Development
Myocarditis in cardiology is called inflammation of the heart muscle. Cardiosclerosis is pathological damage to the muscle tissue of the heart, its replacement with connective scar tissue. Thus, postmyocardial cardiosclerosis is cardiosclerosis that developed as a result of myocarditis .
A synonymous, shorter name for this disease is myocardiosclerosis. According to the international classification of diseases, it does not belong to the group of atherosclerotic heart diseases, but is included in the heading “Heart lesions in other diseases.”
Prevention and prognosis
A poor prognosis is determined by the occurrence of an aneurysm or atrial fibrillation.
Prediction depends on the patient’s age, the course of the disease, a history of concomitant diseases, complications that arose during the illness, and the number of affected areas. A favorable prognosis is acceptable in the absence of disturbances in blood flow and heart rhythm. To prevent post-myocardial cardiosclerosis from occurring, it is recommended to undergo routine vaccination against dangerous infectious diseases. In this case, you should carefully prepare for the procedure, visit a doctor and undergo the necessary tests. All medications should be taken only as prescribed by a doctor. Existing provoking diseases should be kept in remission.
Causes and risk factors
The causes of myocarditis, which can lead to this disease, are quite well studied and have a very wide range. These include the following factors:
- Infectious:
- viral (ARVI, influenza, chicken pox, rubella);
- Allergic (after vaccination and drug therapy).
The use of antibiotics, cytostatics, antituberculosis and anticonvulsants, and nonsteroidal anti-inflammatory drugs is likely to cause immune reactions. - System .
As a result of general diseases of the connective tissue of the whole body (rheumatism, polyarthritis, systemic lupus erythematosus, etc.). - Toxic (uremic myocarditis).
- Idiopathic .
Causes unexplained by modern medicine that have characteristic clinical manifestations.
bacterial (scarlet fever, tonsillitis, diphtheria, pneumonia).
Microorganisms such as protozoa, helminths, spirochetes, and fungi can also cause inflammatory lesions of the heart.
Myocarditis caused by allergic and systemic causes is characterized by rapid progression of sclerotic changes.
There are also acute, subacute, latent, recurrent and chronic (lasting more than six months) course of the disease. It is chronic inflammation of the heart that most often leads to the occurrence of myocardiosclerosis.
This disease affects all age groups, including children and adolescents . Children and the elderly should be identified as a special risk group.
In children, the immune system is not yet fully developed, while in older people it is already quite weakened. This increases the possibility of infectious diseases, one of the main causes of myocardiosclerosis.
Causes of the disease
Postmyocardial cardiosclerosis is always a secondary disease. Most often it becomes a consequence of myocarditis. The reasons are the following factors:
- Infections - damage by Coxsackie viruses A and B, influenza, diphtheria, scarlet fever, hepatitis, adenovirus, herpes, CMV, ECHO, HIV, Epstein-Barr.
- Bacterial infections, especially beta-hemolytic streptococci gr. A. They have a special affinity for the tissues of the heart - they lead to rheumatism.
- Allergies.
- Toxic damage - antidepressant abuse.
- Thyrotoxicosis.
- Idiopathic myocarditis.
The disease can be caused by a heart attack, ischemia, myocardial dystrophy (occurs with anemia, hypoxia, etc.) According to ICD-10, the code for myocardial cardiosclerosis with rhythm disturbance is I20.0-I20.9.
Prevention of post-myocardial cardiosclerosis
To prevent the development of myocardiosclerosis, a patient who has had myocarditis must systematically visit a cardiologist, as well as a therapist, and undergo appropriate heart-supportive therapy.
Preventive examinations should be carried out at least 2 times a year.
If the first and minor symptoms of post-myocardial cardiosclerosis appear, it is necessary to immediately visit a cardiologist in order to conduct a full instrumental examination and promptly begin therapy for sclerosis of the heart muscle.
Self-medication, or simply ignoring the developing pathology of the heart, can lead to very sad consequences, which will end in a sudden heart attack with a fatal outcome.
It is possible to stop the progression of the pathology of postmyocardial cardiosclerosis by following the doctor’s instructions, as well as a properly selected diet.
