With regard to drug treatment, there has long been an opinion among people that “we treat one thing, we cripple another.” And this is true, since most medications have a number of side effects that are detrimental to health. Even seemingly harmless intravenous administration of drugs can lead to inflammation of the veins. This inflammatory process is called post-injection phlebitis. Let's take a closer look at what pathology is, why the veins become inflamed, and what therapeutic methods are most effective.
Nuances of manipulation: what to pay attention to
It is sometimes said that a nurse has a “light hand.” This statement means that the medical worker is excellent at giving IVs and injections. In such cases, patients feel virtually no pain, and after the procedure there are no marks left on their hands. But most often there is no opportunity to choose a specialist, so all that remains is to observe how the health worker performs the manipulation.
If during the injection the patient feels a strong burning sensation or pain, it is necessary to immediately report this to a medical professional. There is a high probability that the needle pierced the vein and the medicine was injected bypassed. This will cause a bruise.
After the manipulation, the nurse always applies cotton wool moistened with alcohol to the puncture site. You need to press and hold it for about ten minutes. This is necessary to prevent blood from getting from the vein under the skin, as this will cause a bruise. Do not ignore the recommendation and do not throw away the cotton wool immediately after the bleeding stops. If after the dropper only a bruise has formed, but there is no lump, then, first of all, you should apply something cold to the injection site. But this must be done in the first hour after the injection. An accessible and beloved method of dealing with bruises is based on the well-known fact that all vital processes in tissues slow down when cooled. The activity of blood flowing out of the vein under the skin also decreases. But if a lump or hematoma has already formed, let's find out what to do about it.
How to treat
Before treatment, you need to make sure that the lump or lump after the IV does not show signs of purulent infection. Remember, if you have a fever, severe swelling and throbbing pain, you should never self-medicate! You must immediately call a doctor, otherwise the consequences will be very sad.
If we are definitely not dealing with an abscess, then we can cope with the swelling on our own. Firstly, if the swelling appears due to improper placement of the needle and the medication getting into the soft tissue, you need to call a nurse. She will reposition the needle and give some recommendations to combat swelling. Both medications and folk remedies can help.
Drug treatment
For therapy, ointments that contain heparin and/or troxerutin are usually used: Vishnevsky ointment, Ketanov, Methirulacil, Heparin ointment, Dimexide. Apply ointments every hour.
These drugs have contraindications:
- ulcerative-necrotic skin processes;
- increased vascular permeability;
- People with reduced blood clotting should use ointments with caution.
Dimexide is used for compress. To do this, mix the drug with vodka 1:1, and then dilute the mixture with distilled water 1:4. The lump needs to be lubricated with a rich cream (you can use baby cream) to avoid burns. Soak cotton wool or gauze in the solution, apply to the swollen area and cover with film. Leave the bandage on for 7-8 hours.
Among the medications used to combat swelling, Detralex and Magnesia for compress are also used. Never neglect the iodine network - although it is simple, it is a proven and effective remedy. An iodine mesh should be applied to the damaged area of skin 1-2 times a day, at approximately equal time intervals. Be sure to make sure you are not allergic to iodine.
Folk remedies
Traditional medicine is rich in ways to combat swelling after a drip from binge drinking in Moscow. They mainly use compresses, the most popular of which we will now look at:
- Alcoholic. The compress is prepared from water and alcohol, which are mixed in equal proportions. To prevent skin burns, it should be lubricated with a rich cream and only then apply a bandage. We soak a piece of cotton wool, cloth or a cotton pad in the solution and apply it to the seal. Cover the top with film or a plastic bag, add another layer of cotton wool and bandage it. Do not remove the bandage for 5-6 hours.
- Compress made from burdock or cabbage leaves. Take a cabbage or burdock leaf and crush it in your hands until it becomes moist. Then we apply it to the swelling and bandage it. Leaves need to be changed as they dry out.
- From aloe. Aloe is a plant known for its anti-inflammatory effect, so a compress from it will help quickly relieve swelling. The plant leaf must be washed, cut lengthwise into two parts, and the pulp crushed. Apply the resulting paste to the affected area of skin and secure with a bandage. The bandage can be left on overnight.
- Vegetable compresses. Take a potato, cucumber or carrot and grate them. Wrap the paste in gauze and keep it on the inflamed area until the compress dries.
- Honey cakes. Honey helps the seal after the drip to quickly dissolve. To prepare the flatbread, take 1 tablespoon of honey and mix it with a little flour. You can also apply the cake at night.
