The brain (BM) is the most important organ, the center of the nervous system. When problems or pathologies arise in it, all organs and systems suffer. There are many GM diseases. Medicine cannot yet combat some of them, but it is quite possible to influence the course of the pathology. Other ailments are quite treatable.
Based on the nature of the underlying cause, pathologies are divided into diffuse and focal brain lesions. The first are characterized by homogeneity. Typically, pathologies develop gradually, spreading to all living cells. A similar phenomenon can be observed in case of circulatory disorders, head injury, and viral infections. The main difference between diffuse and focal is the presence of chronic fatigue, apathy, pressing pain in the brain along the entire circuit, drowsiness, the functioning of the sensory organs is disrupted, and performance decreases.
It is impossible to make an accurate diagnosis based on the clinical picture and patient complaints. To determine the type of lesion, it is necessary to undergo diagnostics. The most informative method is computed tomography.
Clinical picture
A variety of symptoms may indicate focal brain lesions.
- Headache. Most often they appear suddenly, for no apparent reason. They are intense, reminiscent of a migraine. The pain may surround or be localized on one or both sides of the brain.
- Blood pressure increases. With focal damage, an increase in blood pressure indicates that the body is trying to compensate for the lack of nutrition that occurred due to vascular dystrophy of the brain.
- There is impairment of hearing, vision, and coordination of movement.
- Memory deteriorates, fatigue increases, and weakness appears.
- There is nausea and vomiting, which does not bring relief.
- Fainting conditions.
- Tremor of the limbs, convulsions, in some cases paralysis.
- Loss of reflexes.
- Breathing is impaired.
- A person is disturbed by psycho-emotional disorders, stress, and irritability increases.
Epileptic seizures and strokes may occur, which directly indicate the presence of focal brain damage. All these symptoms may be pronounced or may not appear at all.
Any clinical signs of the disease are associated with neurology, since nerve tissue is affected in focal lesions, which causes changes in autonomic function.
Symptoms of focal brain damage
Clinical manifestations directly depend on the location of the pathological focus.
Frontal lobe defects provoke motor dysfunction, which is characterized by:
unsteadiness of gait;- paresis or paralysis of individual muscle groups or limbs (usually unilateral);
- muscle rigidity;
- nystagmus, strabismus, visual disturbances;
- epileptic paroxysms;
- psychoemotional disorders.
Patients retain the skills acquired throughout life, but are not able to apply them in practice.
Deviations in the functioning of the limbic system are manifested by symptoms:
- memory impairment;
- loss of ability to remember;
- state of apathy;
- inability to distinguish odors;
- cognitive dysfunction.
With disorders in the parietal lobe, patients complain of:
- changes in tactile and temperature sensitivity;
- phantom sensations of non-existent limbs, or the inability to recognize one’s own body parts;
- loss of reading, counting and writing skills.
Patients are unable to recognize familiar objects by touch, but recognize them through eye contact. In addition, they become disoriented in space and have difficulty finding certain places.
Temporal lobe defects are expressed by:
- hearing loss while maintaining normal ear anatomy;
- auditory hallucinations;
- inability to perceive words or music;
- memory loss, frequent repetitions of situations;
- epileptic paroxysms, convulsions.
The presence of pathological foci in the occipital lobe causes:
- visual dysfunction;
- cortical blindness, in which the patient may deny the inability to see;
- inability to recognize objects through visual contact;
- visual illusions and visual hallucinations.
Cerebellar disorders are represented by impaired motor skills and coordination of movements. Patients experience:
- uncertainty and unsteadiness of movements when walking and performing simple actions;
- tremor of the limbs;
- difficulties with consistent rapid flexion and extension of joints;
- nystagmus.
Causes of GM damage
Focal lesions can be caused by a variety of reasons.
