Photo: https://pixabay.com/illustrations/heart-curve-health-pulse-frequency-66888/ Sclerosis (from the Greek skleros - hard) is a pathological process that is the outcome of any inflammation or damage to tissues or organs. This is a kind of compaction of the tissue structure, which occurs due to the proliferation of connective tissue at the site of damage. The tissue replaces healthy cells of a particular organ, reducing or significantly impairing its function.
Cardiosclerosis (myocardiosclerosis) is the process of replacement by connective tissue of cardiomyocytes - cardiac muscle cells, muscle fibers due to the proliferation of connective tissue, leading to a decrease in the function of the heart muscle and deformation of the valve apparatus. The name aortocardiosclerosis is also widely used - a term that is not used in clinical practice due to its obsolescence and the revision of the international classification of diseases.
What factors lead to the development of cardiosclerosis?
The causes of the disease can be both heart disease and non-cardiac pathology. Of these, the most common are:
- coronary heart disease, myocardial infarction;
- long-term arterial hypertension;
- hypertrophy of the heart chambers, most often the left ventricle;
- endocrine pathology: diabetes mellitus, thyroid diseases, etc.;
- alcohol abuse, malnutrition, low-protein diets.
When can cardiosclerosis become dangerous?
The development of cardiosclerosis up to 40.0% - 45.0% does not cause any pronounced signs and symptoms that would express the development of cardiosclerosis. Such minor scarring does not pose a strong danger to humans, but on the condition that it is necessary to constantly treat pathologies of the heart organ and blood flow system.
It is especially necessary to treat hypercholesterolemia and arterial hypertension, which causes damage to the coronary arteries, which provoke ischemia of the cardiac organ.
Danger to human life arises under these circumstances:
- With the progression of cardiosclerosis and the spread of a diffuse type of pathology over a large area of the myocardium, leading to thinning of the walls of the heart;
- When the ability of the heart to contract as much as possible decreases, which leads to cardiac organ failure;
- With hypertrophy of the walls of the heart chambers and interchamber septa, which causes an increase in the size and volume of the heart;
- Weak scarring can cause the development of an aneurysm, which, with strong protrusion, can have the properties of rupture, which leads to death;
- A very thick scar, affecting the main lines of the cardiac impulse, can lead to blockade of the cardiac impulse, arrhythmia, or to the development of such pathologies of the heart rhythm - extrasystole, ventricular fibrillation.
Atherosclerosis
Classification of cardiosclerosis
main forms are distinguished .
- Postmyocardial cardiosclerosis. Myocarditis is an inflammation of the heart muscle (myocardium), the sources of which can be chronic foci of infection in the body, viral and fungal infections suffered in childhood and young age, toxic lesions of the myocardium (drugs, radiation, chemicals) or rheumatic diseases (systemic red lupus, giant cell arteritis, etc.). It most often affects children, as they are most susceptible to infections, or young people.
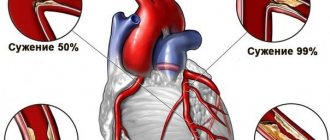
- Atherosclerotic cardiosclerosis. A pathology more common in older patients. With long-term coronary heart disease, when the myocardium is insufficiently supplied with blood due to arteries narrowed from atherosclerosis, the heart's reserves of nutrients and oxygen are depleted, dystrophy of muscle fibers develops, and their gradual death is replaced by connective tissue. The process of atherosclerotic cardiosclerosis has an extensive, so-called diffuse nature.
- Post-infarction cardiosclerosis. Develops at the site of a dead section of the heart muscle after the development of myocardial infarction. Due to blockage of the coronary artery, blood stops flowing to the area of the myocardium that it supplies. First, ischemia of cardiomyocytes develops, then their necrosis. After 7-10 days, the area of necrosis begins to degenerate, leukocytes destroy dead cells, and in their place they begin to synthesize coarse connective tissue fibers. After 4 weeks from the onset of myocardial infarction, a full-fledged connective tissue scar, or post-infarction cardiosclerosis, forms.
Based on the extent of damage, they are classified as:
- focal cardiosclerosis;
- diffuse cardiosclerosis.