The diet should include the maximum amount of vitamins and fiber found in fresh vegetables and fruits, as well as polyunsaturated fatty acids found in sea fish and vegetable oils.
The diet should not include fatty meats and eggs, full-fat dairy products and trans fats. Limiting sweet foods and the amount of salt consumed.
Also, the diet should not contain fried and smoked foods, as well as canned food and marinades. It is necessary to completely give up smoking, drugs and alcoholic beverages.
Constantly monitor the blood pressure index, as well as the index of cholesterol and glucose in the blood.
Avoid stress and overstrain of the nervous system. Do not overload the body physically, but also do not lead a sedentary lifestyle. Constantly fight obesity.
Treatment principles and prognosis
Treatment of this pathology, like any other heart disease, is a long and scrupulous process. The basic principles of treatment are listed below.
Thorough sanitation of foci of infection
What is this for? First of all, to prevent the occurrence of recurrent myocarditis. Sanitation of foci of infection includes treatment of caries, removal of sulfur plugs, treatment of cholecystitis, sinusitis, frontal sinusitis, etc. Even if these lesions do not make themselves felt, they can, under certain conditions, provoke the development of recurrent myocarditis.
Selection of antiarrhythmic drugs
Antiarrhythmic drugs are selected strictly individually in each specific case. The most widely used drugs in domestic medicine are propanorm, etacizin, and amiodarone. The listed drugs have many contraindications, so they are taken under the supervision of a cardiologist.
Treatment of heart failure
To eliminate and prevent further development of heart failure, the following groups of drugs are used:
- cardiac glycosides (digoxin),
- nitroglycerin preparations (cardiquet, nitroglycerin),
- ACE inhibitors (perindopril, ramilong),
- sortans (losartan),
- diuretics (pamid, furosemide),
- B-blockers (metoprolol, betaloc).
The patient should know that medications for the treatment of heart failure, as well as antiarrhythmic drugs, should be taken for life, without changing dosages or stopping them without a doctor’s prescription. The consequences of a “creative approach” to taking such drugs can be disastrous; heart failure can lead to disability and death. Twice a year, such patients are indicated for hospitalization in a cardiology hospital.
Treatment prognosis depends on the extent of the process. If a small area of cardiac tissue is affected, over time the process is somewhat compensated, but, unfortunately, it is impossible to completely abandon medications. Unfortunately, it is impossible to get rid of heart failure forever.
Post-infarction cardiosclerosis: causes, symptoms, diagnosis, how to treat, consequences
Postmyocardial cardiosclerosis appears against the background of an inflammatory process, medically called myocarditis. Pathology causes degradation of muscle tissue, instead of which connective tissue grows. But if the muscles are normally elastic and can contract, the connective tissues are not capable of this, so the functioning of the heart is complicated. Postmyocardial cardiosclerosis is associated with heart failure and arrhythmia. Postmyocardial cardiosclerosis is more often observed if myocarditis was triggered by allergies or systemic pathologies.
Note! Diagnosis and treatment are not carried out virtually!
Symptoms: how does pathology manifest itself?
The manifestation of the disease is expressed by symptoms such as the inability to take a full breath and cough.
Postmyocardial cardiosclerosis can be focal, when scar formations appear in certain areas of the heart muscle, and diffuse, in which sclerosis covers all tissues. The disease manifests itself as follows:
- heartache;
- orthopnea and cough;
- persistent hypotension;
- inability to take a full breath;
- heart rhythm disturbances (bradycardia or tachycardia);
- hyperhidrosis;
- constant cold and chilliness in the hands and feet;
- swelling of the lower and upper extremities;
- pale or bluish skin;
- weakness, fatigue even after minor physical exertion.
Symptoms and signs
In mild forms of myocarditis, the body itself can cope with the disease without causing any clinical manifestations. Peculiar symptoms, similar to many heart diseases , appear in the patient already at the stage of development of sclerotic myocardial lesions.
In the initial stage, there may be arrhythmia, low blood pressure, heart murmurs and poor conduction . With the development of the disease, when the degree of distribution of scar tissue in relation to healthy tissue increases, symptoms begin to increase.