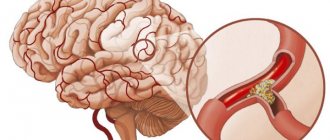
In case of focal lesions of the brain of a dyscirculatory nature, the cause may be a lack of nutrients caused by circulatory disorders (with ischemic heart disease, stroke and other pathologies). Often the cause of the disease is a neoplasm. It has a negative effect on neighboring areas of the brain, causing various changes in them, including the death of brain cells.
Causes of brain inflammation
The most common cause of brain inflammation is infection with the tick-borne encephalitis virus. The disease is transmitted not only through tick bites, but also through consumption of untreated milk from infected animals (for example, cows).
Other viral inflammations of the brain are caused mainly by herpes viruses, rubella, cytomegalovirus, and measles. A specific case is rabies, which in the absence of timely treatment always ends in the death of the patient.
Bacterial encephalitis is most often caused by meningococci and pneumococci . Less common are other bacterial infections, among which it should be noted (due to specific treatment) borreliosis and - today rare - tuberculosis.
Viral and bacterial infections are relatively common in Russia. In countries where there are no sources of clean drinking water and low levels of hygiene, a common cause of brain inflammation is protozoal infections (amoebas and toxoplasma) or parasites ( ascaris and tapeworm larvae ).
Inflammation of the brain may be a consequence of the body's protective reaction. Isolated cases of this type of inflammation relate mainly to young women with ovarian tumors. When fighting cancer cells, the body produces antibodies, which also attack nerve cells and cause diseases of the peripheral nervous system.
Very rarely there are cases of brain inflammation in acute sclerosis (demyelinating disease occurs in children, mainly due to infection).
What else leads to illness?
Focal pathologies can be caused by traumatic brain injuries, hematomas, and edema.
The following can also lead to the development of lesions:
- Spinal pathologies. One of the most common causes is osteochondrosis, in which nerves and blood vessels are compressed. As a result, an insufficient amount of blood enters the brain, cell nutrition is disrupted, and lesions of the brain arise.
- Fractures of the cervical spine. Within the neck there are two large vessels. When fractured, they can be damaged (torn, compressed). Impaired blood flow in the cervical region leads to inhibited blood supply to the brain. As a result, cells suffer from a lack of oxygen and nutrients.
- Excess weight. This reason is considered secondary. Obesity can lead to impaired brain function. Obesity with lack of physical activity is especially dangerous.
- Atherosclerosis. With this pathology, cholesterol plaques form in the vessels. They clog the lumen of the vascular bed, which leads to a lack of nutrients.
- Endocrine pathologies.
Modern approaches to therapy
Treatment should be aimed at the underlying disease that led to brain disorders. In addition, it is necessary to use means to prevent the progression of the disease.
Vascular agents such as pentoxifylline, vinpocetine, cinnarizine, and dihydroergocriptine are mandatory prescribed. They have a positive effect on cerebral circulation, normalize microcirculation, increase the plasticity of red blood cells, reduce blood viscosity and restore its fluidity. These drugs relieve vascular spasm and restore tissue resistance to hypoxia.
Cytoflavin, Actovegin, thioctic acid, piracetam, and ginkgo biloba are used as antioxidant, nootropic, and antihypoxic treatments.
Treatment with vestibulotropic drugs reduces dizziness, eliminates unsteadiness when walking, and improves the quality of life of patients. Treatment with betahistine, vertigogel, dimenhydrinate, meclozine, and diazepam is justified.
With high blood pressure, regular monitoring of blood pressure and heart rate numbers is necessary and their normalization according to indications. Aspirin, dipyridamole, clopidogrel, warfarin, and dabigatran are used to thin the blood. Statins are used to treat high blood cholesterol levels.
Currently, special attention is paid to calcium channel blockers, which, along with the function of normalizing blood pressure, have a neuroprotective effect. Cerebrolysin, Cerebrolysate, gliatilin, Mexidol restore cognitive functions well.