If hand swelling is accompanied by an abscess, consult a doctor immediately. Self-treatment can lead to even greater problems. The doctor will prescribe a course of therapy or open the “bump” to clean out the pus from it.
Alcohol compress
If a hematoma appears, a regular alcohol compress will help. The alcohol must be diluted with water in equal parts or use vodka. It is necessary to moisten a small piece of bandage, apply it to the bruise, and cover the top with plastic wrap or parchment paper. Next, put cotton wool and bandage it. Leave the bandage on for about forty minutes. The compress must be done every day until the hematoma disappears. In most cases, the bruise goes away in two to three days. Without treatment, it can last up to a week.
Arm veins hurt: causes
In most cases, the causes of pain in the upper extremities are the same factors and diseases that cause a similar symptom in the legs. There are no fundamental differences in the symptoms of these diseases, with the exception of the localization of pain and the degree of its intensity. This is explained by the fact that the legs bear a fairly large load of a person’s weight, so pain in the legs is usually more pronounced.
Paget-Schroetter syndrome
A pathology in which the subclavian vein is blocked (it is in this vein that IVs are most often placed during prolonged infusion). Most often, only one limb is affected, and there is a loss of sensitivity in this area, numbness and the formation of edema. Paget-Schrötter syndrome can be recognized by a characteristic feature: if the patient raises his arms up, one can see a significant increase in the venous pattern, which may acquire a blue or burgundy color.
The pain in this pathology is acute, bursting in nature, the degree of mobility of the limb is impaired, and the person complains of severe heaviness in the injured arm.
Soda
You can also use a soda compress. To prepare the solution, take four tablespoons of baking soda per glass of warm water. Moisten the gauze generously in a concentrated solution, place the cloth on the hematoma, cover the top with film and wrap it with a bandage. The application should be left on for about an hour. The compress helps the seals dissolve and eliminates bruises perfectly. Repeat the procedure until complete recovery.
Clay
A clay compress is also very effective. Mix any pharmaceutical clay in water to the consistency of thick sour cream, apply to the problem area so that all the hematoma and healthy tissue 2-3 centimeters around it are covered. The top of the compress is covered with polyethylene and bandaged. Leave the application on for at least two hours. To improve the effect, clay can be mixed with salt, soda or honey.
Pain in the veins in the elbow and knee joints
Knee pain
Painful sensations localized primarily in the back of the knee joint may indicate thrombosis of the popliteal vein. This is a fairly rare disease - the pathology occurs in approximately 3-6% of patients. Diagnosis of thrombosis in this area is hampered by the lack of characteristic symptoms, therefore, when initially visiting a doctor, completely different diseases (mainly the musculoskeletal system), accompanied by pain in the location of the popliteal vein, are assumed.
Only a thorough examination, including mandatory examination of the veins of the lower extremities using ultrasound, will help establish the correct diagnosis. Patients who have increased body weight or a genetic predisposition to diseases of the cardiovascular system should undergo such an examination once a year for the purpose of prevention.
Elbow pain
Pain in the veins in the elbow area most often appears in combination with the formation of lumps and intensifies with pressure. This phenomenon is typical for patients who were given IVs or had blood taken from a vein. Cubital (post-injection) thrombophlebitis is not dangerous, as it is the body’s reaction to the administration of drugs (when taking blood from a vein - to antiseptic solutions used for treatment).
No special treatment for this pathology is required - local application of ointments (for example, Leoton) is sufficient.
Iodine mesh
Draw a grid on the problem area with iodine. To do this, take a cotton swab, wet its tip in the solution and make a pattern at the injection site, consisting of several longitudinal and transverse stripes approximately a centimeter apart from each other. The main thing is not to cover up the entire hematoma, otherwise a burn may form, because an IV is usually done where the skin is tender and sensitive. Iodine is good at removing bruises and bumps that appear at the puncture site.
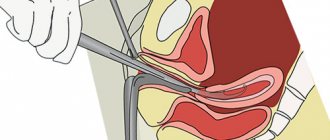
Tissue swelling after injection
If an intravenous injection was performed incorrectly, complications may appear in the form of swelling around the injection site. This means that the needle did not enter the lumen of the vein or came out of it. As a result of this error, the drug enters the surrounding subcutaneous tissue. In this case, the health care worker does not remove the needle, but first withdraws the injected liquid with a syringe. Next, press the injection site with a cotton ball, and only then remove the needle.
