Prerequisites that may indicate a stroke
Disorders such as stroke do not occur suddenly.
As a rule, before an attack there are signs that the blood supply to the brain is impaired. These signs include:
- frequent headaches;
- memory impairment;
- tinnitus;
- numbness of the limbs and facial muscles;
- disorder in coordination of movements.
A predisposition to such disorders is observed in hypertensive patients, long-term smokers, people suffering from diabetes mellitus, heart and vascular diseases, obesity, as well as in those whose blood cholesterol levels exceed the norm.
If you experience one or more of the symptoms that precede a stroke, you should seek medical help immediately.
What to do if you have a headache?
You must report the problem to your doctor. Under no circumstances should you self-medicate!
It is necessary to conduct an examination and identify the cause of the pain, only then can treatment begin. In some cases, proper nutrition and more rest are enough, but in other situations, drug therapy cannot be avoided.
Stroke victims do not always experience a headache, but a neuropathic, apparent headache after a stroke can haunt the patient for a long time. The main thing is not to get depressed and rely on doctors and loved ones.
The alarming statistics on the frequency of strokes in young people requires close attention to their condition and the health of their loved ones, since a stroke may be preceded by seemingly harmless symptoms.
Although the term “stroke” itself means “sudden attack,” this condition is not that sudden. It’s just that many people don’t pay attention to the increased frequency of headaches, numbness of the limbs or tingling. People suffering from high blood pressure should be especially vigilant. After all, this group has a much higher risk of stroke, which often happens against the background of a hypertensive crisis.
It must be understood that a stroke can also affect those who do not have problems with high blood pressure, since its cause is not always hypertension, heart rhythm disturbances or myocardial infarction. These can be pathological changes in the blood vessels of the head or neck, as well as the spine. Low blood pressure, which drops catastrophically during sleep, can also cause a stroke.
Headache during a stroke is one of the general cerebral symptoms that should alert you first. Although, with a hemorrhagic stroke or subarachnoid hemorrhage, it can be unbearably strong, but with an ischemic stroke it is quite insignificant. Pain in the occipital part of the head, especially when bending, is always present in the first two cases, but in the latter it may not be present at all.
Therefore, you should not focus only on headaches at the first manifestations. Loss of consciousness can also occur for only a few minutes. Experts recommend that everyone learn a simple technique for recognizing a stroke. Firstly, you should ask the victim to smile, which he either will not be able to do at all, or the smile will look more like a grimace with the corners of his lips downturned.
The second test is to say a simple sentence. As a rule, speech is impaired, but not always. Third, let the person raise his hands up: even if this is possible, one hand will soon slide down or go to the side. You can also look additionally at the tongue, which may fall to one side or be positioned unevenly.
If any of the signs listed above occur, you should immediately call an ambulance, because the hours are ticking. It is believed that the first 3 to 6 hours are of particular importance for healing. This is that precious time during which brain cells that have been “switched off” for a while can start working again.
Before the ambulance arrives, you need to create all the conditions for a horizontal position of the patient, open a window or vent to increase the access of fresh air into the room. It is necessary to monitor the level of pressure and, if it increases, give drugs that reduce it, but not vasodilators.
Headache after a stroke is present, according to statistics, in 8% of cases in people who have suffered a brain disorder. Such symptoms can last from a month to several years, depending on the severity of the disease. Doctors call this manifestation neuropathic post-stroke pain. It can involve not only the head, but also parts of the body that were damaged due to cerebrovascular accident.
Sometimes the symptoms appear simply in the form of numbness, tingling, “goosebumps” all over the body, which can hardly be called pain. In some cases, patients simply suffer from unbearable headaches for a long time. Traditional painkillers are not always effective because they help prevent mechanical pain rather than neuropathic pain.
The fact is that after a stroke the brain perceives pain completely differently. Even previously familiar touches and ambient temperature can cause discomfort. this is due to loss of sensation. Therefore, you do not need to hide your feelings from the doctor, but, on the contrary, even write down detailed symptoms and in which case pain occurs. Only then will the doctor be able to select effective remedies.
Sometimes the pain is not at all associated with a stroke, but is caused by a violation of venous outflow. Therefore, each individual case must be examined by a doctor. The moral support of loved ones is of great importance.