The patient may be concerned about:
- shortness of breath and feeling of lack of air during physical activity,
- fatigue and systematic weakness,
- increased sweating,
- pain in the heart area,
- various arrhythmias (atrial fibrillation and extrasystole),
- tachycardia or bradycardia,
- low pressure,
- systolic murmur (when listened to by a doctor),
- cough after shortness of breath (most often manifests itself at night),
- swelling of the limbs and abdominal cavity,
- pale skin,
- cold extremities,
- pre-fainting states.
Since many of the symptoms are common in other heart diseases, it is very important to identify this disease early . Only an experienced doctor, after conducting a series of special tests and examinations, can diagnose post-myocardial cardiosclerosis. Therefore, it is important to consult a cardiologist if these symptoms systematically appear.
After severe infectious and viral diseases, electrocardiography is recommended to exclude heart complications.
The main symptoms of cardiosclerosis
Manifestations of post-myocardial cardiosclerosis can be divided into two groups. Namely:
- Heart failure (usually chronic);
- Rhythm disturbances.
In cardiosclerosis with small foci and moderate diffuse damage, an asymptomatic course is possible. This is more often typical for young people who have not previously suffered from other cardiovascular diseases.
Scar formation in the myocardium is a relatively slow process. During it, adaptation mechanisms are gradually activated, allowing the heart to cope with the load. Connective tissue is unable to contract. Therefore, if the heart does not have enough remaining working tissue, compensatory myocardial hypertrophy occurs (an increase in the muscle mass of the ventricles, primarily the left one). At this stage, patients often do not complain.
Heart failure
When the protective mechanism in the form of hypertrophy becomes insufficient, the heart begins to cope with its pumping function worse. This leads to the accumulation of blood in the ventricles and their gradual increase in volume. At the stage of mild and moderate dilatation, there may also be no complaints. With a pronounced loss of working myocardial mass, symptoms of heart failure occur. The main ones:
- Dyspnea. Most often it is inspiratory in nature (difficulty breathing). In severe cases, orthopnea occurs - severe shortness of breath in a horizontal position, which decreases when taking a sitting position.
- Weakness. There is increased fatigue and lethargy.
- Edema. Usually first appear in the lower extremities. Unlike edema in vascular diseases (for example, varicose veins), they are always symmetrical. May be combined with ascites (accumulation of fluid in the abdominal cavity).
- Increase in heart rate. It occurs due to the fact that the heart, which is not capable of normal contraction, tries to “pump out” the required volume by accelerating its work.
- Decrease in blood pressure. Characteristic of severe CHF.
Signs of CHF can vary from mild to severe. The rate of transition to decompensation and the severity of symptoms depend on the area of the affected myocardium and the presence of concomitant diseases.
Rhythm disorders
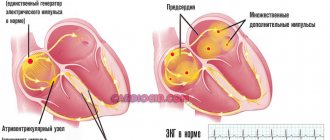
Foci of cardiosclerosis can become a source of arrhythmia. The type of rhythm disturbance depends on the area of heart damage. For example, an arrhythmia of the bigeminy type is possible: the formation of a pathological impulse after each normal beat (ratio 1:1).
The progression of CHF with post-myocardial cardiosclerosis can also cause arrhythmia. The atria, which are stretched due to volume overload, begin to flicker, that is, contract chaotically.
Subjectively, rhythm disturbances can be felt as interruptions in the functioning of the heart, a feeling of fluttering or upheaval of the heart in the chest. With persistent forms of arrhythmia, patients often stop feeling them. Particularly dangerous are episodes of sudden loss of consciousness.
Important nuances
When visiting a doctor for the first time to diagnose a pathology, the patient must mention what diseases he has had before. If the medical history includes myocarditis, the likelihood of developing disorders increases significantly.
Can postmyocardial cardiosclerosis be cured? Unfortunately, nowadays science still does not know ways to reverse the negative process. The exception is the mildest forms of the disease, which the body overcomes with its resources.
The gene therapy currently being developed has a certain positive effect. True, such treatment is expensive and is still at an insufficient level.
Symptoms for different forms of pathology
Myocardiosclerosis can be focal or diffuse. The presence of the first option means the formation of large or small areas of necrosis. If the second form of the disease is detected, it means that replacement with fibrous tissue spreads evenly throughout the myocardium.