Neurotransmitters, for example, citicoline, have a nootropic and psychostimulating effect, normalize memory, attention, improve well-being, and restore the patient’s ability to self-care. The mechanism of action is based on the fact that the drug reduces cerebral edema, stabilizes cell membranes,
L-lysine escinate has anti-inflammatory, anti-edematous, and neuroprotective properties. Stimulates the secretion of glucocorticoids, restores vascular permeability, tones the veins and normalizes venous outflow.
to contents ^
Diagnostics
To identify pathological changes occurring in the brain, magnetic resonance imaging is performed. This is the only method to find out what exactly is happening under the skull, to see all the unfavorable processes in the structure of the brain, to assess the possible consequences and to make the most accurate prediction of the development of the disease. In the diagnosis of focal brain lesions, MRI is the “golden” method that can provide the most accurate assessment of the disease. It is non-invasive, fast and highly informative.
MRI allows you to determine the presence of a lesion, as well as conduct a comparative analysis of the obtained images with images of a healthy brain. On them, almost all lesions look like light spots of various sizes.
In addition, magnetic resonance imaging helps to accurately determine the number of lesions. Single changes in the brain are observed in all patients over the age of 50 years. In such cases, it is necessary to monitor the dynamics of the development of the lesion, as well as take measures to eliminate the causes of damage to the brain.
Perivascular spaces are dilated - what is it? Causes and treatment
If brain pathology is suspected, patients are prescribed magnetic resonance imaging. Often the study results indicate that the patient has dilated perivascular spaces. How dangerous is this? And what diseases could such a sign indicate? We will consider these questions in the article.
What it is
Perivascular spaces are located between the walls of blood vessels and the white matter of the brain. These formations are also called criblures or Virchow-Robin spaces. They are filled with cerebrospinal fluid and regulate the outflow of cerebrospinal fluid.
Normally, criblures are so small that they are not visible on an MRI image. However, there are cases when examination reveals expanded perivascular spaces. What does this diagnostic result mean? This suggests that criblures are visualized during an MRI examination. They look like white spots in the photo.
Causes
Enlarged perivascular Robin-Virchow spaces are not always a sign of pathology. This diagnostic result is also observed in completely healthy people. Most often, expansion of criblures is observed in elderly patients and is associated with age-related changes in the brain.
However, in some cases, dilated perivascular spaces may be a sign of the following diseases and conditions:
- brain atrophy;
- leukoaraiosis;
- cerebral ischemia (including cerebral infarction);
- disseminated encephalomyelitis.
In elderly people, expansion of criblures is often observed with hypertension, atherosclerosis, and dementia. These pathologies are usually accompanied by memory impairment and other cognitive impairment.
What to do if the MRI results indicate that you have dilated perivascular Virchow-Robin spaces? It is necessary to show the transcript of the study to a neurologist. Only a specialist can determine whether this is a variant of the norm, an age-related feature, or a sign of pathology.
There are cases when MRI does not reveal any changes in the brain, but the image shows dilated perivascular Virchow-Robin spaces. What does this mean? As a rule, such a sign does not indicate pathology. Doctors consider an increase in criblures only in combination with other changes identified during an MRI examination.
If necessary, the doctor may prescribe additional tests:
- multislice computed tomography;
- vascular angiography;
- Dopplerography;
- cerebrospinal fluid examination.
Let's take a closer look at the most common diseases and conditions that can lead to expansion of criblures.
If the patient’s perivascular spaces are expanded and the volume of the brain is reduced, then doctors talk about organ atrophy. Most often this is a sign of the following diseases:
- senile dementia;
- atherosclerosis;
- Alzheimer's disease.
In these diseases, neurons die. This is accompanied by memory impairment, mental impairment, and mental disorders. Typically, such diseases occur in elderly patients.
In some cases, dilated perivascular Virchow-Robin spaces are detected in newborns. This may be a sign of serious genetic diseases accompanied by the death of neurons.
