Cardiologist, Candidate of Medical Sciences, Associate Professor of the Department of Faculty Therapy No. 1 of the Institute of Clinical Medicine of Sechenov University (I.M. Sechenov First Moscow State Medical University).
Area of professional interests: arterial hypertension, cardiac arrhythmias, coronary heart disease, heart failure.
Author of more than 70 publications in domestic and foreign medical literature. Member of the Russian Society of Cardiology (RSC), the National Society for the Study of Atherosclerosis (NOA) and the European Society of Cardiology (ESC).
Author and scientific editor of the series of popular science books “Doctor Rodionov’s Academy”.
Consultation
Hello! Tell me, please, why after the stenting operation (anterior advanced myocardial infarction. Thrombolysis with streptokinase. Coronary stenting 01.10. 16 gsh. HF PA art. NYHA III. Hypertension stage 3, degree 3, risk 4) on the 40th-plus day after the operation, the pressure may drop to 110-100/65-60 mm pc in the morning and evening - already for 2 days (I take: Nebil (1 t per day), Ampril (1 t in the evening - 2.5), alpha- Lipon, Roxera, Brilinta)??
Thank you. Is this normal?
Guaranteed response within an hour
Doctors' answers
You did not indicate what your blood pressure was initially before treatment and when you started taking such treatment. Although a decrease in blood pressure to 11065 cannot be called a shock, especially if the decrease in pressure is not associated with a worsening of the condition or the appearance of chest pain. shortness of breath, cold sticky sweat. Such a decrease in blood pressure may well occur against the background of ongoing antihypertensive therapy (you receive a combination of three drugs - = nebivolol (dose not specified), amprilan and Brilint. All these drugs have a fairly good antihypertensive effect, so when taking them, it may well be possible to reduce blood pressure to such figures. And this is not necessarily related to previous surgical intervention. But nevertheless, if there is a pronounced decrease in blood pressure, it is necessary to call a local therapist at home, and it is also recommended to perform an ECG on the spot.
Cardiovascular tenting is an effective minimally invasive method of treating ischemic processes, which allows mechanically to dilate the vessels of the heart and restore blood flow.
When the coronary arteries are damaged, normal trophism (nutrition) is disrupted. The myocardium does not receive enough nutrients and oxygen. Due to poor blood flow, atrophic processes quickly develop. Further, a heart attack cannot be avoided. Many diseases provoke such a deplorable scenario.
A stent installed in the heart allows you to restore the normal diameter of the arteries and ensure adequate tissue trophism. The procedure as such does not pose any danger, and in capable hands it is an effective tool for treating disorders.
However, the procedure is not always possible. Despite its effectiveness, there are still contraindications. There are also complications. The patient must know what he is getting into and what to expect as a result.
The essence of the method and the expected effect
Stenting is a surgical technique. And like any surgical intervention, it carries certain risks. Although minimal.
During the procedure, the specialist uses special equipment. The doctor gains access to the surgical field through small punctures in the area of the femoral artery. And they move to the heart naturally - through large vessels. This allows you to reduce risks and minimize recovery time after surgery.
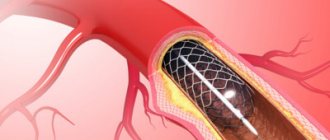
When the specialist gets to the coronary arteries, right (RCA) or left (LCA), he begins work with the affected vessel. A special structure, a stent, is installed into the lumen. It is a mesh, sponge-like frame. It is made from metals, also from alloys, polymers. The choice of material is a separate issue.
Regardless of this, the product is not rejected by the body, does not oxidize, and lasts indefinitely.
The stent rests against the walls of the vessels on both sides and does not allow the artery to close. Maintains the lumen and its diameter at the same level. That's what it's all about: mechanical expansion.
As practice and statistics show, the effect of stenting is significant. The patient can count on good results:
- Blood flow is quickly adjusted. The arteries are no longer narrowed, the lumen is normal. This means that the myocardium will receive enough oxygen and useful compounds. The product itself, due to its shape, does not interfere with trophism.
Shortness of breath after cardiac stenting
Stenting is a medical surgical procedure whose purpose is to install a stent.
It is located in the hollow parts of the coronary vessels of the heart, which makes it possible to expand the focus narrowed by pathology. Any deviations in the tree of arteries cause their narrowing, as a result of which blood flow slows down.
The myocardium experiences a lack of oxygen, gradually losing its normal functioning, which leads to coronary heart disease.
Indications for intervention
The creation and implementation of stents in cardiology is a significant breakthrough in the treatment of coronary artery disease. Improvements are constantly being made to their designs.
The stent itself is a wire tube with corresponding cells, which, once in the affected area of the lesion, is inflated with a special balloon. He pushes the narrowing apart, pressing into the walls of the vessel.
After this, its lumen increases, which improves blood flow to the heart.
