost 50-80% of the population who died due to pulmonary embolism.
This disease progresses very rapidly. That is why it is important to quickly and correctly diagnose the pathology. And also provide adequate treatment that can save a human life.
If a blood clot in the lungs is detected in a timely manner, the survival rate increases significantly. The mortality rate among patients who receive the necessary treatment is about 10%. Without diagnosis and adequate therapy, it reaches 40-50%.
Symptoms
Blood clots often remain invisible and are rarely diagnosed. But if the blood clot has already come off, then the person cannot be saved, because death occurs instantly.
However, there are several key points that you should immediately pay attention to and do not hesitate to visit a doctor with suspected thrombosis. Here are some of them:
- Severe sudden shortness of breath.
- Chest pain.
- Dizziness or loss of consciousness.
- Reduced blood pressure.
- Single symptoms of tachycardia.
- Swollen veins in the neck.
- Cough with blood.
- Too pale skin.
- The skin on the upper half of the body may turn blue.
- Temperature increase.
These are the symptoms that patients who suffered thrombosis complained about. The rest of the people did not notice any changes in the body. This suggests that you need to closely monitor your body and respond adequately to disruptions in its functioning.
Causes of the disease
A blood clot in the lungs, the photo of which is located in this article, appears as a result of:
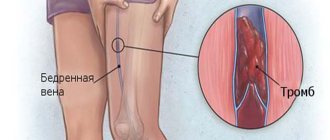
- deep vein thrombosis of the lower extremities;
- formation of a blood clot in any area of the venous system.
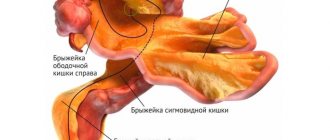
Much less frequently, this pathology can be localized in the veins of the peritoneum or upper extremities.
Risk factors presuming the development of pulmonary embolism in a patient are 3 precipitating conditions. They are called Virchow's triad. These are the following factors:
- Reduced blood circulation rate in the venous system. Congestion in blood vessels. Slow blood flow.
- Increased susceptibility to thrombosis. Hypercoagulability of blood.
- Injury or damage to the venous wall.
Thus, there are certain situations that provoke the occurrence of the above factors, as a result of which a blood clot is detected in the lungs. The reasons may be hidden in the following circumstances.
The following can lead to a slowdown in venous blood flow:
- long trips, travel, as a result of which a person has to sit for a long time in an airplane, car, train;
- hospitalization, which requires bed rest for a long period.
Hypercoagulability can be caused by:
- smoking;
- use of contraceptives, estrogen;
- genetic predisposition;
- oncology;
- polycythemia - a large number of red blood cells in the blood;
- surgical intervention;
- pregnancy.
Injuries to the venous walls result from:
- deep vein thrombosis;
- household leg injuries;
- surgical interventions on the lower extremities.
Preventive measures
Preventive measures are divided into secondary and primary. In the first case, we are talking about preventing relapse of the disease. By primary we mean measures taken when a person is prone to thrombosis.
In this case, it is recommended to follow the following principles:
- It is necessary to ensure an active lifestyle: periodically play sports, take walks, spend more time in the fresh air.
- If there is increased blood clotting, it is necessary to take medications to thin it.
- It is important to avoid foods high in cholesterol. This will avoid deterioration of the structure of blood vessels.
- It is necessary to regularly monitor blood clotting, glucose and cholesterol levels in the blood.
- Inflammatory processes and infectious diseases should be eliminated in a timely manner. They can become an impetus for the development of thrombosis.
- Drinking strong alcoholic drinks and smoking is strictly prohibited.
- For varicose veins of the lower extremities, pneumocompression of the legs should be performed, which helps eliminate swelling.
Read also: Do compression socks help with varicose veins?
After treatment against thromboembolism, people live for a long time. But in this case, it is necessary to be observed by a doctor to prevent relapse of the disease.
Pulmonary thrombosis is surpassed only by cardiac ischemia and stroke in the number of deaths.
It is extremely important to get rid of bad habits and normalize your diet. From time to time, a preventive course of treatment with anticoagulants is carried out.
With relapses of the disease, the probability of death increases several times.
Risk factors
Doctors identify the following predisposing factors in which a blood clot is most often detected in the lungs. The consequences of the pathology are extremely dangerous. Therefore, it is necessary to pay close attention to the health of those people who have the following factors:
- decreased physical activity;
- age over 50 years;
- oncological pathologies;
- surgical interventions;
- heart failure, heart attack;
- traumatic injuries;
- varicose veins;
- use of hormonal contraceptives;
- complications of childbirth;
- erythremia;
- overweight;
- genetic pathologies;
- systemic lupus erythematosus.