Sources used: provizor.org
Ancillary drugs
You should also remember about various kinds of auxiliary drugs, for example, complexes of vitamins K and E. This group also includes omega-3 acids and ascorutin with folic acid. The first and last components are found in abundance in simple sea fish, so there is simply no need to purchase additional preparations.
It’s worth talking specifically about aids. Many patients simply forget about them, thinking that they have no significance in therapy. This is not so: the pills that a person takes can trigger processes in his body that will cause him to eventually feel a deficiency of some substance (for example, vitamin E). To replenish what was spent, he needs to adhere to all medical recommendations, including when choosing a diet and additional food additives, even if it seems that the advice of specialists is meaningless. If you wish, you can simply clarify the purpose of prescribing a particular medicine - as a rule, doctors answer these questions clearly and in some detail.
Features of manifestations in women
Due to physiological characteristics, the signs of an impending stroke in men and women are somewhat different, although the general picture is similar. Warning signs of a possible stroke in a woman:
- severe headaches appear for no apparent reason;
- numbness of the upper and lower limbs on the right or left;
- vision is impaired, and double vision is often observed;
- Nausea, vomiting and hiccups occur periodically;
- facial muscles weaken, signs of numbness are observed;
- gestures and speech are difficult;
- sensitivity to pain and temperature changes is impaired;
- the patient loses consciousness for a short time;
- attacks of severe dizziness occur;
- convulsions appear (not in every case).
In addition, changes occur in the woman’s emotional state; a depressive state is replaced by attacks of irritability for no reason.
Headaches due to ischemic stroke
Characteristics of pain
Headache occurs in approximately 25% of patients with ischemic stroke. More often it is insignificant or of medium intensity. Only a small number of patients with brainstem localization of the infarction or massive hemispheric lesions experience severe headache.
Patients characterize cephalgia as pressing, squeezing, bursting, reminiscent of a “feeling of heaviness” in the head. They often have limited localization in the temporoparietal region and usually on the side of the ischemic focus (opposite to the paretic limbs).
With a brainstem infarction, headaches affect the cervical-occipital region. Diffuse, diffuse headaches are much less common. They are usually observed with large or multiple infarctions and are associated with severe neurological deficits, nausea, vomiting, and confusion.
Headaches bother patients for several hours or days and then disappear, while focal neurological deficits persist. Only a small number of patients have headaches that persist for a longer period of time. Moreover, the less pronounced the cephalalgia, the faster it disappears.
In some patients (approximately 15%), headaches can be combined with other subjective symptoms: dizziness, nausea, vomiting.
In some cases, headache occurs on the 3-5th day of stroke development, since it is during these periods that the severity of hypoxic edema—swelling of the brain—reaches its maximum.
Diagnostics
The connection between cephalgia and cerebral infarction rarely causes diagnostic difficulties, especially considering the above-mentioned correlation between the severity of focal neurological symptoms, which arise acutely and persist for more than a day, and the intensity of headaches.
When collecting anamnesis in such patients to confirm the diagnosis of ischemic stroke as the cause of headaches, it is necessary to take into account the frequent occurrence of cerebral infarction at night, information about previous transient short-term episodes of neurological deficit (transient ischemic attacks), indications of coronary pathology, peripheral vascular disease, diabetes mellitus, cardiac arrhythmias. A gradual, step-by-step increase in symptoms is typical.
An objective general clinical examination confirms the diagnosis of cerebral infarction by the presence of signs of atherosclerotic damage to the heart and large vessels, a decrease in the pulsation of the carotid arteries, the absence of a significant increase in blood pressure, and the relative preservation of respiratory and cardiovascular regulation.
In neurological status, the main criteria are the predominance of focal symptoms over cerebral ones. The most common defects are asymmetric hemiparesis or monoparesis, often in combination with sensory disorders, speech disorders, and insufficiency of cranial innervation. Consciousness is most often preserved; depression in the form of stupor or stupor is much less common.
The use of additional diagnostic methods is also aimed at confirming cerebral infarction and determining its location.
Computed tomography and nuclear magnetic resonance tomography are considered the most informative in this regard.
Various technical modifications of transcranial Doppler ultrasound make it possible to determine stenotic lesions of the main arteries of the head and arterial system of the brain, and to register changes in the speed of cerebral blood flow.