Diagnosis of cardiosclerosis
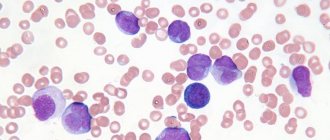
The presence of collagen tissue at the site of the myocardium does not have any effect on the blood, so laboratory diagnosis is not informative. It can only help to determine the cause of cardiosclerosis.
Currently, the following instrumental techniques are used to determine changes in the heart wall:
- ECG - this method is not reliable in diagnosing cardiosclerosis. Electrocardiography can only detect an area of the heart that has been damaged or has insufficient blood supply. Based on these changes, the doctor may assume the presence of a pathological focus and prescribe additional examination;
- Echocardiography (synonymous with ultrasound of the heart) is the most informative way to detect changes in the myocardium. EchoCG can directly see the growth of connective tissue in the wall of the heart and accurately determine the size and location of the defect. Most often, surface echocardiography is used - an ultrasound sensor is placed directly on the skin of the anterior chest wall, after which the doctor receives an image of the heart in various planes on the monitor;
- Scintigraphy - this method is rarely used in Russia due to its high cost. It is carried out as follows: the patient is injected with radioactive isotopes of a certain chemical element (usually thallium) and its distribution throughout the heart is assessed. The presence of “cold spots” (places where there is no isotope) indicates difficulty in blood flow in this part of the myocardium and possible cardiosclerosis. It is necessary to clarify that scintigraphy is a completely safe method, but is not included in the mandatory diagnostic standard.
Using the above examination methods, you can detect cardiosclerosis and begin treating such a patient.
Changes occurring in the organ
Focal cardiosclerosis occurs in isolation as a result of myocardial infarction. The part of the myocardium that was previously damaged undergoes changes. Depending on the nature of the lesion, focal cardiosclerosis can be large-focal - often after an extensive transmural infarction, when the entire affected area is replaced by connective tissue and a clear focus of sclerosis is formed, or small-focal - when damage in the myocardium has not developed in every first cell, but chaotically, in different muscle cells. fibers due to long-term ischemia and hypoxia of these areas.
Healthy heart cells seem to fall into the zone of non-functioning cardiomyocytes, and then even with all the contraction potential, they do not fully perform their function, being in a kind of trap.
Photo: https://pixabay.com/illustrations/heart-attack-stroke-heart-disease-3177360/
Diffuse cardiosclerosis or myocardiofibrosis occurs with long-term uniform lesions of the heart. This most often occurs with left ventricular hypertrophy, long-term coronary heart disease, heart damage due to diabetes, thyroid diseases, toxic myocardial damage, etc.
Due to a constant lack of oxygen and nutrients, high sugar levels or impaired blood flow, degeneration and atrophy of cardiomyocytes develops throughout the heart muscle, which reduces the overall contractility of the heart and its basic pumping function.
How effective is the treatment?
Treatment of cardiosclerosis is carried out only after the diagnosis has been established. To get rid of the signs of the disease, it is necessary to turn the connective tissue back into muscle, but unfortunately, this is impossible. The only way out in this situation is to support the functioning of the myocardium by all available methods in order to stop the further spread of areas of sclerosis.
The following treatment methods are available to the doctor:
- diet;
- lifestyle modification;
- pharmacological drugs;
- surgical intervention.
Main clinical manifestations of cardiosclerosis
Myocardiosclerosis has no specific symptoms. This is a syndrome that completes the course of any cardiac pathology. Regardless of its origin, cardiosclerosis acquires symptoms of heart failure.
Dyspnea
Shortness of breath may be the earliest symptom of heart failure. At first, patients feel a lack of air during high physical activity, then, as the disease progresses and the pumping function of the heart decreases, shortness of breath gradually occurs with less intense exercise, and in severe cases, even at rest.
Arrhythmia
Various types of arrhythmias: supraventricular and ventricular extrasystoles, paroxysmal tachycardia, atrial fibrillation, blockade, etc. Cardiomyocytes, which are responsible for conducting impulses along muscle fibers, are also replaced by connective tissue, which is not capable of conducting electrical impulses.