Sometimes blood clots can be diagnosed in the lungs of women after childbirth, especially severe ones. As a rule, this condition is preceded by the formation of a clot in the thigh or calf. It makes itself felt by pain, fever, redness or even swelling. Such a pathology should be reported to the doctor immediately so as not to aggravate the pathological process.
Disease prevention
It is possible to avoid a sad fate if you follow the recommendations of specialists on following the rules of prevention. The same statistics show that following them can reduce the risk of blood clots by almost 85%. These are the recommendations:
- Maintaining an active lifestyle that involves performing feasible physical activity.
- Therapeutic gymnastics classes.
- Prolonged stay in the fresh air.
- Daily walking.
- Nutrition correction, which includes excluding fatty, fried and spicy foods from the menu.
- Normalization of weight.
- Quitting smoking and drinking alcohol.
- Wearing comfortable shoes.
- Constant use of compression garments to prevent the development of varicose veins.
- Taking anticoagulants to prevent increased blood clotting.
- Implantation of vena cava filters, ensuring normalization of blood flow and eliminating the possibility of blood clots.
Attentive attitude to the state of your health, timely seeking medical help, maintaining a healthy lifestyle, strict adherence to medical recommendations - this is the key to successfully resisting the negative manifestations of pathology.
Characteristic symptoms
In order to promptly diagnose a blood clot in the lungs, the symptoms of the pathology should be clearly understood. You should be extremely careful with the possible development of this disease. Unfortunately, the clinical picture of pulmonary embolism is quite varied. It is determined by the severity of the pathology, the rate of development of changes in the lungs and the signs of the underlying disease that provoked this complication.
If a blood clot is present in the lungs, the patient's symptoms (mandatory) are as follows:
- Shortness of breath that suddenly appeared for unknown reasons.
- There is an increase in heart rate (more than 100 beats in one minute).
- Pale skin with a characteristic gray tint.
- Pain syndrome that occurs in different parts of the sternum.
- Impaired intestinal motility.
- Sharp blood filling of the neck veins and solar plexus, their bulging is observed, and pulsation of the aorta is noticeable.
- The peritoneum is irritated - the wall is quite tense, pain occurs when palpating the abdomen.
- Heart murmurs.
- Blood pressure drops significantly.
In patients who have a blood clot in the lungs, the above symptoms are necessarily present. However, none of these symptoms are specific.
In addition to the mandatory symptoms, the following conditions may develop:
- fever;
- hemoptysis;
- fainting;
- chest pain;
- vomit;
- seizure activity;
- fluid in the sternum;
- coma.
Symptoms of a blood clot in the lungs, emergency care and treatment
A thrombus in the lungs is a pathological clot that clogs the vascular bed and prevents blood from moving normally through the arteries and veins. It leads to the development of such a pathological process as PE - pulmonary embolism.
Thrombosis is not an independent nosological entity. This is a consequence of venous thrombosis. In 90% of cases, a pulmonary thrombus enters the affected organ from deep-lying leg veins. A clot traveling through an artery is called an embolus. 85% of patients with this diagnosis die, death occurs at any time.
The risk group consists of patients over 50 years of age (usually men). A history of cardiovascular disease significantly aggravates the situation.
It is possible to identify a number of reasons and predictive factors that significantly influence the development of such a disease as pulmonary artery thrombosis.
These include:
- pathology of the heart and blood vessels;
- malignant neoplasms;
- blood diseases;
- varicose veins and thrombophlebitis;
- increased blood clotting;
- endocrine pathologies;
- excess body weight;
- bad habits;
- taking medications that affect the functioning of the cardiovascular system and the blood clotting process;
- staying in the same position for a long time (bed rest, sitting for a long time during flights or moving);
- surgical interventions;
- tumor formations, cystic formations in the uterus.
In addition to a blood clot, pulmonary thrombosis is caused by a blood clot of fatty or air origin.
According to the severity of the pathological process, pulmonary embolism is divided into 3 stages:
- Massive.
- Submassive.
- Not massive.
At the first stage, 50% or more percent of all pulmonary vessels are affected. Blood clots block the lumen of the lung trunk or its main arteries. In this case, a sharp decrease in blood pressure occurs, and a state of shock occurs.
In the submassive form of the detected disease, no more than 30%-50% of the pulmonary arteries are affected. A thrombus in the lungs blocks the lobar and segmental arteries, causing dysfunction of the right ventricle.
The third stage is characterized by blockage of small pulmonary arteries, and the vascular bed is slightly affected. Symptoms are mild, and heart attacks rarely occur.
According to the flow, the disease can be divided into three forms:
- Acute - the course is rapid, detached blood clots clog the large pulmonary artery, breathing stops, heart contractions stop, and death occurs.
- Subacute - accompanied by repeated heart attacks, lasts several weeks, very often resulting in the death of the patient.
- Chronic - frequent damage to small vessels, heart failure develops.
