Varieties
Cerebrovascular disease, or CVD for short, is associated with increasing damage to brain structures. As a rule, it occurs due to pathology of the cerebral vessels and causes a lack of blood supply and oxygen. Most often, CVD is detected in older people, but occasionally occurs in children.
The disease develops slowly, but already in the early stages the brain begins to experience a lack of oxygen due to impaired vascular function. During the transition to the chronic form, all parts of the brain are affected, and at first the pathological changes in the tissues are temporary, transient, but over time they become persistent and sometimes irreversible.
Information: CVD can lead to the development of discirculatory encephalopathy, in which diffuse and/or focal brain damage is observed. CVD is classified into acute, temporary and chronic.
Acute cerebrovascular insufficiency (ACVI) includes:
- encephalopathy type hypertension;
- ischemic attacks;
- strokes.
Chronic forms of CVD include the following:
- embolism due to blockage of blood vessels by blood clots;
- bleeding due to rupture of the walls of blood vessels, which can provoke a hemorrhagic stroke;
- thrombosis.
Temporary cerebrovascular insufficiency is, first of all, hypertensive cerebral crisis and TIA - transient ischemic attacks.
Mechanism of development of cerebrovascular disease
Disruption of the blood supply to the brain tissue within a few seconds causes ischemia of its cells. If blood flow is not restored within a few minutes, a heart attack develops, followed by necrosis—the death of cells. When insufficient cerebral circulation persists for a longer period, it can lead to infarction in the border zones (areas of poor blood supply between the main branches of the cerebral artery).
Areas of brain tissue with blood flow less than 10 ml/100 g tissue/min are the most damaged areas, as cells here die within minutes of a stroke. The “ischemic penumbra” zone with a blood flow of more than 25 ml / 100 g of tissue / min continues to function for a longer time (several hours).
An ischemic wave of disorders occurs where there is an energy problem due to lack of oxygen and nutrients. The cascade of damage results in decreased production of adenosine triphosphate, or ATP, which is a high-energy molecule needed for cell function in the brain. ATP consumption continues despite insufficient production, this leads to a decrease in its total amount and the development of lactic acidosis. In this pathological condition, ion homeostasis in neurons is disrupted.
Thus, the mechanisms of ischemic damage and stroke development are triggered. The ion pumps no longer transport Ca2+ out of the cells, which in turn causes the release of glutamate, which prevents calcium from passing through the cell walls. Eventually, apoptosis is initiated and cell death occurs.
In severe cases, global hypoxia-ischemia causes widespread traumatic brain injury, leading to significant cognitive complications called hypoxic-ischemic encephalopathy.
Causes
Arterial hypertension and atherosclerosis are the main causes of CVD. With increased pressure, blood vessels narrow, and brain cells do not receive the required amount of nutrition and oxygen. And the greater the lack of the latter, the higher the risk of developing a stroke - an acute disorder of cerebral circulation.
Blood clots (thrombi) can cause the disease.
With atherosclerosis, blood vessels become clogged with cholesterol plaques, narrowing the lumen. As a result, their “throughput” capacity decreases.
The table shows the causes and provoking factors of CVD:
| Causes | Risk factors |
| Congenital or acquired heart defects | Constant neuropsychic overload |
| Thrombosis | Excessive weight |
| Poor blood clotting | Diabetes |
| Vasculitis | Gout |
| Vascular ischemia | Osteochondrosis of the cervical spine, smoking |
The likelihood of the disease increases if there is a hereditary predisposition or metabolic disorder. The risk group also includes menopausal women and the elderly.
Necessary prevention
Prevention of chronic CVD, like treatment, comes down to eliminating risk factors or at least minimizing them. First of all this:
- healthy lifestyle;
- proper nutrition;
- physical activity (walking more than 30 minutes a day);
- giving up alcohol and smoking;
- continuous sleep of at least 7 hours a day;
- balance of work and rest;
- mental activity - the brain must work (crossword puzzles, learning new skills).
In case of a family history, regular preventive examinations are recommended.
In addition, timely treatment of hypertension (to minimize the occurrence of hypertensive crises), obesity, diabetes mellitus, atherosclerosis, and cardiovascular pathologies is necessary. It is recommended to attend clinical examinations, timely therapy and surgical treatment of vascular pathologies.
It is necessary to improve rehabilitation using not only drug treatment, but also physiotherapy, exercise therapy, and sanatorium-resort treatment. Psychotherapeutic support is also required.