If calcium chloride or X-ray contrast agents were administered intravenously, tissue necrosis may begin at the site of swelling. In this case, the healthcare worker should stop administering the drug, quickly remove the needle and inject the affected area with the drug recommended by the doctor. Usually this is a solution of adrenaline or novocaine. A pressure bandage and cold are applied over the affected area. On the third day you can apply semi-alcohol compresses.
Getting rid of hematomas: other tips
At night, apply a cabbage leaf coated with honey to the hematoma. Instead of a vegetable, you can use plantain leaf. A compress made from a mixture of soda and honey is also very effective. To prepare, you need to mix the liquid bee product with soda to obtain a viscous dough. Then it is distributed over the surface of the hematoma and covered with polyethylene, and bandaged on top.
For extensive bruises, thinly sliced potatoes, a gauze bag with which should be attached with a plaster to the injection site and left overnight, help. Repeat the manipulation every day until complete recovery.
Pharmacies sell many drugs that help if your arm hurts after an IV. For example, Troxevasin-gel quickly relieves swelling and promotes the healing of bruises. Heparin ointment resolves blood clots, relieves inflammation and swelling. The good old badyaga is also effective - it will easily help get rid of bruises. Swelling is relieved by massage - stroking and light rubbing of the hematoma are allowed.
The methods listed above for getting rid of bruises are quite effective. If the veins in your arm hurt after an IV and a hematoma, and the discomfort does not stop for several days in a row, such methods will quickly solve the problem.
But what if the damaged area becomes red and hot? This indicates a developing inflammatory process. Unfortunately, complications sometimes arise after an IV drip, which are also accompanied by pain. Most of them are a consequence of improper technique in performing these procedures.
Vein hurts after injection
Have you been trying to heal your JOINTS for many years?
Head of the Institute for the Treatment of Joints: “You will be amazed at how easy it is to cure your joints by taking the product every day for 147 rubles .
In the section Diseases, Medicines, to the question Why does my arm hurt after an injection into a vein? The best answer given by the author Ksenia means the medicine got under the skin.
Our readers successfully use Sustalaif to treat joints. Seeing how popular this product is, we decided to bring it to your attention. Read more here...
Make a compress of vodka or alcohol for an hour.
Perhaps in the hand of t. an air bubble got into the vein, that's a bad thing, but maybe it's a muscle reaction
The crookedness of the one who gave the injection... Most likely, the opposite wall of the vein was caught.
Or maybe the nonsense was dirty
When inserting the needle, it hit a branch of the nerve. It's painful, but not at all dangerous.
I agree with Nadezhda Markova’s advice - you can make a compress. If it gets better, it means the medicine has got under the skin. If not, then my assumption about the nerve is correct.
Talk to the doctors, maybe remove vitamin C? It is also perfectly absorbed when taken orally.
Heparin ointment will help, this happened to me recently, after IVs, the ointment helped.
Pain and swelling after an IV: to summarize what has been said
Many people are interested in whether a hand can hurt after an IV. The reasons are as follows:
- With intravenous injections and drips, damage to nerve trunks can occur. This often happens when the location of the drip is chosen incorrectly, as well as when the vessel supplying the nerve is blocked.
- Thrombophlebitis is an inflammatory process in the area of a vein with the formation of a blood clot. The disease occurs with frequent droppers into the same area of the vein or with the use of blunt needles. Signs of this disease are severe pain at the injection site and redness of the skin. The temperature may rise slightly.
- Tissue necrosis begins when the dropper is placed incorrectly and a sufficiently large amount of medication accidentally gets under the skin. This is possible due to the vein being pierced or not getting into it initially. In most cases, this occurs due to incorrect intravenous administration of the medication. If your arm hurts along its entire length after receiving an IV, what should you do? If necrosis occurs with such a problem, you should immediately consult a doctor.
- A hematoma can also appear during an ineptly placed IV: in this case, a purple spot appears under the skin. This is a consequence of the needle piercing both walls of the vein and the penetration of blood into the tissue. The dropper should be stopped and the injection site should be pressed with cotton wool and alcohol for several minutes. Afterwards, the device is installed in another vein, and a warm compress is applied to the area of the hematoma.
If a severe hematoma appears that does not go away for more than five days, turns red and becomes hot, immediately consult a surgeon or phlebologist.
After the reader has learned why his arm hurts after an IV and what to do about such a problem, he should be more careful about the process.