The clinical picture of the disease is very diverse.
Its course is influenced by the symptoms and severity of the underlying disease, and the rate of pathological changes.
If there is a blood clot in the lungs, there are symptoms of the disease, the presence of which is mandatory:
- sudden shortness of breath that occurs for no apparent reason;
- the heart rate increases significantly (over 100 beats/min.);
- the skin turns pale and acquires a pale gray tint;
- a painful attack occurs in different locations in the chest area;
- intestinal motility changes;
- the veins of the neck and solar plexus are filled with blood, they bulge significantly, the aorta is pulsating;
- symptoms of peritoneal irritation occur, severe pain is felt when palpating the abdomen;
- During auscultation, heart murmurs are heard;
- Blood pressure drops significantly.
If blood clots are detected in the lungs, all of the above symptoms must be present, but none of them are specific.
In addition to the main symptoms, the following signs of the disease may be observed:
- feverish condition;
- blood when coughing;
- fainting;
- pain in the sternum;
- vomit;
- spasm;
- fluid in the sternum;
- coma.
Pulmonary thrombosis causes severe pathological consequences that lead to the patient's death or severe disability.
If a blood clot breaks loose in the lungs, the doctor has little time to make a decision. It depends on the degree of embolism. If the lesion is small-focal, there is a possibility of spontaneous resorption of the blood clot even without treatment. With extensive damage, a heart attack often develops, which can lead to death.
Symptoms are observed in only 50% of all cases. The rest hardly notice anything. Death occurs within a few minutes.
Diagnosing pulmonary embolism is very difficult. In order to determine which veins are blocked or their number, it is necessary to conduct a diagnostic examination.
It includes:
- collection of anamnesis of illness and life;
- an external examination is carried out (pallor and blue tint of the skin, auscultation of the heart and lungs);
- general and biochemical blood test;
- carrying out a coagulogram;
- checking for the presence of D-dimers (information about the presence of traces of destruction of blood clots in the pulmonary artery);
- taking an electrocardiogram;
- radiography;
- Ultrasound of the heart, lower extremities;
- CT scan;
- angiography;
- echocardiography;
- ventilation-perfusion scintigraphy.
The sooner the correct diagnosis is made, the sooner emergency treatment will be started.
Urgent Care
If there is a suspicion that the blood clot is capable of breaking off or this has already happened, the symptoms begin to increase very rapidly. Death can occur quickly. Therefore, it is necessary to send the patient to the intensive care unit as quickly as possible.
The following immediate relief measures must be taken:
- central vein catheterization;
- administration of Reopoliglucin or glucose-novocaine mixture;
- Medicines are administered intravenously: Heparin, Enoxaparin;
- severe pain is relieved with narcotic analgesics: Promedol, Morin, Droperidol;
- oxygen therapy;
- administration of thrombolytics: Streptokinase, Urokinase;
- for arrhythmia, use magnesium sulfate, Digoxin, Panangin, Ramipril;
- in case of shock, Prednisolone, Hydrocortisone, No-shpa, Eufillin, Papaverine are administered.
After the first resuscitation measures have been carried out, further therapy is necessary.
It is divided into:
- thrombolytic therapy;
- surgical intervention.
Pulmonary artery thrombosis can begin to be treated with Heparin: intravenously for 7-10 days under the control of blood clotting.
Three days before the end of therapy, medications are prescribed in the form of tablets:
- Warfarin.
- Cardiomagnyl.
- Thrombo ACC.
- Thrombostop.
These drugs should be taken for 12 months and under constant monitoring of the clotting process.
In addition to Heparin, the following is prescribed:
- Streptokinase.
- Fraxiparine.
- Urokinase.
- Tissue plasminogen activator.
Symptoms of the disease can be relieved with this thrombolytic therapy, but it is not carried out if surgery has been performed. This therapy is not prescribed if there is a high likelihood of bleeding (for example, with a peptic ulcer).
The operation is performed exclusively in those conditions in which a significant area has been damaged - blood clots localized in large branches or the trunk of the artery are removed to restore full blood flow. The prognosis of the disease after surgery is unpredictable. But in most cases this is the only option for saving a person.
Blood clots tend to break off, and if this happens, the consequences can be very sad. Death occurs within a few minutes. The acute pathological process ends in 90% of cases with cardiac arrest.
Consequences and prevention
It is much easier to prevent pulmonary artery thrombosis than to subsequently treat the disease itself and its consequences. The process of blood clot formation can be reduced by 80% if you follow all the preventive measures recommended by your doctor.
The risk group includes the following categories of the population:
- patients whose age exceeded 40 years;
- patients with a history of stroke or heart attack;
- with body weight exceeding the upper limit of normal;
- if there is a history of thromboembolism;
- patients who have undergone surgery in the chest, lower extremities, and organs located in the pelvic and abdominal areas.