Signs
Due to the slow and gradual development of CVD, it does not begin to manifest clinically immediately. Therefore, the first signs are rather vague, and they are often attributed to overwork and fatigue, without turning to doctors.
First symptoms:
- headaches and dizziness;
- mood swings, nervousness;
- decreased performance, fatigue;
- noise in ears;
- memory and sleep disturbance.
The cause of these manifestations can indeed be stress and various overloads. However, later they become more pronounced and attract attention.
Over time, motor disturbances appear, memory deteriorates sharply, and vascular crises periodically occur. Progression of the disease may lead to the development of vascular dementia, loss of control over the functioning of the excretory organs and other neurological symptoms, including extrapyramidal syndrome.
Signs of vertebrobasilar CVD
The most common form of chronic cerebrovascular insufficiency is its vertebrobasilar variety, which can be a consequence of not only atherosclerosis of the vertebral arteries, but also their deformation.
Reference: By deformation of the vertebral vessels we mean congenital hypoplasia, as well as pinching in diseases of the cervical spine.
The clinical picture of vertebrobasilar CVD includes the following symptoms:
- frequent dizziness, accompanied by nausea, sometimes vomiting;
- unsteady gait;
- headache in the back of the head;
- hearing loss, tinnitus;
- “veil” before the eyes, flashing of flies;
- memory loss;
- unexpected falls, most often without loss of consciousness.
Pseudobulbar syndrome
With pseudobulbar syndrome, there are problems with speech, swallowing function and voice, increased salivation, decreased control over the body's functions and mental disorders.
Psychopathological syndrome
Disturbances in the psychoemotional sphere to one degree or another are observed in almost 100% of patients. In the initial stages, this manifests itself as nervousness, irritability and unstable mood.
Subsequently, memory lapses occur and cognitive abilities are significantly reduced. About a quarter of patients with vascular dementia experience depression.
Symptoms
Acute cerebrovascular insufficiency is characterized by bright, rapidly growing symptoms. Ischemic stroke develops due to blockage of a blood vessel by an atherosclerotic plaque or thrombus or due to vasospasm. The blood cannot overcome the obstacle and oxygen starvation of the brain occurs.
In addition, cerebral edema begins almost immediately after the onset of ischemia. Hemorrhagic stroke occurs when a vessel ruptures or increased permeability of the vascular wall and blood enters the brain. In both cases, the affected part of the brain dies, which causes certain symptoms.
All symptoms of acute cerebrovascular disorders can be divided into general cerebral, characteristic of any type of cerebral circulatory disorder, and focal, which depend on where exactly the pathological focus is localized. Typically, with a hemorrhagic stroke, general cerebral symptoms are more pronounced, while with an ischemic stroke, focal symptoms are more pronounced.
General cerebral symptoms include:
- Dizziness;
- Strong headache;
- Nausea and vomiting. Vomiting does not bring relief to the patient, which distinguishes it from vomiting in diseases of the gastrointestinal tract and poisoning;
- Confusion. Patients sometimes do not remember where they are and do not recognize their relatives. This condition can either pass quickly or last for a long time;
- If the cerebrovascular disorder is severe, there may be loss of consciousness or even coma;
- If the patient remains conscious, psychomotor agitation may occur.
Focal symptoms depend on which part of the brain is affected:
- If there is a circulatory disorder in the anterior cerebral artery, paresis is observed on the side opposite to the pathological focus. Moreover, this is more often noticeable on the lower limb, since paresis of the arm quickly passes;
- There may be urinary incontinence;
- The patient staggers when walking;
- There is increased or decreased sensitivity of the skin on the face and hands;
- Cerebrovascular insufficiency of the brain may be accompanied by speech disorders: a person may understand what is said to him, but is not able to answer;
- If you ask the injured person to stick out his tongue, you may notice that he deviates to the side;
- Very often there are disturbances in the sense of smell and changes in the human psyche;
- The patient is unable to perform any purposeful actions;
- Sometimes memory lapses occur;
- In severe cases, paralysis of the limbs may occur.
Acute cerebrovascular diseases require immediate medical attention! Treatment must be started in the first hour after the lesion, otherwise the risk of death or disability of the patient increases with every hour.
Unlike the acute form, the symptoms of chronic cerebrovascular insufficiency develop slowly. There are three stages of disease development.