Edema of the lower extremities
If the pumping function is impaired, the heart stops pumping blood around the body quickly and efficiently, the speed of blood flow slows down, and it becomes more difficult for the heart to pump blood out of the lower extremities, where it stagnates. Due to the increased pressure, plasma (the liquid part of the blood) sweats through the wall of the vessel into the subcutaneous fatty tissue of the lower legs.
If left untreated, blood stagnation increases, swelling spreads to the thigh, and in particularly severe cases, an accumulation of fluid in the abdominal cavity, called ascites, forms.
Cough
Cough is a symptom of blood stagnation in the pulmonary circulation, that is, in the lungs. The liquid sweats into the alveoli, interferes with proper ventilation of the lungs, and a reflex cough occurs to remove excess fluid. This cough occurs after physical activity and gets worse when lying down. Often, patients with symptoms of stagnation in the pulmonary circulation place additional pillows during sleep or are forced to sleep with the head end of the bed elevated
Muscle weakness
Muscle weakness and rapid fatigue during physical activity. This symptom is caused by impaired blood supply to skeletal muscles due to a decrease in the pumping function of the heart and an increase in symptoms of heart failure.
Pain syndrome
Pain in the heart, palpitations, interruptions in heart function. These symptoms are caused by decreased myocardial function.
Pain in the right hypochondrium and enlarged liver occur due to stagnation of blood in the systemic circulation, an increase in the liver parenchyma and its pressure on the capsule, which abundantly contains nerve endings.
Possible manifestations
Specific symptoms of cardiac cardiosclerosis are most often absent. This is the main feature of this pathology. The disease may not reveal itself in any way. In many patients, a latent course is observed, and the first signs appear when the heart muscle is subject to pronounced structural changes.
To determine the likelihood of developing cardiosclerosis, doctors must take into account the presence of heart and vascular diseases or past pathologies.
Typically, the manifestations of cardiosclerosis coincide with the signs of the underlying pathology that caused the scarring:
- If the appearance of connective tissue is associated with a disruption in the flow of blood to the muscles of the heart, then the person suffers from severe pain in the heart area, which intensifies with physical and emotional stress.
- If large-focal cardiosclerosis or a diffuse process occurs, the organ increases in size.
- If the heart begins to beat at a rate of more than ninety beats, even with little physical activity, then tachycardia is diagnosed. This is a nonspecific but common disorder that accompanies sclerotic processes.
- When sclerotic processes spread to the conduction pathways, the movement of the electrical impulse is disrupted and the heart contracts irregularly, a person experiences interruptions in its work. At the same time, you often feel dizzy, your blood pressure drops, and you experience fainting. Arrhythmias and blockades are frequent companions of cardiosclerosis.
- If muscle tissue is covered with a large number of scars, then it loses its contractile abilities. In this case, the patient is accompanied by weakness, shortness of breath, legs swell, and the liver increases in size. Insufficiency of organ functions develops.
Also read: Features and mechanisms of development of vasospastic angina
Diagnostics
Diagnostics is a multicomponent process and includes the following stages.
Collection of complaints
It is important to ask the patient in detail about the moment of occurrence of a particular symptom, the conditions of its occurrence and the method of relief. Particular attention is paid to questions about past diseases - heart attack, stroke, angina pectoris, myocarditis or rheumatism. Cardiosclerosis can form as a result of any of these pathologies.
Photo: https://pixabay.com/photos/benchmarking-doctor-pressure-830898/
Inspection
Many patients with initial manifestations of the disease do not differ in appearance from healthy patients. But more often, when examining the skin, one notices cyanosis, or blue discoloration of the skin. The lips, fingertips, nose or earlobes may turn blue - so-called acrocyanosis. In the terminal stages, massive staining of the skin in a bluish color is possible.
Often patients do not pay attention to the swelling they experience or do not evaluate its prevalence. Edema in heart failure is characterized by its occurrence at the end of the day, mainly on the legs, and disappears after rest or sleep.
There are also so-called “hidden” edema - when fluid is retained in the body, but it is not enough to manifest itself as swelling of the legs. Patients may notice a weight gain of 2 kg in 5 days or 3 kg in 7 days, which will indicate the hidden development of edema.