Post-injection phlebitis: treatment, after a catheter, IV, what to do
With regard to drug treatment, there has long been an opinion among people that “we treat one thing, we cripple another.” And this is true, since most medications have a number of side effects that are detrimental to health.
Even seemingly harmless intravenous administration of drugs can lead to inflammation of the veins. This inflammatory process is called post-injection phlebitis.
Let's take a closer look at what pathology is, why the veins become inflamed, and what therapeutic methods are most effective.
Post-injection inflammation of the veins: what is it?
Post-injection, or post-infusion, phlebitis is an inflammation of the venous walls, which is a complication of intravenous injection or infusion.
Among all types of vascular pathology, post-injection phlebitis is recognized as the most common form.
Administration of the drug through a vein causes vasospasm, provoking a narrowing of the venous lumen, as well as the penetration of infection, and leads to inflammation of the vein walls.
This process is accompanied by a significant slowdown in blood circulation, deterioration of chemical indicators of blood composition, thinning of the tissues of the vascular walls, the formation of stagnation, and the detection of infectious agents in the plasma.
All this increases the risk of blood clots, leading to a serious complication of phlebitis - thrombophlebitis.
Phlebitis caused by infusion is characterized by the following types:
- periphlebitis - inflammation of the subcutaneous tissue at the site of vessel damage;
- panphlebitis - damage to all venous layers;
- endophlebitis is a pathological change in the inner choroid.
Typically, inflammation of the veins after injection is localized on the arms or lower legs, but phlebitis can develop on any part of the body.
Causes of inflammation of the walls of blood vessels
Post-injection phlebitis is formed due to damage to the vein during an intravenous injection or a catheter installed for infusions.
The risk of developing phlebitis depends on many factors. The main ones among them are the following:
- the size (length and diameter) of the needle through which the medicine was administered;
- use of low-quality raw materials for the manufacture of catheters and syringes;
- installation of a device (catheter) for a long time;
- failure to comply with sanitary standards during the procedure;
- ignoring aseptic rules;
- incorrectly calculated dose and high concentration of the administered drug;
- infection (candida, streptococci, staphylococci) due to failure to maintain sterility.
In addition, phlebitis of the vein in the arm can be caused by very rapid administration of a drug (especially solutions of calcium/potassium chloride, glucose, doxycycline hydrochloride) or too concentrated a substance.
After a catheter has been in the vein for a long time, there are frequent cases of infection, which further complicates the inflammation and course of phlebitis.
According to statistics, the development of phlebitis on the arm is most often provoked by self-installation of IVs at home (when removing patients from a drinking binge, ignoring hospital treatment, during urgent emergency care, etc.).
Also at risk are people with drug addiction, who very often inject in places that are far from sterile.
In such cases, the process of inflammation usually begins with damage to the inner layer of the vessel (endophlebitis) with further progression of the pathology.
How does pathology manifest itself?
Phlebitis after intravenous drip or catheterization of veins manifests itself within 24 hours after the procedure and is accompanied by the following symptoms of venous inflammation:
- thickening due to the accumulation of blood at the injection site and protrusion of the vein outward (appears 2-3 hours after the injection;
- pain when moving a limb;
- stiffening (hardening) of soft tissues, detected upon palpation;
- the appearance of a sharp throbbing pain radiating to the fingers, shoulder, thigh (depending on where the injections were given);
- swelling and swelling of the injection area (appears after a few hours);
- redness of the affected area after 24 hours, followed by the appearance of a burgundy tint and blue discoloration;
- increasing swelling on day 2, swelling of the affected area, including surrounding tissues.
Ignoring the above symptoms of phlebitis leads to the fact that on the 3-4th day the limb stops bending/unbending at the knee/elbow joint, hyperemia and infiltration of the vascular walls develops, and body temperature increases (after some time it can reach 39-40°C).
In the future, the signs of venous inflammation only intensify:
- lymph nodes in the armpits and elbows become inflamed;
- suppuration of the walls of blood vessels forms, affecting nearby arteries.
With such an advanced stage of phlebitis, an operation to excise the pus is prescribed.
In addition, post-infusion phlebitis occurs against a background of general malaise, a noticeable decrease in physical activity, and pronounced pain.
Diagnostic methods
If you notice the above symptoms of phlebitis, you should immediately contact a medical facility. A phlebologist treats vascular pathologies.