The presence of an infarct can be visualized using radionuclide angiography. Carotid angiography for the direct diagnosis of ischemic stroke is currently practically not used.
A blood test is aimed at identifying defects in platelet aggregation, such as coagulopathy, and blood viscosity disorders.
Treatment
Treatment of cephalgia in ischemic stroke rarely presents an independent problem. As a rule, adequate pathogenetic therapy implies and is effective in the treatment of headaches.
In those rare cases when the headache is intense and painful, traditional symptomatic therapy is usually prescribed, including analgesics, antiprostaglandin drugs (indomethacin), tranquilizers and (or) small doses of antipsychotics, aspirin in combination with ascorbic acid, carbamazepine derivatives (finlepsin, tegretol) .
Prevention
As for the prevention of headaches during ischemic stroke, it usually means preventing the appearance or increase of edema - swelling of the brain by the 3-5th day of the stroke, which is achieved by adequate, carefully substantiated dehydration therapy. The most effective treatment in this regard is the use of steroid hormones, in particular dexamethasone.
The following signs may be warning signs of ischemic stroke:
- numbness in the limbs or one side of the body;
- dizziness;
- nausea and vomiting;
- severe headaches;
- speech disorders or difficulties;
- development of unsteadiness.
These signs indicate the beginning of the process and it is necessary to immediately take the necessary measures.
As pathological processes in the brain progress, other symptoms appear, which can be divided into three main types:
- acute symptoms, which are characterized by neurological manifestations (more often occur in patients with arrhythmia);
- manifestations of the undulating type, with increasing symptoms of a ciliary nature;
- tumor-like symptoms that occur when the lesion affects the main arteries of the brain.
Ischemic stroke is also characterized by the appearance of cerebral edema and high intracranial pressure.
Diagnostics
Anamnesis is especially important for diagnosis. Whether a person has high blood pressure and diabetes, as well as a family history of atherosclerosis and other types of vascular diseases, plays an important role. This is followed by a simple neurological examination - for example, a “handshake” test. In the case of a stroke, as already mentioned, paresis and plegia occur, therefore, there is a noticeable difference in the strength of the hand grip.
A more detailed diagnosis is additionally performed in the hospital using CT (computed tomography) data, which can be supplemented by MRI (magnetic resonance imaging). Based on the results of these tests, the extent of brain damage is determined, whether ischemia or bleeding is present, and a prognosis for treatment is made for the patient.
Men should know
The warning signs of stroke in men are in many ways similar to the symptoms in women, but they also have their own characteristics. So, you should be wary if you experience the following signs of an impending stroke:
- the appearance of muscle weakness in the limbs (“woolly” legs and arms);
- vision is impaired in one of the eyes;
- shortness of breath of unknown origin appears;
- any part of the body goes numb (upper or lower limb, half of the face or tongue);
- speech is disrupted;
- local headaches occur, or the pain spreads throughout the head;
- attacks of dizziness appear;
- coordination of movements is impaired;
- Nausea and vomiting occur for no particular reason.
In no case should these symptoms be ignored, since a stroke can cause serious problems that can lead to disability or death.
Risk factors
There are several major risk factors for experiencing headaches during or after a stroke.
These factors include:
- women who have had a stroke;
- the young age of the person who will be recovering from a circulatory disorder;
- migraines or a history of a person who has had a stroke;
- an option when the circulatory disorder itself occurs in one of the parts of the cerebellum;
- low blood pressure, or its appearance after a stroke.
How to treat headaches after a stroke
A stroke, or apoplexy, is an acute brain catastrophe that causes severe damage to health. Brain damage occurs after an acute cerebrovascular accident. This is manifested by neurological disorders: personality disorders, paralysis, pathologies of the pelvic organs and headaches of varying intensity. Why do headaches occur after a stroke? Let's look at this question in order.
Headache after a stroke is a natural phenomenon and the main symptom of a stroke. But at the same time, this is an alarming harbinger of a second attack. Therefore, it is so important to pay serious attention to the nature of the pain and its frequency.
Complaints of headaches appear in stroke patients 2-3 days after the onset of the attack. Why do you have a headache after a stroke?