The blood pressure of patients with heart failure can be either normal or elevated with concomitant arterial hypertension. At the end of the development of the disease, when the heart can no longer cope with the load, the pressure becomes reduced. Heart rate is also variable.
Instrumental diagnostic methods
The main research method to accurately diagnose cardiosclerosis is echocardiography or ultrasound examination of the heart. When it is carried out, the zones of the myocardium that contract poorly (hypokinesia zones) or do not contract at all (akinesia zones) are most accurately visualized. The general contractility of the heart, the size of the cavities, the amount and speed of blood ejected in one cardiac cycle are also visible.
The doctor will subsequently rely on these data when choosing treatment tactics, monitoring its effectiveness and duration.
- An ECG is performed on all patients to assess heart function, diagnose rhythm and conduction disorders, and help assess the prognosis of the disease.
- Detailed clinical blood test.
- A detailed biochemical blood test with the study of electrolytes (sodium, calcium, potassium), liver enzymes, and assessment of glomerular filtration rate.
- Blood test for glucose.
- Study of thyroid function.
- X-ray of the chest organs.
- MRI of the heart.
Many of these methods are aimed at finding the true cause of the disease and prescribing the most appropriate therapy for each patient. It is worth noting that the use of one or another diagnostic method remains at the discretion of the doctor.
Causes
The transition of cardiomyocytes into connective tissue occurs due to the inflammatory process. In this case, the formation of connective tissue fibers is a kind of protective mechanism.
Depending on the reasons, several groups are distinguished:
- atherosclerotic form;
- post-infarction cardiosclerosis;
- myocardial form;
- other reasons.
Atherosclerotic cardiosclerosis
Includes diseases that lead to cardiosclerosis through long-term ischemia and ischemic heart disease. Atherosclerotic cardiosclerosis is not classified in a separate category according to ICD-10.
Coronary heart disease develops as a result of atherosclerosis of the coronary arteries. When the lumen of the vessel narrows, the myocardium ceases to receive normal blood supply. The narrowing occurs due to the deposition of cholesterol and the formation of an atherosclerotic plaque, or due to the presence of a muscular bridge over the coronary vessel.
With prolonged ischemia , connective tissue begins to grow between cardiomyocytes and cardiosclerosis forms. It is important to understand that this is a rather long process and most often the disease is asymptomatic. The first signs begin to appear only when a significant part of the heart muscle is filled with connective tissue. The cause of death is the rapid progression of the disease and the development of complications.
Myocardial form (Postmyocardial cardiosclerosis)
The mechanism of development of myocardial cardiosclerosis is completely different. A lesion forms at the site of former inflammation after myocarditis. This type of cardiosclerosis is characterized by:
- young age;
- history of allergic and infectious diseases;
- the presence of foci of chronic infection.
ICD-10 code for postmyocardial cardiosclerosis: I51.4.
The disease develops due to proliferative and exudative processes in the myocardial stroma, due to destructive changes in the myocytes themselves. With myocarditis, a huge amount of substances are released that have a damaging effect on the membranes of muscle cells. Some of them are destroyed. After recovery, the body, as a protective reaction, increases the production and volume of connective tissue. Myocardial cardiosclerosis develops much faster than atherosclerosis. The myocardial variant is characterized by damage to young people.
Post-infarction cardiosclerosis
Formed at the site of death of cardiomycytes after acute myocardial infarction. When blood access through the coronary artery to the heart muscle is stopped, necrosis of the corresponding area develops. The area may be of different locations depending on which vessel is blocked. Depending on the caliber of the vessel, the size of the affected area also changes. As a compensatory reaction, the body begins increased production of connective tissue at the site of the lesion. The code for post-infarction cardiosclerosis according to ICD-10 is I25.2.
The prognosis for survival after a heart attack depends on many factors. The cause of death after a heart attack lies in complications of the disease and lack of adequate therapy. Post-infarction syndrome is an autoimmune reaction that complicates myocardial infarction and is manifested by symptoms of inflammation of the pericardium, lungs and pleura.
Postpericardiotomy syndrome is an inflammatory autoimmune disease of the pericardium that develops after open heart surgery.