How to treat such pathologies? After all, it is no longer possible to restore lost neurons. You can only slow down the process of death of nerve cells. Patients are prescribed the following drugs for symptomatic therapy:
- nootropics: “Piracetam”, “Cavinton”, “Nootropil”;
- sedatives: “Phenazepam”, “Phenibut”;
- antidepressants: Valdoxan, Amitriptyline.
The prognosis of such pathologies is usually unfavorable, as brain atrophy and neuronal death progress.
Leukoaraiosis
Doctors call leukoaraiosis a thinning of the white matter of the brain. Due to structural changes in the nervous tissue, patients have enlarged perivascular spaces. This is also a sign of diseases characteristic of older people:
- hypertension;
- atherosclerosis;
- senile dementia.
Changes in the white matter of the brain cause cognitive impairment. Patients are treated symptomatically with nootropic drugs. These drugs improve the nutrition of neurons and stop their death. For atherosclerosis, statins are indicated. For high blood pressure, antihypertensive drugs are prescribed.
Ischemic conditions
With ischemia, the blood supply to the brain deteriorates. This is usually a consequence of atherosclerotic changes in the vessels. The patient periodically experiences dizziness, double vision, motor coordination disorders, speech and memory disorders. Due to changes in the vessels, the spaces around their walls also expand.
Patients are prescribed nootropic drugs (“Piracetam”, “Cerebrolysin”, “Actovegin”), as well as drugs that normalize metabolism in brain cells (“Cortexin”, “Ceraxon”). In this case, it is very important to carry out etiotropic treatment of atherosclerosis with statins. The drugs Lovastatin, Atorvastatin, and Simvastatin are prescribed. This therapy eliminates the cause of ischemia.
Brain infarction
Often the perivascular spaces are dilated in patients who have suffered a cerebral infarction. This disease is a consequence of prolonged ischemia. In some cases, cerebral infarction is asymptomatic and goes unnoticed by the patient. Its consequences can only be seen in an MRI scan.
It is important to remember that if the patient has risk factors (high blood pressure, atherosclerosis, diabetes), then the heart attack may recur in severe form. To prevent a recurrent attack of acute ischemia, patients are prescribed antihypertensive medications, hypoglycemic agents, and blood thinners.
Disseminated encephalomyelitis
Disseminated encephalomyelitis (DEM) is an acute pathology of the central nervous system. In this disease, the myelin sheath of nerve fibers is destroyed. The perivascular Virchow-Robin spaces are dilated due to damage to the white and gray matter. The MRI image shows foci of demyelination.
This pathology is of autoimmune origin. The clinical picture of the disease resembles signs of multiple sclerosis. Patients experience gait and movement disturbances, speech disorders, dizziness, and inflammation of the optic nerve.
Unlike many other demyelinating diseases, REM is treatable. Patients are prescribed corticosteroids to suppress the autoimmune reaction:
- “Prednisolone”;
- “Dexamethasone”;
- “Metypred.”
After a course of therapy, 70% of patients experience complete recovery. In advanced cases, patients may still experience the consequences of the disease: impaired sensitivity of the limbs, gait disturbances, and visual disturbances.
Prevention
How to prevent the above pathologies? It can be concluded that older patients are more susceptible to such diseases. Therefore, all people over 60 years of age need to regularly visit a neurologist and undergo an MRI examination of the brain.
It is also important to constantly monitor blood cholesterol levels and blood pressure. After all, diseases accompanied by pathological changes in the white matter most often develop against the background of atherosclerosis and hypertension.
Source: //FB.ru/article/412408/perivaskulyarnyie-prostranstva-rashshirenyi—what-eto-takoe-prichinyi-i-lechenie
Numerous lesions
Patients who have multiple lesions deserve special attention. They are a sign of a serious pathology and may even serve as a symptom of a brain tumor. In the early stages, such diseases can only be detected after MRI.