The main preventive measures include:
- performing gentle physical exercises;
- maintain physical activity, do not sit in one place for a long time;
- after a heart attack, get out of bed as quickly as possible;
- complete refusal to wear high-heeled shoes;
- eradication of bad habits;
- adherence to the principles of healthy eating;
- taking anticoagulants under the direct supervision of a physician;
- wearing compression garments to prevent the development of varicose veins;
- timely treatment of all chronic diseases.
Those patients who have diseases of the cardiovascular system should visit a cardiologist for a preventive examination at least twice a year.
Possible complications include:
- death within minutes;
- inflammation and death of the lung;
- further development of pleurisy;
- lack of oxygen;
- the occurrence of relapses of the disease (most often repeated within 10 months after the first incident).
According to medical statistics, every fifth patient who has suffered pulmonary thrombosis dies within the first 12 months, and 20% of patients die over the next four years.
Source: https://varicozinfo.ru/tromby/tromb-v-legkih.html
Course of the disease
Since pathology is a very dangerous disease that does not exclude death, the symptoms that arise should be considered in more detail.
Initially, the patient develops shortness of breath. Its occurrence is not preceded by any signs. The reasons for the manifestation of anxiety symptoms are completely absent. Shortness of breath appears on exhalation. It is characterized by a quiet sound accompanied by a rustling hue. At the same time, she is constantly present.
In addition, PE is accompanied by an increased heart rate. Can be heard from 100 beats or more in one minute.
The next important sign is a sharp decrease in blood pressure. The degree of reduction of this indicator is inversely proportional to the severity of the disease. The lower the pressure drops, the more serious the pathological changes caused by pulmonary embolism.
Pain sensations depend on the severity of the disease, the volume of damaged vessels and the level of disorders that have occurred in the body:
- Pain behind the sternum, which has an acute, bursting character. This discomfort characterizes blockage of the artery trunk. Pain occurs as a result of compression of the nerve endings of the vessel wall.
- Angina discomfort. The pain is of a compressive nature. Localized in the heart area. It often radiates to the shoulder blade or arm.
- Painful discomfort throughout the sternum. This pathology can characterize a complication - pulmonary infarction. Discomfort increases significantly with any movement - deep breathing, coughing, sneezing.
- Pain under the ribs on the right. Much less often, discomfort may occur in the liver area if the patient has blood clots in the lungs.
There is insufficient blood circulation in the vessels. This can cause the patient to:
- painful hiccups;
- tension in the abdominal wall;
- intestinal paresis;
- bulging of large veins in the neck and legs.
The surface of the skin becomes pale. An ashy or gray tint often develops. Subsequently, blue lips may develop. The last sign indicates massive thromboembolism.
Sometimes the patient hears a characteristic heart murmur and an arrhythmia is detected. In the event of a pulmonary infarction, hemoptysis is possible, combined with severe chest pain and a fairly high temperature. Hyperthermia can last for several days, and sometimes for a week and a half.
Patients who have a blood clot in the lung may experience cerebral circulatory problems. Such patients often have:
- fainting;
- convulsions;
- dizziness;
- coma;
- hiccups
Sometimes the described symptoms may be accompanied by signs of acute renal failure.
Blood clot in the lungs: survival rate, consequences in adults
A blood clot in the lungs is a dangerous phenomenon that can lead to death. The clot obstructs the movement of blood, causing disturbances in cardiopulmonary circulation.
Both factors independent of a person (heredity) and his lifestyle can contribute to the development of the disease. The process of blood clot formation occurs at a time of reduced physical activity.
When movement resumes, the thrombus detaches from the vascular wall and moves along the pulmonary artery. This can lead to dire consequences.
Causes of blood clot formation in the lungs
A blood clot in the lungs forms when favorable conditions are created in the cavity of the vessel. The main predisposing factor is increased blood clotting. Due to slow blood flow, it accumulates in certain areas of the vein, which leads to the appearance of a tumor.
Initially, the thrombus is attached to the wall of the vessel. Under the influence of certain factors, it breaks off, moving through the circulatory system.
The causes of the disease in adults are as follows:
- complicated course of varicose veins;
- postoperative period;
- suffering severe injuries;
- slow metabolism accompanied by excess weight;
- hereditary thrombophilia;
- long-term use of drugs that affect blood clotting;
- smoking and drinking alcoholic beverages.
Statistics show that people who have bad habits are most prone to thrombosis and thrombophlebitis . As you age, your risk of developing a blood clot increases.
This is due to inhibition of metabolic processes, which provokes changes in the vascular walls. In some cases, thrombosis develops as a result of poor nutrition.
Symptoms
The signs and symptoms of the disease at the initial stages of its development are not sufficiently pronounced. Symptoms become noticeable when the process of destruction of the body has already begun. Treatment must be immediate. After a blood clot breaks off, complications and manifestations of thrombosis develop rapidly.