With the development of the focal form, signs are noted in the form of:
- lack of air, which is more disturbing when lying down;
- rapid breathing;
- tachycardia;
- puffiness of the legs;
- headaches;
- dizziness.
The diffuse type is more dangerous in its consequences.
The patient suffers from:
- shortness of breath at rest;
- suffocation at night;
- cardiac asthma (in advanced form);
- painful sensations;
- frequent heart rhythm disturbances;
- discomfort in the side on the right side;
- night cough and chills.
By the end of the day, the patient’s well-being worsens, which should be a reason for immediate contact with a specialist.
Diagnostics
When listening to the patient, weakened heart sounds and murmurs . Blood pressure may be normal or reduced.
Additional laboratory and clinical research methods help differentiate myocardiosclerosis from other heart diseases that have similar symptoms:
- chest x-ray
- Ultrasound of the heart reveals thickening of the myocardial walls throughout the heart or in individual areas. The cavities of the heart (usually on the right side) are dilated. In later stages, the valves do not close the communicating cavities when necessary, and the blood flows backwards, which can also be determined using echocardiography.
- An electrocardiogram reveals disturbances in the cardiac impulse at different levels of its occurrence and conduction. Diffuse changes are noted, more often expressed in the right ventricle.
- The method of radionuclide diagnostics can identify areas of non-viable myocardium (scar tissue).
- Biochemical blood parameters usually remain normal. Post-myocardial cardiosclerosis can be distinguished from post-infarction and atherosclerotic by the absence of an increase in lipoproteins and cholesterol in a biochemical blood test.
Complicated form
Healthy cardiac myocardium has good elasticity and contracts well. When it is replaced by fibrous connective tissues, which do not have elasticity and do not take any part in the contractile function of the myocardium, they lead to the fact that with insufficient contraction of the cardiac muscle, a load on the cardiac organ occurs.
If there are foci of cardiosclerosis in the cardiac organ, it is likely to be asymptomatic, but if the localization of cardiosclerosis is located on the cardiac impulse line, or near the sinus node, then the probability of developing arrhythmia is 100.0%.
The development of changes of the sclerotic type provokes the pathology of compensatory hypertrophy, as well as expansion of the myocardial muscles.
When the muscle reserve of hypertrophy is exhausted, the contractile function of the myocardium decreases and cardiac organ failure develops. Scarring processes in the heart valves provoke deformation of the heart valve apparatus and heart valve insufficiency.
The larger the area of the cardiac myocardium is affected by myocardial cardiosclerosis, the higher the likelihood of disruption of the functioning of the cardiac organ, until it stops completely.
The most dangerous and complex complication of post-myocardial cardiosclerosis is progressive heart failure, as well as aneurysm of the cardiac myocardium, disturbances in the rhythm and conduction of impulses of the cardiac organ.
The larger the area of the cardiac myocardium is affected by myocardial cardiosclerosis, the higher the likelihood of disruption of the functioning of the cardiac organ
Treatment tactics
The first symptoms of the disease appear at the stage when the structure of the myocardial tissue has already changed. It is impossible to achieve regression of this process. Therapy for myocardiosclerosis is aimed at slowing down the formation of connective tissue and improving heart function.
The main treatment plan should be identifying and eliminating the factors that caused myocardial inflammation . If the cause is an infectious disease, antibiotic or antiviral therapy is used depending on the type of infectious agent. In case of systemic manifestations, the underlying disease is treated. Allergic causes require mandatory elimination of the allergen.
At the same time, medications are prescribed that normalize cardiac activity. In drug therapy of the most dangerous complication of cardiosclerosis, heart failure, the following drugs are used - diuretics, cardiac glycosides, vasodilators, antioxidants.
To select the correct treatment regimen, patients undergo daily ECG monitoring and are prescribed trial courses of drugs.
Along with drug therapy, limiting physical activity and a special diet are recommended to reduce the load on the heart.
Cardiac arrhythmias are corrected with the help of antiarrhythmic drugs .
In case of severe bradycardia, implantation of a pacemaker is required, a special device that sets the rhythm of the heart using electrical impulses. If a cardiac aneurysm is present, surgery may be necessary.
The most severe variant of the development of postmyocardial cardiosclerosis is an indication for a heart transplant .