First, it is worth considering the mechanism of the cerebral catastrophe that occurs during hemorrhage. A blood clot formed as a result of hemorrhage changes intracranial pressure and puts pressure on brain structures, as a result of which their ischemia develops. This is the main reason for the occurrence of severe neurological pain, since they develop even with the most minimal change in intracranial pressure.
The pain occurs sharply and suddenly, which is also the main symptom of stroke. It cannot be treated with conventional analgesics. It is accompanied by nausea, repeated vomiting and convulsions.
After overcoming the acute period, the patient's post-stroke headaches can continue for a long time - for 3 months or longer. Subsequently, this condition, depending on the results of the patient’s rehabilitation, may persist, reduce the intensity of the manifestation, or disappear completely.
- cerebral edema resulting from hemorrhage and compression of the brain by a hematoma;
- destruction of nerve cells due to lack of oxygen;
- compression of neck vessels due to muscle rigidity;
- a stressful state turning into depression;
- reaction to certain medications needed in the treatment of stroke;
- hypotension.
Factors contributing to the development of post-stroke headaches are:
- Belonging to the female gender. Women experience this unpleasant symptom 5-6 times more often than men. This is explained by differences in the structure of the female immune and endocrine systems, less serotonin in the brain and periodic fluctuations in the level of sex hormones.
- Age 30-40 years. This group of patients suffers from pain much more often than older people.
- Previously diagnosed migraine.
- Low pressure. It is associated with insufficient cerebral blood supply, which provokes pain.
- More intense pain is typical for patients who have suffered a stroke in the cerebellum or posterior cerebral artery.
Diagnostics
Pain that develops in the post-stroke period has a special character. They make patients suffer from their intensity, reducing the quality of life, making the simplest self-care manipulations impossible. The development of headaches may be accompanied by a decrease in the patient’s intellectual abilities and memory impairment.
To differentiate the diagnosis and select the correct therapeutic strategy, a thorough comprehensive diagnostic study is necessary:
- monitoring blood pressure dynamics to exclude the development of hypertension;
- general blood analysis;
- blood test for sugar;
- echocardiogram of the vessels of the brain and heart;
- MRI;
- psychotherapeutic testing;
- examination of neck vessels.
Therapy
Developed headache during a stroke goes into the post-stroke period and can remain for the rest of his life if the patient is not provided with qualified neurological and psychological assistance. With adequate, timely therapy, headache symptoms go away. Thus, the earlier treatment for stroke is started, the more favorable the prognosis for the patient.
Diagnostics
Only a specialist who will be guided by tests and the results of certain procedures can diagnose the very cause of pain in the head.
These include:
- general blood test of the patient;
- tracking the dynamics of changes in blood pressure;
- MRI;
- conducting an echocardiogram of cerebral vessels;
- conducting a blood test for the presence of sugar and checking its effect on the occurrence of pain;
- conducting consultations with a specialist for those who are on the verge of depression.
Read our article for important information about hemorrhagic stroke in children.
Post-stroke headaches: why they occur and how to treat them effectively
There are many complications that can result from a stroke, and persistent headache is one of them. The occurrence of transient cephalgia after the development of a cerebral catastrophe is considered a normal variant. The sensations are mild or moderate in severity, last no more than 30 days, and their intensity gradually decreases.
At-risk groups
The course of the post-stroke period is influenced by a number of external and individual factors. The risks of developing cephalalgia are higher in people who have suffered a hemorrhagic stroke.
You can learn more about hemorrhagic stroke here.
A large area affected also increases the likelihood of a problem occurring. Severe pain during the rehabilitation period is almost guaranteed if the posterior cerebral artery or cerebellum is damaged.
Groups of people who most often experience headaches during a stroke:
- women – suffer from the symptom 5 times more often due to weaker immunity, a sensitive endocrine system, and systematic fluctuations in hormonal levels;
- young people under 40 years of age;
- persons with a history of hypotension - disruption of the blood channels provokes cerebral circulatory failure;
- people with weather dependence - sensitivity to weather changes is often due to vascular weakness;
You will learn more about weather dependence and cephalgia from this article.
- Migraine patients are people who are initially predisposed to headaches with reduced immunity and problematic blood vessels.
Pathological cephalgia of the post-stroke period is highly pronounced. It negatively affects the general condition of the patient and does not allow him to fully work in accordance with the rehabilitation program. The problem can cause deep depression, from which it is very difficult to lift patients out of it.