There are signs that you should pay attention to first:
- swelling of the veins in the neck;
- cough with blood discharge;
- paleness of the skin;
- painful sensations in the chest;
- increased body temperature;
- sudden shortness of breath;
- dizziness followed by fainting;
- lowering blood pressure;
- symptoms characteristic of takardia.
Symptoms of thrombosis appear only in 50% of cases. This is why diagnosing the pathological process is difficult.
Classification
Pulmonary thrombosis (PE) is classified depending on the degree of blockage of the vessel, the size of the blood clot, the nature of the blood circulation and the severity of symptoms.
Taking into account the localization of the clot, thrombosis is divided into the following types:
- embolism that occurred in the area of the main pulmonary arteries and pulmonary trunk;
- pathology at the level of segmental arteries;
- concentration of the clot in the area of the intermediate and lobar arteries.
Right, left and bilateral thrombosis are also distinguished, depending on which part of the lungs is affected.
Thrombosis causes a decrease or cessation of blood supply to certain areas of the lung, which can lead to a heart attack or infarction-pneumonia of the affected tissue.
Classification by type of symptoms is as follows:
- Acute cor pulmonale. The pathological process affects large and small vessels of the pulmonary artery. This causes severe shortness of breath, cardiogenic shock, and a decrease in blood pressure.
- Infarction pneumonia. The disease affects only the small vessels of the pulmonary artery. Intense pain in the sternum appears, shortness of breath increases when the person is in an upright position, hemoptysis appears and the heart rate increases.
- Unmotivated shortness of breath. This type of pathology represents a recurrence of thrombosis. It is accompanied by pronounced shortness of breath and a decrease in blood pressure.
Modern therapy
Conservative treatment methods are aimed at restoring lung perfusion. Measures are also taken to prevent complications, one of which is the chronic form of pulmonary hypertension.
Once the patient is admitted to intensive care, blood clots in the lungs are treated with medications or surgery. The pressure in the veins is also monitored. In case of acute respiratory failure, tracheal intubation is performed.
To reduce blood pressure and relieve symptoms of thrombosis, Eufillin solution is administered intravenously.
If the pressure does not exceed the limit of 100, the drug cannot be used. In case of development of infarction pneumonia, antibacterial therapy is prescribed.
If clot therapy is insufficiently effective, a surgical intervention method is selected. Most often, a vena cava filter is installed in the vascular cavity. It blocks the blood clot from reaching the arteries of the lungs. The filter is inserted through the skin surface in the thigh or kidney area.
Long trips during which a person is in one position can contribute to a slowdown in venous blood flow. Drivers, machinists, travelers, etc. are at risk.
Preventive measures
Preventive measures are divided into secondary and primary. In the first case, we are talking about preventing relapse of the disease. By primary we mean measures taken when a person is prone to thrombosis.
In this case, it is recommended to follow the following principles:
- It is necessary to ensure an active lifestyle: periodically play sports, take walks, spend more time in the fresh air.
- If there is increased blood clotting, it is necessary to take medications to thin it.
- It is important to avoid foods high in cholesterol. This will avoid deterioration of the structure of blood vessels.
- It is necessary to regularly monitor blood clotting, glucose and cholesterol levels in the blood.
- Inflammatory processes and infectious diseases should be eliminated in a timely manner. They can become an impetus for the development of thrombosis.
- Drinking strong alcoholic drinks and smoking is strictly prohibited.
- For varicose veins of the lower extremities, pneumocompression of the legs should be performed, which helps eliminate swelling.
After treatment against thromboembolism, people live for a long time. But in this case, it is necessary to be observed by a doctor to prevent relapse of the disease.
Pulmonary thrombosis is surpassed only by cardiac ischemia and stroke in the number of deaths.
With relapses of the disease, the probability of death increases several times.
Complications of pulmonary embolism
A pathology in which a blood clot is localized in the lungs is extremely dangerous. The consequences for the body can be very diverse. It is the complication that arises that determines the course of the disease, the quality and life expectancy of the patient.
The main consequences of pulmonary embolism are:
- Chronically increased pressure in the pulmonary vessels.
- Pulmonary infarction.
- Paradoxical embolism in the vessels of the systemic circle.
However, not everything is so sad if blood clots in the lungs are diagnosed in a timely manner. The prognosis, as noted above, is favorable if the patient receives adequate treatment. In this case, there is a high chance of minimizing the risk of unpleasant consequences.
Below are the main pathologies that doctors diagnose as a result of complications of pulmonary embolism:
- pleurisy;
- pulmonary infarction;
- pneumonia;
- empyema;
- lung abscess;
- renal failure;
- pneumothorax.