Other reasons
In addition to those described above, there are other reasons that are more rare.
- Radiation exposure. Under the influence of radiation exposure, changes occur in a variety of organs and tissues. After irradiation of the heart muscle, irreversible changes and complete restructuring occur in cardiomyocytes at the molecular level. Gradually, connective tissue begins to form, its proliferation and the formation of cardiosclerosis. The pathology can develop lightning fast (within several months after strong radiation) or slowly (several years after exposure to a low dose of radiation).
- Sarcoidosis of the heart. A systemic disease that can affect a wide variety of organs and tissues. In the cardiac form, inflammatory granulomas form in the myocardium. With proper therapy, these formations disappear, but in their place, pockets of scar tissue can form. Thus, focal cardiosclerosis is formed.
- Hemochromatosis. This disease is characterized by the deposition of iron in the tissues of the heart. Gradually, the toxic effect increases, an inflammatory process develops, which ends with the proliferation of connective tissues. With hemochromatosis, cardiosclerosis affects the entire thickness of the myocardium. In more severe cases, the endocardium is also damaged.
- Idiopathic cardiosclerosis. This concept includes cardiosclerosis, which has developed for no apparent reason. It is assumed that it is based on as yet unknown mechanisms. The likelihood of the influence of hereditary factors that provoke increased growth of connective tissue at a certain stage of the patient’s life is considered.
- Scleroderma. Damage to the heart muscle in scleroderma is one of the most dangerous complications of the disease. Connective tissue begins to grow from the capillaries that the heart muscle is so rich in. Gradually, the size of the heart increases against the background of constant thickening of the walls. Traditional signs of destruction of cardiomyocytes and the presence of an inflammatory process are not recorded.
There are many mechanisms and reasons for triggering the proliferation of connective tissue in the myocardium. It is quite difficult to reliably establish the true cause of the disease. However, identifying the root cause of the pathology is simply necessary to prescribe the correct treatment.
Complex treatment of cardiosclerosis
You need to understand that cardiosclerosis is not a fatal disease or a depressing illness, it is a way of life, coexistence with such a feature of the heart. You can live an absolutely fulfilling life by following a diet, physical activity and taking medications. You can enjoy life by taking control of the disease.
Photo: https://pixabay.com/photos/doctor-doctor-s-office-stethoscope-3464761/
Therefore, an integrated approach in the treatment of cardiosclerosis is important, teamwork between the doctor and the patient working towards a single result - human health.
So how do you need to change your lifestyle?
Control body weight
The first stage of lifestyle changes is to monitor the efficiency of the heart and the effect of drug therapy by controlling hidden edema. If your body weight has increased by 2 kg in 5 days or by 3 kg in 7 days, you should contact a cardiologist or adjust the therapy yourself according to the algorithms given by the doctor.
Follow a diet
Excess body weight or obesity worsens the prognosis and course of the disease, therefore, with a body mass index of more than 25 cm/kg2, you should adhere to a diet that limits caloric intake depending on age and somatic norms. At the same time, the diet should contain a sufficient amount of protein - mainly fish, lean poultry, legumes, contain a lot of polyunsaturated fatty acids, vegetables and fruits (up to 500 g per day).
It is necessary to exclude or minimize the intake of processed meat, simple carbohydrates, salty, fatty, fried foods, and canned food from the diet. The amount of table salt supplied with food should not exceed 6 g/day, which corresponds to moderate salting of food during cooking or “do not add salt to food,” since a large amount of essential sodium and chlorine enters the body with foods that do not contain salt.
Liquids should be limited only if the patient’s condition is severe with severe edema; in other cases, it is recommended to drink about 1.5 l/day.
Do physical exercise
You can and should do physical exercise! Even if the patient’s condition is serious, it is necessary to practice breathing exercises even while sitting in bed, starting from a few minutes a day, increasing the pace, since it has been proven that increasing the body’s fitness improves the patient’s prognosis and his quality of life.
Starting with breathing exercises with a gradual increase in intensity and improvement, over time the patient can move on to aerobic exercises such as walking, then running, cycling, swimming and water exercises, Nordic walking. The level of tolerable and suitable load is taken into account taking into account the six-minute walk test (how many meters the patient can walk in 6 minutes). The motor regimen should be prescribed and discussed with the patient by the attending physician.