An experienced specialist, with a thorough visual examination, based on the patient’s complaints and the presence of pronounced signs of post-injection phlebitis, will be able to make a diagnosis.
However, to establish an accurate diagnosis for venous inflammation (phlebitis is often confused with phlegmon of the extremities), additional examinations are necessary:
- general blood and urine analysis;
- blood test for coagulation;
- X-ray and ultrasound of the affected area.
Finding out the full clinical picture of phlebitis will help the specialist prescribe timely and competent treatment, and the patient will avoid severe complications of venous inflammation.
Methods for treating phlebitis
Treatment of post-injection phlebitis is mainly carried out using conservative therapy, but in difficult cases they resort to more radical methods - surgery.
The choice of treatment method for phlebitis directly depends on how much time has passed since the first signs of venous inflammation were detected. If the patient consults a doctor 1-3 days after the onset of phlebitis, a medicinal method of treatment is used.
To avoid complications of inflammation of the venous walls (phlegmon/thromboembolism), treatment of post-infusion phlebitis is carried out in a hospital setting under the mandatory supervision of a vascular surgeon, especially if an acute period of the disease is detected.
Conservative treatment for phlebitis is prescribed for the purpose of antibacterial treatment and detoxification of the affected area, as well as stopping the source of inflammation, increasing blood circulation and restoring venous walls.
For the treatment of post-injection phlebitis, medications are prescribed:
- non-steroidal anti-inflammatory drugs - Ibuprofen, Butadione, Nimesil, etc.;
- angioprotectors that strengthen blood vessels and increase blood flow - Troxevasin, Heparin;
- indirect anticoagulants to reduce blood viscosity and prevent the formation of blood clots - Aspecard, Warfarin;
- fibrinolytics for dissolving blood clots (in complicated cases) – Urokinase, Streptokinase;
- antibacterial drugs - sulfonamides, tetracyclines, macrolides - to eliminate the risk of blood poisoning.
Treatment of phlebitis with the above-mentioned medications is carried out using tablets, topical preparations (ointments/gels/creams), as well as intramuscular and intravenous injections.
If the inflammation during phlebitis is very severe, then they resort to endolymphatic insertion of a catheter needle to accelerate the therapeutic effect of the drugs.
Gauze bandages with a silver solution, heparin ointment, and semi-alcohol compresses are used as local medications to eliminate phlebitis.
When a patient contacts you early (on days 1-2) for phlebitis, physiotherapeutic procedures are often prescribed. However, when inflammation of the veins intensifies (usually on the 3rd day), hyperthermic procedures are strictly contraindicated. It is allowed to apply cold to the damaged area.
If drug treatment for phlebitis is ineffective, they resort to the surgical method. This occurs when the affected area becomes even more inflamed, suppuration begins and blood clots form.
The operation for phlebitis of the veins in the arms is performed in a hospital under local anesthesia and is reduced to removing the formed abscesses. The recovery period after such manipulation lasts about 2-3 weeks.
Doctors recommend wrapping the limb with an elastic bandage on the second day after surgery, as well as ensuring rest and placing the affected arm (leg) on an elevated surface.
Please note that if a surgical incision is made, physiotherapeutic procedures for the treatment of inflammation of the veins in the arms are prohibited.
Ignoring the treatment of post-infusion phlebitis or self-medication is unacceptable, since a complication of the inflammation process is possible, threatening the death of the patient.
Traditional methods of treatment
To speed up the recovery process for post-injection phlebitis, alternative medicine is often used - ointments and compresses based on components of plant origin. However, treatment of inflammation of the vascular walls can be carried out only after consultation with a doctor and testing for the absence of an allergic reaction.
We suggest using the most effective recipes that relieve venous inflammation:
- Honey compress. Lubricate the area of inflammation with liquid honey and wrap it with natural fabric (linen, chintz).
- Applying cabbage leaf. Crumple a cabbage leaf thoroughly washed and scalded with boiling water, spread with honey and apply to the site of inflammation. Secure with a bandage.
- A decoction of beet tops relieves inflammation well. Pour 50 g of dried red beet leaf into 1 liter of boiling water. Let it brew for an hour. Take 150 ml of infusion in the morning on an empty stomach.
- A decoction of currant or rowan leaves. Take the raw material brewed using the above method for venous inflammation 2-3 times a day, 100 ml.
Please note that traditional medicine for inflammation of the vascular walls after injection are additional preventive measures and cannot replace the main treatment of phlebitis with medications.