Prevention
Necessary to reduce the likelihood of developing pulmonary embolism in the following cases:
- in the presence of chronic heart failure;
- women who take hormonal contraceptives for a long time;
- for systemic pathologies of connective tissue, vasculitis, diabetes mellitus, oncology, obesity;
- people who are on long-term bed rest;
- when using large doses of diuretics or the need to take them for a long time;
- after spinal cord injuries, stroke;
- when installing a central catheter into a vein for a long time.
For prophylactic purposes, the prescription of low molecular weight Heparin is indicated; after suffering from pulmonary embolism, antiplatelet agents are prescribed. The duration of treatment is determined by the doctor.
With timely diagnosis and treatment of pulmonary embolism (except for the fatal form), the prognosis for life is favorable. If severe disturbances in the activity of the heart, blood vessels, or lungs occur, the mortality rate is about 35%. After an illness, patients should receive preventive anticoagulant treatment; in the absence of it, relapses are possible. The fulminant course of the disease ends in death within a few minutes.
Recurrent pulmonary embolism
This pathology can recur in patients several times throughout life. In this case, we are talking about a recurrent form of thromboembolism. About 10-30% of patients who have had this disease once are susceptible to repeated episodes of pulmonary embolism. One patient may experience a different number of attacks. On average, their number varies from 2 to 20. Many past episodes of pathology represent blockage of small branches. Subsequently, this pathology leads to embolization of large arteries. A massive pulmonary embolism is formed.
The reasons for the development of a recurrent form can be:
- chronic pathologies of the respiratory and cardiovascular systems;
- oncological diseases;
- surgical interventions in the abdominal area.
This form does not have clear clinical signs. It is characterized by an erased flow. Correctly diagnosing this condition is very difficult. Often, unexpressed symptoms are mistaken for signs of other diseases.
Recurrent pulmonary embolism may be manifested by the following conditions:
- persistent pneumonia that has arisen for an unknown reason;
- fainting conditions;
- pleurisy that lasts for several days;
- attacks of suffocation;
- cardiovascular collapse;
- labored breathing;
- increased heart rate;
- elevated temperature that cannot be eliminated with antibacterial medications;
- heart failure, in the absence of chronic pathology of the lungs or heart.
This disease can lead to the following complications:
- emphysema;
- pneumosclerosis - lung tissue is replaced by connective tissue;
- heart failure;
- pulmonary hypertension.
Recurrent pulmonary embolism is dangerous because any subsequent episode can be fatal.
Classification
Pulmonary thrombosis (PE) is classified depending on the degree of blockage of the vessel, the size of the blood clot, the nature of the blood circulation and the severity of symptoms.
Taking into account the localization of the clot, thrombosis is divided into the following types:
- embolism that occurred in the area of the main pulmonary arteries and pulmonary trunk;
- pathology at the level of segmental arteries;
- concentration of the clot in the area of the intermediate and lobar arteries.
Right, left and bilateral thrombosis are also distinguished, depending on which part of the lungs is affected.
Thrombosis causes a decrease or cessation of blood supply to certain areas of the lung, which can lead to a heart attack or infarction-pneumonia of the affected tissue.
Classification by type of symptoms is as follows:
- Acute cor pulmonale. The pathological process affects large and small vessels of the pulmonary artery. This causes severe shortness of breath, cardiogenic shock, and a decrease in blood pressure.
- Infarction pneumonia. The disease affects only the small vessels of the pulmonary artery. Intense pain in the sternum appears, shortness of breath increases when the person is in an upright position, hemoptysis appears and the heart rate increases.
- Unmotivated shortness of breath. This type of pathology represents a recurrence of thrombosis. It is accompanied by pronounced shortness of breath and a decrease in blood pressure.
Diagnosis of the disease
The symptoms described above, as already mentioned, are not specific. Therefore, it is impossible to make a diagnosis based on these signs. However, with PE there are 4 characteristic symptoms:
- dyspnea;
- tachycardia - increased heart contractions;
- chest pain;
- rapid breathing.
If a patient does not have these four signs, then he does not have thromboembolism.
But not everything is so easy. Diagnosis of the pathology is extremely difficult. To suspect pulmonary embolism, the possibility of developing the disease should be analyzed. Therefore, the doctor initially pays attention to possible risk factors: the presence of a heart attack, thrombosis, surgery. This allows you to determine the cause of the disease, the area from which the blood clot entered the lung.
Mandatory examinations to identify or exclude PE are the following studies:
- ECG. A very informative diagnostic method. An electrocardiogram gives an idea of the severity of the pathology. If you combine the information obtained with your medical history, PE is diagnosed with high accuracy.
- X-ray. This study is not very informative for making a diagnosis of pulmonary embolism. However, it is precisely this that allows one to distinguish the disease from many other pathologies that have similar symptoms. For example, from lobar pneumonia, pleurisy, pneumothorax, aortic aneurysm, pericarditis.