- Stage 1 – initial. At this stage, patients may notice rapid fatigue and decreased performance. They become less attentive and complain of memory deterioration. Mild motor disturbances and changes in skin sensitivity may be observed, which quickly disappear.
- Stage 2 - with further progression of the disease, the symptoms of stage 1 CVD intensify: memory and performance decrease even more, the patient gets tired very quickly, irritability and changes in character are observed. In addition, there are other signs of impaired blood supply to the brain. The gait changes: it becomes heavy, shuffling or mincing. Coordination of movements is impaired, oculomotor changes appear.
- Stage 3 – cerebrovascular syndrome becomes pronounced. Coordination of movements, memory are severely impaired, and mental abilities are reduced. Sometimes fainting and epileptic-type seizures may occur. At this stage, patients most often need the help and care of others, in rare cases still remaining competent.
Stages
Cerebrovascular disease goes through 3 stages. Stage 1 is characterized by asthenoneurotic, oculomotor and coordination disorders, asymmetry of reflexes, and mild signs of oral automatism.
At stage 2, memory problems worsen, performance decreases noticeably, gait changes, and symptoms of oral automatism intensify.
At the 3rd stage, a pronounced amyostatic symptom complex appears - movements become slow and inexpressive, muscle tone gradually increases, and small tremor (shaking) is often observed.
Psychoorganic syndrome is expressed in weakened memory, decreased intellectual abilities, and inadequate emotional reactions. In addition, there are signs of pyramidal insufficiency - in fact, paralysis or paresis with the following symptoms:
MRI of cerebral vessels
- strength in the leg muscles decreases;
- fine motor skills of the fingers deteriorate, and the person cannot, for example, play musical instruments, sew or embroider;
- the muscles become hypertonic and spasm, which is manifested by a typical gait when the legs have weakness and limited range of motion. “He can barely move his legs” - this is how the patient can be described;
- tendon reflexes increase - knees and elbows react sharply to the blows of the neurological hammer, literally jumping. If the patient suddenly bends the foot, convulsions begin in it - clonus;
- Skin - in particular, abdominal - reflexes decrease, and pathological ones appear.
CVD is a life-threatening disease that, in severe cases, ends in death
At the 3rd stage of cerebrovascular disease, pathological reflexes of Babinsky, Bekhterev, Rossolimo, Zhukovsky and Oppenheim may occur. With the Babinski reflex, the toes fan out when a light object is passed along the edge of the sole from bottom to top. A healthy person's fingers should bend.
Note: Patients with the third stage of CVD rarely remain fully competent.
Risk factors and prevention of ischemic cerebrovascular diseases
P
Prevention of ischemic cerebrovascular diseases is an urgent medical and social problem due to their widespread prevalence, high incidence of mortality and disability in ischemic stroke and vascular dementia.
Prevention is based on eliminating or weakening the effect of correctable risk factors for ischemic cerebrovascular diseases [1–7]. Table 1 presents the main risk factors for ischemic cerebrovascular diseases. Ischemic cerebrovascular accidents in approximately 90–95% of cases are caused by atherosclerosis of the cerebral and precerebral (carotid and vertebral) arteries
, damage to small cerebral arteries due to arterial hypertension, diabetes mellitus or cardiogenic embolism.
Atherosclerosis of the precerebral (carotid, vertebral) and cerebral arteries causes ischemic cerebral complications through various pathogenetic mechanisms. Atherothrombosis and arterio-arterial embolism account for about 50% of the causes of ischemic cerebrovascular accidents.
Main pathogenetic mechanisms
cerebral ischemia in atherosclerosis of precerebral and cerebral arteries:
- blockage of the precerebral or cerebral artery;
- hemodynamically significant stenosis of the precerebral or cerebral artery (narrowing of 70–75% or more of the lumen area of the artery);
- arterio-arterial embolism.
Heart diseases through the mechanism of cardiogenic embolism are the cause of about 20% of ischemic strokes and transient ischemic attacks.
Cardiogenic embolism usually occurs due to the formation of embolic fragments on the heart valves or the formation of an intracardiac thrombus. Risk factors for cardiogenic cerebral embolism are presented in Table 2. Arterial hypertension is the main correctable risk factor for ischemic cerebrovascular diseases
. Arterial hypertension leads to the development of ischemic brain damage through various pathogenetic mechanisms.