Follow recommendations for a healthy lifestyle
Smoking is contraindicated for all categories of patients. Alcohol should also be excluded, but the recommendations of the Russian Cardiological Society are a little softer - no more than 250 ml of beer or 125 ml of wine per day. It is also recommended that patients be vaccinated against influenza and pneumococcal infections annually according to the vaccination plan.
Photo: https://pixabay.com/photos/a-change-in-lifestyle-banana-diet-1430599/
Psychological support for patients
It has been scientifically proven that prevention of depression, work with a psychoanalyst in groups and schools of heart failure improves the prognosis of patients and has a positive effect on the dynamics of the disease.
Treatment
First of all, it is necessary to clarify that it is impossible to cure cardiosclerosis. The changes that have occurred in the affected area of the myocardium are irreversible, therefore therapy for such patients is aimed at maintaining the functioning of the remaining heart muscle, eliminating congestion in large vessels and preventing heart attack. Currently, the following treatment regimen is used:
- Acetylsalicylic acid - this substance prevents the formation of blood clots in all arteries of the body. It is an essential component of therapy, as it significantly reduces the risk of heart attack and “blockage”/thromboembolism of the pulmonary artery (PE). It is recommended to use combination acid + magnesium preparations, which will reduce the likelihood of side effects in the form of ulcers. For example: Aspirin Cardio, Cardiomagnyl;
- Angiotensin-converting enzyme (ACE) inhibitors are necessary to slow the development of heart failure, therefore they are prescribed to most patients with cardiosclerosis. They also tend to reduce blood pressure, so if the patient is prone to hypotension (low blood pressure), the dosage is selected individually. Recommended drugs: Enalapril, Captopril, Lisinopril;
Typical side effect. When taking ACE inhibitors, a dry, obsessive cough may begin that persists throughout the day. As a rule, it disappears after several days of using the medicine. However, in rare cases, the cough remains for a long time. The presence of this side effect is a reason to replace inhibitors with an alternative drug.
- Beta blockers - reduce the load on the heart, reducing the force of its contractions. In case of cardiosclerosis, it is prescribed with caution, since cardiac output in such patients is already somewhat reduced. Contraindicated at low contraction frequencies (less than 60 beats/min). Not recommended if you are prone to hypotension. Commonly used beta blockers: Bisopralol, Atenolol;
- Diuretics - these drugs also reduce the load on the myocardium, increasing the removal of fluid from the body. There are different groups of diuretics. The appropriate medicine is chosen depending on the severity of edema, shortness of breath and the presence of hypertension. It is possible to use thiazide drugs (Hypothiazide), aldosterone receptor antagonists (Veroshpiron). Loop diuretics (Furosemide) are used somewhat less frequently;
- Cardiac glycosides - prescribed to maintain heart function. They are used with caution, since along with an increase in cardiac output, the myocardial need for blood supply also increases. But it is often difficult. The only recommended medicine in this group is Digoxin;
- Antiarrhythmic drugs (according to indications) - if the patient has rhythm disturbances, the following medications can be recommended: Amiodarone, Cordarone;
- Statins (according to indications) - cardiosclerosis is often accompanied by elevated levels of cholesterol (above 5 mmol/l) and LDL (above 3 mol/l). In this case, patients are prescribed Atorvastatin, Rosuvastatin, etc.
The use of this scheme, in most cases, makes it possible to achieve an improvement in the patient’s condition. However, if there is no effect of therapy, surgical treatment is recommended, which is aimed at improving the blood supply to the heart. For this purpose, the following is carried out:
- Transluminal balloon angioplasty (abbreviated as TLBAP) - the operation consists of introducing a special device into the coronary vessel, which restores the patency of blood through it;
- Coronary artery bypass grafting - this method has become widespread and is still considered the “gold standard” for difficult blood flow through the coronary arteries. The principle of the operation is as follows: a narrowed/obstructed area is identified and a bypass path for blood is created. For this purpose, a less significant vessel is taken from the patient (most often the saphenous vein of the leg) and the aorta and the patent part of the coronary artery are connected to it.