- Echocardiography. The study allows us to identify the exact location of the blood clot, its shape, size, and volume.
- Lung scintigraphy. This method provides the doctor with a “picture” of the pulmonary vessels. It clearly shows areas of impaired blood circulation. But it is impossible to detect the place where blood clots are located in the lungs. The study has a high diagnostic value only for pathology of large vessels. It is impossible to identify problems in small branches using this method.
- Ultrasound of leg veins.
If necessary, the patient may be prescribed additional research methods.
Symptoms of the disease
Pulmonary thrombosis usually manifests itself with the following symptoms:
- Severe chest pain.
- Tachycardia and shortness of breath.
- Constant dizziness to the point of loss of consciousness.
- A sharp drop in vascular tone.
- Skin color changes. She becomes pale. Sometimes bluish areas are found.
- A person develops psychological problems associated with the fear of sudden death.
Symptoms of the disease are usually pronounced. They should never be ignored. Timely assistance can protect a person from sudden death. That is why, at the first signs of thromboembolism, you should immediately call an ambulance.
Urgent help
It should be remembered that if a blood clot breaks loose in the lungs, the patient’s symptoms can develop at lightning speed. And just as quickly lead to death. Therefore, if there are signs of pulmonary embolism, the patient should be given complete rest and a cardiac ambulance should be immediately called. The patient is hospitalized in the intensive care unit.
Emergency care is based on the following measures:
- Emergency catheterization of the central vein and administration of the drug "Reopoliglyukin" or a glucose-novocaine mixture.
- Intravenous administration of drugs is carried out: Heparin, Dalteparin, Enoxaparin.
- The pain effect is eliminated by narcotic analgesics, such as Promedol, Fentanyl, Morin, Lexir, Droperidol.
- Oxygen therapy.
- The patient is administered thrombolytics: Streptokinase and Urokinase.
- In cases of arrhythmia, the following drugs are used: Magnesium Sulfate, Digoxin, ATP, Ramipril, Panangin.
- If the patient has a shock reaction, he is administered Prednisolone or Hydrocortisone, as well as antispasmodics: No-shpu, Eufillin, Papaverine.
Pulmonary artery thrombosis
According to statistics, pulmonary artery thrombosis is detected in 1-2 people per 1000 population annually. And in most cases, the diagnosis is posthumous, because with the rapid development of the problem, the patient has little chance of surviving until a diagnosis is made, and thrombosis of small arteries is very difficult to diagnose, since its symptoms are similar to many other serious diseases, including myocardial infarction, heart failure, pneumonia, etc.
Ways to combat pulmonary embolism
Resuscitation measures can restore blood supply to the lungs, prevent the patient from developing sepsis, and also protect against the formation of pulmonary hypertension.
However, after first aid is provided, the patient needs continued treatment. The fight against pathology is aimed at preventing relapses of the disease and completely resolving the blood clot.
Today, there are two ways to eliminate blood clots in the lungs. Treatment methods for pathology are as follows:
- thrombolytic therapy;
- surgical intervention.
Pulmonary artery thrombosis
According to statistics, pulmonary artery thrombosis is detected in 1-2 people per 1000 population annually. And in most cases, the diagnosis is posthumous, because with the rapid development of the problem, the patient has little chance of surviving until a diagnosis is made, and thrombosis of small arteries is very difficult to diagnose, since its symptoms are similar to many other serious diseases, including myocardial infarction, heart failure, pneumonia, etc.
Thrombolytic therapy
Drug treatment is based on drugs such as:
- "Heparin";
- "Streptokinase";
- "Fraxiparin";
- tissue plasminogen activator;
- "Urokinase."
Such drugs help dissolve blood clots and prevent the formation of new clots.
The medicine "Heparin" is administered to the patient intravenously for 7-10 days. At the same time, blood clotting indicators are carefully monitored. 3-7 days before the end of treatment, the patient is prescribed one of the following drugs in tablet form:
- "Warfarin";
- "Thrombostop";
- "Cardiomagnyl";
- "Thrombo ACC".
Monitoring of blood clotting continues. Taking the prescribed pills lasts (after suffering from pulmonary embolism) for about 1 year.
Medicines “Urokinase” and “Streptokinase” are administered intravenously throughout the day. This manipulation is repeated once a month. Tissue plasminogen activator is also used intravenously. A single dose should be administered over several hours.
Thrombolytic therapy is not given after surgery. It is also prohibited in the case of pathologies that may be complicated by bleeding. For example, peptic ulcer. Because thrombolytic drugs can increase the risk of bleeding.
Modern therapy
Treatment of the disease should be aimed at restoring lung perfusion. In addition, with the help of therapy, it is necessary to prevent thrombosis and the occurrence of complications in the form of chronic pulmonary hypertension.