Interesting scientific research is being carried out today in the treatment of cardiosclerosis with stem cells, but due to the high cost and ambiguous results, the widespread use of this technique remains in question.
How is the treatment carried out?
Use of medications
The treatment regimen is prescribed by the doctor; self-medication is prohibited. For the treatment of post-myocardial cardiosclerosis, the drugs shown in the table are used:
| Medication group | Name |
| Cardiac glycosides | "Korglikon" |
| "Strophanthin" | |
| "Digoxin" | |
| "Celanid" | |
| Vasodilators | "Apressin" |
| "Molsidomin" | |
| "Glycine" | |
| "Nitroglycerine" | |
| "No-Shpa" | |
| Sodium nitroprusside | |
| Antioxidants | "Vitrum Cardio" |
| "Vitrum Antioxidant" | |
| "Omakor" | |
| "Epadol" | |
| "Cratal" | |
| "Dibikor" | |
| "Asparkam" | |
| Diuretics | "Furosemide" |
| "Diakarb" | |
| "Veroshpiron" | |
| "Hypothiazide" | |
| "Lasix" |
Surgical intervention
Surgery to install a pacemaker is performed to normalize the heart rhythm.
Treatment of the disease is carried out using the following operations:
- Heart transplantation. An organ is being replaced with a donor one.
- Installation of a pacemaker. The device ensures normalization of heart rhythm by releasing impulses that correct the heart rate.
Life forecast
Postmyocardial cardiosclerosis can be treated comprehensively and achieve good results. There is no way to start this pathology; the sooner cardiosclerosis is diagnosed, the sooner its progression can be stopped with minimal damage to the cardiac myocardium.
It is impossible to completely restore the destruction of the myocardium, but it is quite possible to stop the failure and lead a normal lifestyle.
If postmyocardial cardiosclerosis is not treated, it progresses quite quickly and leads to sudden death.
Treatment
Treatment of post-myocardial cardiosclerosis is based on drug therapy, and compliance with nutritional and dietary measures, as well as lifestyle changes. If a diagnosis of post-myocardial cardiosclerosis is made, it is necessary to reduce physical activity on the body for the next six months.
After 6 months, with normal restitution of cardiac function, physical activity is carried out slowly and gradually.
Once the functionality of the heart has been restored, you can begin to exercise, but only if the systolic function of the left ventricle is completely restored.
Smoking and alcohol are strictly prohibited.
Salt restriction is only for those patients who have been diagnosed with heart failure.
The main therapy is aimed at:
- Treatment of left ventricular dysfunction and treatment of left ventricular failure;
- Decrease in blood pressure index;
- Elimination of disturbed heart rhythm;
- Elimination of impaired electrical conductivity of cardiac impulses.
It is also necessary to stop heart failure and restore all metabolic processes in the body.
Drug therapy consists of the following groups of medications:
- ACE inhibitors;
- Beta blockers in acute forms of pathology development, but only during the period of stabilization of the condition;
- Mineralocorticoid receptor antagonists - the drug Spironolactone;
- For swelling, diuretics are prescribed;
- Many patients are prescribed Digoxin, or the drug Ivabradine.
If drug therapy does not have a positive result, then surgical treatment of post-myocardial cardiosclerosis is used.
Drug therapy
Immunosuppressive drug therapy for cardiosclerosis
This therapy is prescribed to patients in whom an inflammatory process in the myocardial infiltration has been confirmed by biopsy, but if viral and infectious agents are not detected in the cardiac myocardium.
Immunosuppressive therapy with Prednisolone and Azathioprine significantly improves left ventricular systole and reduces severe symptoms of left ventricular failure.
Immunosuppressive therapy lasts from 90 days to 180 days.
Causes of the disease
Unlike other cardiovascular diseases, this pathology is often diagnosed in young people under the age of 30 and older and in children. This disease can rightly be called a typical disease of young people. Therefore, questions always arise: post-myocardial cardiosclerosis - what is it, what is the prognosis for life and ability to work, and whether people with such a diagnosis can be drafted into the army.
Its etiology and pathogenesis differ from the causes and development of atherosclerosis in coronary artery disease. According to ICD 10, the disease has a code of 120.0 -120.9. When a diagnosis is established, the code of which is within these limits according to the ICD, a military ID is issued, but the possibility of service is considered individually in each case, taking into account the severity of heart damage.