As a rule, surgical treatment of cardiosclerosis can significantly improve the quality of life of patients. After it, doctors give recommendations that must be followed to prevent relapses.
Diet for cardiosclerosis
The nutrition of patients should be aimed at reducing body weight and normalizing the level of fats in the blood (cholesterol, LDL, triglycerides). It implies an exception:
- Any fried foods;
- Salty, flour, smoked products;
- Animal fat (including butter and fatty meats: pork, veal, beef).
Preference should be given to steamed dishes. You should include plant foods (vegetables, fruits, juices, etc.) and lean meat (chicken) in your diet. Food should not be added salt.
Drug treatment of cardiosclerosis
- Treatment of the underlying disease - cardiac or other therapeutic pathology.
- The main groups of drugs that have been proven to reduce mortality and improve prognosis.
Angiotensin-converting enzyme inhibitors (ACEIs). The drugs reduce blood pressure in arterial hypertension and improve the contractile function of the heart due to the fact that they slow down the degeneration of muscle fibers into connective tissue - the so-called cardioprotective effect. In case of contraindications or intolerance to ACE inhibitors, the doctor may prescribe angiotensin II receptor blockers that have the same mechanism of action.
Beta blockers. Beta blockers block beta adrenergic receptors in the heart, exerting various effects on it - reducing heart rate, force of heart contractions, intensity of heart contractions, reducing dystrophy and necrosis of cardiomyocytes, reducing hypertrophy of the heart chambers, the degree of ischemia and the incidence of life-threatening arrhythmias. The cardioprotective effect is comparable to ACEI.
Mineralcorticoid receptor antagonists (MCRA). This group of drugs reduces fluid retention in the body, providing a diuretic effect, preserving all necessary electrolytes. AMCRs have a pronounced cardioprotective effect, reducing the degree of myocardial fibrosis.
Diuretics. They are used for edema and are prescribed in small doses at an early stage of the disease.
Anticoagulants and antiplatelet agents. Drugs that reduce blood clotting are necessary in a number of cases when the pumping function of the heart deteriorates so much that the blood flow slows down, the blood stagnates and blood clots can form in the bloodstream, which are dangerous for the development of thromboembolic complications.
Antiarrhythmics and cardiac glycosides. Indicated for concomitant arrhythmias to reduce their incidence.
What is cardiosclerosis
In general, sclerosis is the death of functional cells of an organ and their replacement by non-functional connective tissue.
Sclerosis is not an independent disease, but a consequence of other negative processes occurring in the body. This is how the protective reaction of the immune system manifests itself, compensation occurs, replenishment of lost cells. If for some reason the cells of the heart muscle (cardiomyocytes) are damaged, then dense scars of connective tissue form at the site of the defects. Their fibers are completely unable to perform the necessary functions.
The damaged area of the heart muscle is restored not by new muscle cells, but by connective tissue cells (scar),
which do not perform functions characteristic of heart muscle cells .
In the initial stages of the disease, healthy myocytes perform double work: their own and the damaged cells. But gradually their nutrition is disrupted, they also die, and scarring occurs again. As the affected areas grow, the heart muscle begins to lose efficiency, its contractile function decreases, and the rhythm of the heartbeat is disrupted.
Unfortunately, there is a lot behind the statement that the heart muscle is losing its functionality. First of all, the loss of part of the muscle’s ability to contract (scar tissue cannot contract) leads to a redistribution of efforts to push blood to other parts of the muscle. This leads to a general increase in the load on the heart and a shortening of the full life of the heart and its carrier.
Damaged muscle areas are not able to correctly distribute contraction control impulses coming from the brain. As a result, heart rhythm disturbances occur.
The same damaged areas begin to distort the paths of nervous excitation, blocking the paths of impulses from the atria to the ventricles with blockades of various types.
The disease may be:
- focal, with the formation of whitish scars between normal cells;
- diffuse, when the connective tissue is a lattice in the cells of which healthy cardiomyocytes are located.