The main pathogenetic mechanisms of cerebral ischemia in arterial hypertension:
- development of changes in perforating arteries of the brain (lipohyalinosis, fibrinoid necrosis);
- increased atherosclerosis of large and medium precerebral (carotid, vertebral) and cerebral arteries;
- development of heart diseases (atrial fibrillation, myocardial infarction and others), complicated by cerebral embolism and chronic circulatory failure.
Damage to small perforating arteries of the brain, resulting from arterial hypertension, leads to the development of small lacunar infarctions, which account for 15–30% of all ischemic strokes.
In cases where no major risk factors for cerebrovascular disease are found in a patient with ischemic stroke or transient ischemic attack, it is necessary to exclude rare causes of ischemic cerebrovascular accidents, which are most common in young patients.
Rare causes of ischemic cerebrovascular accidents:
- vasculitis;
- hematological diseases (erythremia, sickle cell anemia, thrombocythemia, leukemia);
- immunological disorders (antiphospholipid syndrome);
- venous thrombosis;
- dissection of the carotid or vertebral artery;
- migraine;
- taking oral contraceptives;
- drug use.
As already noted, secondary prevention of stroke in persons who have suffered a transient ischemic attack or ischemic stroke is aimed at eliminating or reducing correctable risk factors for ischemic stroke.
The main directions of secondary stroke prevention:
- treatment of arterial hypertension;
- stopping or reducing smoking;
- diet and/or lipid-lowering medications;
- taking antiplatelet drugs;
- taking anticoagulants;
- carotid endarterectomy.
Treatment of arterial hypertension is one of the most effective areas of stroke prevention. The effectiveness of antihypertensive therapy in secondary prevention of stroke was convincingly proven in the recently completed PROGRESS
(Perindopril Protection Against Recurrent Stroke Study - a study of perindopril as a means of preventing recurrent stroke). It has been shown that the combination of perindopril (4 mg/day) and indapamide (2.5 mg/day), used for 5 years, reduces the risk of recurrent stroke by an average of 28%, and major cardiovascular diseases by 26%.
Quitting smoking is associated with a gradual, significant reduction in the risk of stroke
, and after 5 years of abstinence from smoking, the risk of developing a stroke in a former smoker is little different from the risk of developing a stroke in a person who has never smoked.
For patients who have suffered a transient ischemic attack or ischemic stroke, it is recommended to reduce fat intake to 30% of the total calorie intake and cholesterol to 300 mg per day
. For hyperlipidemia, a more strict diet is indicated (reducing fat intake to 20% of the total calorie intake and cholesterol to a level of less than 150 mg per day). In cases of severe atherosclerotic damage to the carotid and vertebral arteries, a very low-fat diet (reducing cholesterol intake to 5 mg per day) can be used to prevent the progression of atherosclerosis. If within 6 months of the diet it is not possible to significantly reduce hyperlipidemia, then it is recommended to take lipid-lowering drugs (lovastatin, simvastatin, pravastatin, etc.) in the absence of contraindications to their use.
One of the most effective areas of secondary prevention of stroke is the use of antiplatelet agents (Table 3).
The most commonly used is acetylsalicylic acid. Clopidogrel is prescribed in cases where acetylsalicylic acid is contraindicated or there are side effects from its use, or cardiovascular disease has occurred in a patient taking acetylsalicylic acid. A combination of acetylsalicylic acid and dipyridamole is effective. Because of the potential for bone marrow suppression, ticlopidine is rarely prescribed at present, but it should not be discontinued in patients who have already been taking it for a long time without side effects.
Indirect anticoagulants (warfarin in an average daily dose of 5 mg) are recommended for patients who have suffered ischemic cerebrovascular accident due to the mechanism of cardiogenic embolism. When treating with indirect anticoagulants, regular monitoring of blood prothrombin levels is necessary (it is recommended to reduce the prothrombin index to 50–60% or increase the international normalizing coefficient to 3.0–4.0). In cases where the use of warfarin is contraindicated or regular testing of prothrombin levels in the blood is impossible, the use of antiplatelet agents is recommended.
The main indications for the use of indirect anticoagulants for the purpose of secondary prevention of ischemic stroke:
- atrial fibrillation (atrial fibrillation);
- artificial heart valve;
- intracardiac thrombus;
- rheumatic heart valve disease;
- myxoma;
- recent (less than 1 month) myocardial infarction.