The causes that lead to myocarditis can be very different:
- Infectious diseases caused by viral pathogens (ARVI, herpes, chickenpox, hepatitis), bacteria (angina, diphtheria, scarlet fever), fungi, helminths, protozoa, account for 60 - 70% of all cases.
- Allergic processes that occur after taking certain medications or vaccinations.
- Toxic effects of alcohol or other harmful substances.
- Systemic diseases in which connective tissue and blood vessels are damaged (systemic lupus erythematosus, scleroderma, hemorrhagic vasculitis, rheumatism, periarteritis nodosa) - the myocardium is affected in 35 - 45%.
- Unidentified reasons when, with developed myocarditis (idiopathic) and, subsequently, post-myocardial cardiosclerosis, it was not possible to establish a risk factor.
According to WHO, the development of post-myocardial cardiosclerosis develops in approximately half of patients who have had myocarditis.
Pathogenesis of myocardiosclerosis
As has been established, myocardiocytes are destroyed under the influence of some pathological factor, and in their place connective tissue is formed - areas of sclerosis. According to the number and prevalence of sclerotic lesions, the disease can be:
- focal - when small areas of sclerosis appear in the myocardium;
- diffuse - the process evenly involves the myocardium of all parts of the heart.
In this case, there is no change in the structure of the walls of the coronary vessels: it is not the coronary arteries that are affected, but the capillaries of the heart muscle itself. Therefore, when examined, there may be no changes in the form of cholesterol plaques in the coronary arteries, and according to the International Classification of Diseases, this pathology is classified according to this criterion as other diseases that do not have an atherosclerotic origin.
Classification
Postmyocardial cardiosclerosis can occur in two forms - focal and diffuse.
The focal (scar) form is most characteristic of this disease. With it, the heart muscle is partially affected. Individual foci of changes can have a variety of shapes and localizations.
In the diffuse, most severe form, sclerotic changes in the tissues of the heart are evenly distributed.
Diagnosis of the disease
Myocardial cardiosclerosis is very difficult to identify. Considering that it is a secondary disease, its symptoms may be mistaken for symptoms of a primary disease, prescribing treatment for another disease. Rhythm disturbances may be noticeable on the ECG, but they are not a reason to make such a serious diagnosis. With the disease, bradycardia and tachycardia are observed equally, which also greatly complicates the diagnostic process. The most effective ways to detect the disease:
- MRI;
- dynamic electrocardiogram;
- examination of coronary vessels with or without contrast.
To confirm the diagnosis, a biopsy is performed, i.e. fibrous tissue is taken for examination. Studying tissue in the laboratory gives doctors the opportunity to more accurately determine the form of cardiosclerosis.
Complications
Myocardial hypertrophy - an increase in the size of the heart - is a rather rare complication. The heart increases in size because it must perform its functions regardless of the amount of connective tissue. If the pathology is advanced due to the lack of adequate treatment, the outcome of the disease will be fatal.
Aneurysm. Cells grow on the left ventricle, causing its walls to bulge. Such a complication occurs in almost every case, regardless of the degree of damage. In addition, postmyocardial cardiosclerosis can lead to the development of angina or heart failure.
What to expect?
The most common question from people who have been diagnosed with post-myocardial cardiosclerosis is: “Do they take you into the army?” It all depends on the form of the disease and the degree of its development. A mild form will not be an obstacle to service, while complex cases become the reason for the assignment of disability. Of course, in this case it is impossible to serve in the army.
Disability is prescribed if, as a result of pathology, a person becomes unfit for work. Practice shows that cases of death due to pathology are quite frequent. Many of them are associated with the development of complications: stroke, heart attack.
Diagnosis of the disease
Making an accurate diagnosis usually causes difficulties, since the listed symptoms are accompanied by many pathologies of the cardiovascular system.
The patient is prescribed blood biochemistry and undergoes a number of instrumental studies:
- electrocardiography;
- echocardiography;
- chest x-ray;
- coronary angiography;
- Holter monitoring.
The data obtained will allow you to correctly draw up a treatment regimen using effective drugs.