Surgery
- Placement of an implantable pacemaker (ICS) - used when the conduction of impulses along the heart fibers is disrupted or the heart rate decreases.
- Coronary artery or mammary coronary artery bypass grafting.
- Surgeries on heart valves for heart failure caused by valvular defects.
- Heart transplantation.
Photo: https://pixabay.com/photos/hospital-operating-room-doctor-2767950/
Causes of cardiosclerosis
Every disease has its own origins. The main causes of cardiosclerosis lie in the diseases that gave rise to the development of the disease, as well as in the lifestyle of patients. From the point of view of the Great Medical Encyclopedia, there are only three main causes of cardiosclerosis. This:
- Narrowing of the large vessels of the heart, resulting in insufficient blood supply to the myocardium and hypoxia developing;
- Inflammatory processes affecting the heart muscle;
- An increase in the volume of the heart muscle, stretching of its walls (for example, due to dilated cardiomyopathy).
The occurrence of this condition is also influenced by lifestyle characteristics and genetic predisposition (for example, to atherosclerosis).
The most common cause of cardiosclerosis is atherosclerosis of the heart vessels, often associated with a previous heart attack, to which the heart tissue responded by sclerosis
The development of cardiac pathology is most strongly influenced by:
- Sedentary lifestyle and lack of physical activity and sports;
- Smoking;
- Eating fatty and spicy foods in large quantities;
- Systematic overeating and, as a result, excess body weight;
- Alcohol abuse;
- Regular excessive physical activity for a long time;
- Constant stress;
- Heredity.
Due to such factors, the number of cases of cardiovascular diseases in the world increases every year. And with them the risk of developing cardiosclerosis increases.
Prevention of cardiosclerosis
The first stage of prevention is constant monitoring by a cardiologist or therapist, treatment of the underlying cardiac pathology.
It is also important to undergo an annual examination: do an ECG, ultrasound of the heart, take blood tests for cholesterol and sugar.
It is worth observing the work and rest schedule, not performing heavy physical activity, engaging in physical education, and monitoring blood pressure levels.
Follow the Mediterranean diet rules in your diet, consume healthy and tasty food, drink at least 1.5 liters of water per day.
Factors that provoke cardiosclerosis
Factors provoking cardiac sclerosis:
- Arterial hypertension with a very high blood pressure index. With a high blood pressure index, blood accelerates in the bloodstream, which causes the heart to beat faster. Increased cardiac contraction depletes the myocardium, and also causes the appearance of atherosclerotic plaques and blood clots on the coronary arteries and heart vessels, causing hypoxia of the organ and the development of cardiosclerosis;
- Disorders of metabolic processes in the body and the most detrimental effect for the heart organ are disturbances in lipid metabolism, which causes the development of hypercholesterolemia, and a high cholesterol index becomes a factor in the development of systemic atherosclerosis, which quite often affects the coronary arteries, leading to myocardial hypoxia and the development of sclerosis;
- Adverse negative habits lead to a narrowing of the arteries of the blood flow system and the heart feels a lack of oxygen. Nicotine addiction is especially dangerous for cardiac hypoxia;
- Excess body weight is also one of the main reasons for the formation of cardiosclerosis. With obesity, the heart organ must pump a larger volume of blood, which doubles the load on the myocardium. With such a load, the heart quickly wears out, which can cause death even at a young age;
- Constant interruption in stressful situations. During nervous overstrain, significant production of hormones occurs by the endocrine system, namely the adrenal glands. For this reason, the vessels lose their elasticity, and metabolic processes are disrupted. This causes oxygen deficiency, the development of hypoxia of the cardiac organ and the formation of cardiosclerosis on its basis;
- When exposed to radiation, cardiomyocytes die and are replaced by fibrous tissue;
- Physical inactivity;
- Poor diet with large amounts of cholesterol-containing foods. There are also disturbances in lipid metabolism from eating fried, pickled, smoked foods, which causes deviations in the functioning of the blood flow system, which leads to hypoxia of the cardiac myocardium and scar formation;
- Overloading the body with heavy physical labor also depletes the myocardium and provokes the death of cardiomyocytes and their replacement with fibrous tissue.
Factors provocateurs of cardiac sclerosis