Carotid endarterectomy is indicated for severe stenosis (narrowing of 70–99% of the diameter) of the internal carotid artery in patients who have suffered a transient ischemic attack or minor stroke. It can also be performed for moderate stenosis (narrowing of 30–69% of the diameter) of the internal carotid artery in patients with mild or moderate neurological deficit after a stroke. However, the effectiveness of surgical treatment in these cases has not yet been proven. When deciding on surgical treatment, one should take into account not only the degree of carotid artery stenosis, but also the prevalence of atherosclerotic lesions and the presence of concomitant somatic diseases.
Algorithm for the management of patients after a stroke
Vascular dementia
is a chronic form of ischemic cerebrovascular diseases. The risk factors for the development of vascular dementia are the same as for acute ischemic cerebrovascular diseases; The leading role is given to arterial hypertension, which causes changes in small penetrating arteries of the brain and the development of lacunar infarctions or significant diffuse damage to the white matter of the brain.
In patients who have suffered a transient ischemic attack or ischemic stroke, the prevention of vascular dementia includes the previously described stroke prevention and the prescription of drugs that improve the patient’s cognitive functions. For this purpose, Cerebrolysin
20–30 ml IV in saline solution daily for a month, in courses for several months a year, or continuously
piracetam
1.6–4.8 mg/day,
vinpocetine
15–30 mg/day,
tanakan
120 –160 mg/day,
gliatilin
1200 mg/day,
nimodipine
30 mg 3-4 times a day and other drugs.
In recent years, double-blind placebo-controlled studies have been conducted that have proven the effectiveness of Actovegin
in improving cognitive functions in patients with cerebrovascular pathology. It has been shown that the use of Actovegin tablets 400 or 600 mg three times a day for 12 weeks has significant advantages over placebo in improving cognitive functions and well-being of patients, with a more pronounced effect noted in patients with mild cognitive disorders. Actovegin tablets are well tolerated by elderly patients and are suitable for long-term outpatient treatment. The algorithm for managing patients after a stroke is presented in the figure.
The use of scientifically proven methods for the prevention of stroke and vascular dementia in clinical practice can lead to a significant reduction in the incidence of stroke and disability in patients caused by motor and cognitive impairment.
Unfortunately, according to our data, only less than 10% of patients who have suffered a transient ischemic attack or ischemic stroke undergo adequate prevention of recurrent stroke and vascular dementia. This, on the one hand, explains the high incidence of cerebrovascular diseases at present; on the other hand, it indicates the potential for reducing the incidence of vascular pathology of the brain and preventing its progression. Literature:
1. Vibers D.O., Feigin V.L., Brown R.D. // Guide to cerebrovascular diseases. Per. from English M., 1999 – 672 p.
2. Vilensky B.S. // Stroke: prevention, diagnosis and treatment. St. Petersburg, 1999 – 336 p.
3. Damulin I.V., Parfenov V.A., Skoromets A.A., Yakhno N.N. // Diseases of the nervous system. Guide for doctors. Ed. Yakhno N.N., Shtulmana D.R., M., 2001, T.1, pp. 231–302.
4. Stroke. Practical guide for the management of patients // C.P. Warlow, M.S. Dennis, J. van Geyn et al. Trans. from English St. Petersburg, 1998 – 629 p.
5. Shevchenko O.P., Praskurnichy E.A., Yakhno N.N., Parfenov V.A. // Arterial hypertension and cerebral stroke. M., 2001 – 192 p.
6. Victor M., Ropper AH // Adams and Victor's principles of Neurology. New York. 2001, pp. 777–873.
7. Yatsu FM, Grotta JC, Pettigrew LC // Stroke. 100 Maxims. St. Louis, 1995 – 178 p.
Possible consequences
Severe forms of brain disorders are accompanied by the progress of irreversible changes, which entails mental, intellectual and neurological disorders. Fears and phobias appear, coordination of movements worsens, it becomes difficult to concentrate on something, etc.
The most dangerous consequences of CVD are stroke and Binswanger's disease, the symptoms of which correspond to stage 3 of brain failure. With a stroke, the symptoms are very variable, but they can be both reversible and irreversible.
Treatment
Comprehensive treatment of cerebrovascular disease begins with correction of the underlying disease that led to the development of CVD. For this purpose, doctors prescribe antihypertensive, hypoglycemic and anti-sclerotic medications. Next, specific drugs of several groups are prescribed:
- neuro- and angioprotectors – Cavinton, Tanakan;
- nootropics – Cerebrolysin;
- antihypoxants – Actovegin;
- antispasmodics – Papaverine, NoShpa, Dibazol;
- anticoagulants – Warfarin, Fraxiparine.