If it is necessary to study blood vessels, an MRI with contrast is prescribed. As a result of the injection of a contrast agent, the blood is painted a different color, which is reflected in special shades on MRI images. When analyzing them, the doctor sees how blood flows through the vessels, in what directions and whether there are damages, blood clots, or aneurysms.
Discirculatory changes
Focal changes in the white matter of the brain due to impaired vascular trophism are the most common occurrence when analyzing MRI scans in older patients. They are considered to be caused by chronic hypoxia and dystrophy due to damage to small arteries and arterioles.
decreased blood flow is one of the main causes of age-related changes in the brain
MRI signs of vascular lesions:
- Multiple focal changes in white matter, mainly in the deep structures of the brain, not involving the ventricles and gray matter;
- Lacunar or border areas of necrosis;
- Diffuse lesions in the deep sections.
foci of lacunar microstrokes in the brain
The described picture may resemble that of age-related atrophy, therefore it can be associated with dyscirculatory encephalopathy only if the corresponding symptoms are present. Lacunar infarctions usually occur against the background of atherosclerotic lesions of cerebral vessels. Both atherosclerosis and hypertension give similar changes on MRI in a chronic course, can be combined and are characteristic of people after the 50th birthday.
Diseases accompanied by demyelination and a diffuse dystrophic process often require careful differential diagnosis, taking into account symptoms and medical history. Thus, sarcoidosis can simulate a variety of pathologies, including multiple sclerosis, and requires contrast-enhanced MRI, which shows characteristic focal changes in the basal ganglia and meninges.
In Lyme borreliosis, the most important facts are a tick bite shortly before the onset of neurological symptoms and a skin rash. Focal changes in the brain are similar to those in multiple sclerosis, measure no more than 3 mm and are combined with changes in the spinal cord.
Types of lesions
There are several types of focal GM diseases. The most dangerous are neoplasms. In the early stages, brain tumor symptoms can be confused with migraines and other illnesses. But with growth, the functioning of neurons deteriorates and signal transmission to the brain is disrupted. If the tumor grows, it begins to invade more and more new territories, and the clinical picture begins to increase.
Another type of focal disease is a cyst (a small cavity with liquid contents). For a long time, cavities do not make themselves felt until they begin to grow and increase in size. Despite the fact that they are not prone to growth and increase in size, like neoplasms, they are also considered a foreign body. Cysts can cause compression of blood vessels, which complicates the flow of blood to the brain.
Foci of damage are observed with necrosis. As a result of any previous infections or other diseases, areas of brain cells die without receiving the nutrition they need. Necrosis is dangerous because it entails irreversible changes.
Dangerous focal lesions of the white matter of the brain are intracerebral scars and hemorrhages. Most often they are the result of injuries, falls, blows. These types of foci lead to changes in the composition of the substance.
Any focal brain lesions of vascular origin lead to the destruction of brain cells and can lead to coma.
Natural degeneration during aging
Focal changes in the brain substance of a dystrophic nature against the background of age-related involution are represented by MRI signs:
- Periventricular (around the vessels) “caps” and “stripes” - found outside the lateral ventricles, arising due to the breakdown of myelin and expansion of the perivascular spaces, proliferation of glial cells under the ependyma of the ventricles;
- Atrophic changes in the hemispheres with expansion of the grooves and the ventricular system;
- Single focal changes in the deep white matter.
Multiple focal changes of a discirculatory nature have a characteristic deep location in the white matter of the brain. The described changes will be more pronounced, and the symptoms of encephalopathy will progress with age-related hypertension.
changes in the brain with age (younger → older): leukoaraiosis around the ventricles of the brain, atrophy, focal changes
Depending on the prevalence of age-related changes, the following are distinguished:
- Mild degree - single focal changes in the white matter of point sizes in the deep parts of the brain;
- Middle - drainage pockets;
- Severe - large confluent, scattered foci of damage to nervous tissue, mainly in deep sections against the background of vascular disorders.