If doctors suspect pulmonary embolism, the patient should be placed on bed rest, which will make it possible to avoid recurrence of the disease. When the patient is hospitalized, central venous catheterization is performed to ensure effective treatment and monitoring of venous pressure. In the presence of acute respiratory failure, tracheal intubation is appropriate.
If a person complains of thrombosis and severe pain, the circulation should be expanded. To do this, the patient must take special narcotic analgesics. For example, Morphine solution, which can relieve an attack of shortness of breath. People who have a pulmonary thrombus, shock or arterial hypotension must immediately administer Reopoliglucin. But here the readings of central venous pressure should be taken into account: if they are too high, then the drug should not be administered.
Read also: How to cure varicocele of the left testicle without surgery
In order to reduce blood pressure and remove some symptoms, doctors prescribe Eufillin intravenously. But, again, if the upper pressure scale shows a figure less than 100, then the drug cannot be used. For infarction pneumonia, treatment with antibiotics is appropriate.
To restore arterial patency, modern medicine uses conservative and surgical therapy.
Conservative treatment includes thrombolysis and measures to prevent relapse of the disease. This suggests that therapy should be carried out until blood flow through the pulmonary arteries is restored.
Such treatment is appropriate when the doctor has fully established the diagnosis and taken control of the treatment process. But here some contraindications should be taken into account: the first week after surgery, treatment of chronic diseases, the presence of tuberculosis, hemorrhagic diathesis or varicose veins in the esophagus.
For a person who cannot undergo thrombolytic therapy due to the presence of a pulmonary blood clot, doctors recommend getting rid of the problem surgically. In addition, the specialist may prefer to install a vena cava filter in the vessels. These filters are substances that delay thrombosis and block its access to the arteries of the lungs. The filter is inserted through the skin on the femoral or renal veins.
Surgery
This question arises only when a large area is affected. In this case, it is necessary to promptly remove the localized blood clot in the lungs. The following treatment is recommended. A special technique is used to remove the blood clot from the vessel. This operation allows you to completely remove the obstacle to blood flow.
Complex surgical intervention is carried out if large branches or the trunk of the artery are blocked. In this case, it is necessary to restore blood flow over almost the entire area of the lung.
Treatment
If a blood clot in the pulmonary artery is suspected, and especially if it is assumed that it has broken off and is traveling, the patient requires urgent medical care, since negative symptoms develop at lightning speed. Delay in this situation is fraught with irreversible consequences.
Providing urgent assistance
Preventing death directly depends on the timeliness of emergency measures carried out in the intensive care unit.
The treatment algorithm includes the following measures:
- Connecting a catheter to the central vein.
- Intravenous administration of Reopoliglucin or a mixture of Glucose and Novocaine.
- This is followed by intravenous administration of Heparin, Enoxaparin or Dalteparin.
- In order to eliminate intense pain, painkillers with narcotic effects are used. The most effective of them are Fentanyl, Droperidol and Lexir.
- Next, oxygen therapy is carried out, which involves the administration of thrombolytics - Urokinase or Stretokinase.
- Symptoms of arrhythmia are eliminated by Digoxin, Magnesium Sulfate, Panangin or Ramipril.
- A state of shock requires the administration of Hydrocortisone or Prednisolone.
- To relieve vascular spasms, No-Shpa, Papavarin, and Euphellin are used.
Carrying out resuscitation measures helps stabilize blood circulation in the lungs, preventing the likelihood of developing sepsis and pulmonary hypertension.
Urgent care is the first stage of therapeutic measures. To treat pulmonary thrombophlebitis, a long course of therapy will be required.
Further treatment
After eliminating the acute condition, treatment continues with the goal of finally dissolving the blood clot and preventing the likelihood of relapse of the pathological process.
Continuation of treatment measures is carried out using two methods. This is thrombolytic drug therapy or surgery.
Conservative treatment
The main focus of the treatment course is to dissolve existing clots and prevent the formation of new blood clots. Treatment proceeds according to the following scheme:
- Intravenous administration of Heparin, Fraxiparine, Urokinase, Streptokinase. Course duration is from 7 to 10 days. These drugs require mandatory monitoring of indicators that reflect blood clotting.
- 3-4 days before stopping Heparin therapy, thrombolytic drugs are added to the treatment regimen - Cardiomagnyl, Warfarin, Thrombostop. The duration of treatment is about a year.
- Use of tissue-based plasminogen activator.
Thrombolytics are not prescribed after surgical treatment and the presence of pathological conditions accompanied by the likelihood of bleeding.
Surgery
The indication for surgical intervention is massive lung damage, accompanied by blockage of blood flow in large branches or the trunk of the artery by a thrombus.
This situation requires immediate removal of the clot from the blood vessel in order to restore blood circulation, which has been disrupted in almost the entire lung.