Therapy for CVB also includes amino acid agents and neurotransmitters - Glycine, Neuromidin, Choline alfo-scerate. Problems with decreased intelligence are solved with the help of anticholinesterase drugs and ginkgo biloba.
In case of dizziness and tinnitus, Betahistine 16 mg is used. Trental is prescribed to dilate blood vessels, and Aspirin is prescribed to thin the blood. If there are signs of heart failure, Pentamin is used.
Often it is enough to eliminate the provoking factor to stop or slow down the disease
In case of heart rhythm disturbances, taking Strophanthin or Korglykon is indicated. Neuropsychiatric syndromes are relieved with Haloperidol or Diphenhydramine. Furosemide and Mannitol are used for cerebral edema.
Clinical picture
There are several difficult aspects associated with a disease such as cerebral vascular crisis (its symptoms and treatment are interrelated). But if a non-specialist can recognize the symptoms, then the correct course of treatment, based on data from tests, examination, and various studies, can only be prescribed by a doctor with a higher education.
It is important for a potential patient to know that the first sign of a hypertensive crisis is headache. Sometimes it can be diffuse in nature (it is difficult to determine the source of pain), more often the pain is present in the occipital region. The higher the blood pressure and the more swelling of the brain, the worse the headaches will be.
There is a high probability that the patient has a cerebrovascular crisis - symptoms indicating vasogenic cerebral edema:
- nausea, vomiting;
- fear of light;
- disruption of the vestibular apparatus;
- disorders of the visual organs.
In the most severe cases, acute encephalopathy and seizures similar to epileptic ones are diagnosed. In some cases, disorientation in space, disturbance of the emotional background, and the appearance of excessive anxiety may be observed.
Signs of cardiac pathologies are quite common - palpitations, shortness of breath, pain in the heart area. Options include fainting, short-term disturbances of consciousness. High blood pressure can lead to facial flushing. The crisis is replaced by general weakness, the person feels overwhelmed, tired, and weak.
FAQ
What are pressure chambers used for? Oxygen therapy is performed in hyperbaric chambers to enrich the blood with oxygen and facilitate its “supply” to the tissues. Due to clean air in a special capsule, the cells are saturated with oxygen, thereby eliminating hypoxia.
What operations are performed for CVD? Severe forms of the disease are treated surgically using stenting, balloon angioplasty, extra-intracanal anatomy, and endarterectomy. A stent (metal or plastic structure) is installed in the stenting chord to widen the vessel.
Balloon angioplasty involves inserting a balloon into the narrowest part of the vessel, after which the balloon expands.
Endarterectomy is the removal of cholesterol plaques with subsequent restoration of the vascular wall damaged by them.
Extra-intracanal anamostosis is the connection of intra- and extracranial arteries with each other. This operation is performed in case of obstruction, narrowing of the vessel and the impossibility of its restoration in any other way.
Diagnosis of chronic cerebrovascular insufficiency
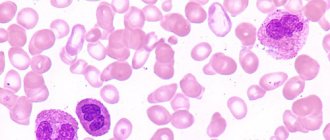
Laboratory examination consists of a clinical blood test to determine the level of platelets, red blood cells, hemoglobin, hematocrit, and leukocytes with a detailed leukocyte formula. An analysis of the lipid spectrum, blood clotting rate, and blood glucose levels is carried out.
Diagnosis of the disease is carried out mainly using instrumental methods:
- Dopplerography of cerebral vessels using ultrasound to detect vascular abnormalities;
- electroencephalography (EEG) of the brain, which allows you to study the activity of the cerebral hemispheres;
- CT scan of brain vessels of spiral type;
- MRI of the head to determine the extent of vascular and white matter damage;
- X-ray of the head with the introduction of contrast agents.
To confirm this diagnosis, examinations of the patient's neurological and psychological condition are also prescribed.
Physical studies are carried out to identify pathological processes in the cardiovascular system.
The following procedures are carried out:
- measurement of pulsation of blood vessels of the limbs and head;
- pressure at 4 points of the upper and lower extremities;
- ECG and ultrasound of the heart;
- auscultation of the heart and abdominal aorta for the presence of arrhythmia and murmurs;
- Dopplerogram of the cervical vessels to exclude stenosis of the carotid and cephalic arteries.