Signs of hemorrhagic stroke
Features of the development of hemorrhagic stroke include the following manifestations:
- tingling and numbness in one side of the face;
- spontaneous loss of balance;
- difficulties in speech perception;
- sharp pain in the eyes and partial loss of vision.
These symptoms appear before an attack, but are not always harbingers of a hemorrhagic type disorder.
In case of a violation, the following increasing symptoms appear:
- blood pressure increases, resulting in redness on the face;
- breathing problems;
- paresis (paralysis) of the arms or legs on one side of the body;
- “floating” and chaotically moving pupils, unnatural eye position;
- sagging cheeks, it becomes as if saggy;
- opposite the side on which the area of the brain was affected, the foot is turned toe outward.
If any of these symptoms are present, you should immediately call an ambulance.
Precursors and symptoms of a microstroke
Microstrokes (or mini-strokes) manifest themselves in the form of pinpoint injuries or hemorrhages in the brain.
The duration of such a violation ranges from 2-3 minutes to 1 day.
Micro-strokes are accompanied by the following symptoms:
- feeling weak and overwhelmed;
- headache;
- feeling of being stunned.
Then, to these symptoms are added sharp pain in the frontal region and temples, the appearance of nausea and impaired motor functions. Often, the consequences of a micro-stroke go away on their own and brain function is completely restored.
The task is to stop at the approaches to the brain!
Spinal strokes are acute disorders of the spinal cord circulatory system. This type of disorder can be caused by ischemic or hemorrhagic stroke. Happens more often in old and senile age.
Precursors of this type of disorder include the appearance of the following symptoms:
- pain in the neck, lower back, arms and legs;
- feeling of heaviness in the head;
- noise in ears;
- short-term dizziness;
- headache;
- memory impairment;
- numbness in the legs after a long walk;
- constant feeling of fatigue.
Depending on the location of the disorder, other signs may be added to the listed symptoms.
If there are prerequisites for the development of a stroke, you should not self-medicate and postpone a visit to the doctor. As a rule, for such symptoms, drug therapy is prescribed, which includes taking drugs to protect blood vessels and the brain.
During preliminary therapy, the following medications are indicated:
- antiarrhythmic drugs;
- thrombin inhibitors;
- drugs to lower blood sugar levels;
- medications to thin the blood and prevent blood clots;
- anticoagulants;
- drugs to lower blood pressure;
- sedatives.
In addition to taking medications, you will need to follow some recommendations:
- to refuse from bad habits;
- control blood pressure;
- monitor blood sugar levels;
- follow a diet, the essence of which is to exclude fatty foods, coffee and strong tea.
- spend more time outdoors.
These measures will help prevent the development of stroke and the occurrence of serious disorders, including death.
Treatment
The fight against headaches with anti-inflammatory drugs begins. For each patient, one drug will be better suited than others. Unfortunately, a universal remedy has not yet been invented, and doctors will tell you what to do to alleviate the patient’s condition.
Practice has shown that the use of Paracetamol will also be effective. But you should not take it on a regular basis - liver problems may occur.
In cases where analgesics do not relieve pain, antidepressants can be used. Treatment is carried out in a course.
In order to get rid of headaches after a stroke, the course of treatment must be selected very carefully. The attending physician must apply an individual approach to each patient.
There is not only drug treatment, you can also resort to folk remedies to cope with pain.
Medication
| Antidepressants | Doctors prescribe Fluoxetine, Sertraline or Amitriptyline. It is possible to help the patient’s emotional state and avoid unpleasant moments thanks to the care of relatives. |
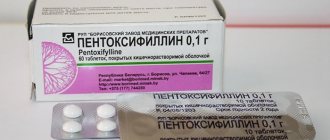
| Painkiller | In order to overcome headache pain after a stroke, Pentalgin, Ketorol and Movalis are often prescribed. Regular Aspirin, Analgin and Paracetamol are suitable for pain relief. |
| Anticonvulsants | These include Lyrica, Gabapentin and Finlepsin. |
Treatment lasts from 1 to 4 months. It happens that it takes time to select the drug that will be most suitable.
Folk remedies
In order to carry out treatment with traditional methods, it is necessary to consult with your doctor. Self-treatment of the consequences of stroke and headaches may be unsafe.