Arterial patency can be treated using the following techniques:
- conservative therapy;
- coronary bypass surgery;
- stenting of affected arteries;
- angioplasty.
Drug treatment is not always effective, and the patient continues to suffer from angina attacks. He is offered other techniques, including stenting of heart vessels.
Despite the minimally invasive method, the operation remains an extraneous intervention in the body’s activities. The risks can be serious. Therefore, we must take into account the benefits that should justify them. To do this, a thorough diagnosis of the condition of the heart and arteries is carried out. The issue of the technical feasibility of stenting is being resolved.
Indications for intervention:
- Angina pectoris progresses when an ambulance does not leave the house.
- Early post-infarction angina, attacks of which are repeated, despite attempts at treatment.
- Angina pectoris, which is not affected by medication, but the quality of life is reduced.
- Early prerequisites for heart attack or coronary syndrome.
- Cardiovascular mortality risk found in research.
The patient has undergone surgery. Will he feel relief immediately? Why can pain in the heart after stenting poison your life and make you despondent? This is a natural process of the body adapting to new conditions:
- The very first reason is a change in hemodynamics in the heart and the whole body. It takes time to adapt, and it is individual for each patient.
- The appearance of a foreign body in a coronary vessel causes a confrontation of the immune system.
- Blood clotting is ready for vascular thrombosis, atherosclerosis.
The received chance for a new way of life must be consolidated.
Complications, consequences, risks
Complications are conventionally divided:
Intraoperative, which allows you to see changes during the intervention:
- myocardial rhythm disturbance;
- heart attack;
- detachment of the inner lining of the vessel;
- angina outbreak
- rare possibility of death;
- the need to change the operation to bypass surgery;
Postoperative provocations in the early stages:
- heart rhythm disturbances;
- coronary thrombosis of the stent, causing a heart attack;
- bruising at the site of catheter penetration;
- aneurysm of a vessel with a stent;
Late postoperative changes:
After stenting on the heart, there may be pain in the thoracic region due to such complications. But they do not necessarily accompany the operation. According to statistics, 90% of patients have favorable consequences. Over time, a lasting recovery will occur, blood circulation will stabilize, which will have a positive effect on your well-being.
The doctor warns the patient about the risks before the operation. It’s like in the instructions for drugs, where side effects are indicated, but this is not necessarily their manifestation. Existing risks of stenting:
- Bleeding, blood clots, infection at the catheter site.
- Cardiac arrhythmia, coronary artery rupture, myocardial infarction, blood vessel damage.
- Blood clots in the limbs or lungs.
- Allergy to contrast agents or the medicine used in the stent.
- Stent displacement.
- Kidney failure or stroke.
Rehabilitation and life expectancy
The goal of rehabilitation is a set of measures aimed at:
- Restore heart function.
- Eliminate postoperative negative consequences, especially narrowing of stented arteries.
- Slow down the development of ischemia.
- Increase the patient’s physical capabilities and reduce lifestyle restrictions.
- Improve therapeutic treatment.
- Restore laboratory test results.
- Create a psychologically comfortable situation for the patient;
- Make adjustments to the patient’s lifestyle and health care
The period of hospital stay is insufficient for complete recovery of the body. Cardiac rehabilitation, consisting of a complex of health procedures, will become indispensable in consolidating the results of therapy. A special training program will help you adapt to your new life. It is recommended to spend this period in a cardiological sanatorium. Main rehabilitation measures:
- drug therapy;
- dietary nutrition;
- exercise therapy classes;
- regular doctor examinations;
- educational work.
The patient must understand that surgery is not a treatment for the underlying disease. He continues to suffer from atherosclerosis. Relief after stenting should remind you of the fight against cholesterol.
Therefore, the duration of existence on earth is in the hands of the patient. Each patient has his own individual capabilities of the body and associated pathologies.
By following the doctor’s recommendations, the essence of which is a healthy lifestyle, a change in attitude towards nutrition, and restoration of metabolic processes, you can live happily ever after.
Assignment of disability
Stenting of coronary vessels is not a reason to receive a disability group. The operation is aimed at restoring the patient's health and performance. But restriction of work activity in the presence of the illness for which it was carried out can lead to it, for example:
- Disability group 3 is assigned to patients who have suffered a heart attack without any particular impairment of the left ventricular function or angina pectoris.
- Disability group 2 is assigned in the case of heart pathologies that lead to restrictions on movement and work activity.
- Disability group 1 is given to patients with cardiac pathology in the form of angina and heart attack who have lost the ability to self-care.
Restoring loads after stenting
If the operation was successful, then after a rehabilitation course the patient can return to his previous life. The most important thing for a person is his work activity.
The sphere of intellectual work allows you to get involved in work immediately. Labor associated with physical activity has time limits.
You need to check yourself for the possibility of stress in any weather, to what extent after stenting it does not cause pain in the heart vessels.
It is active loads that are relevant in restoring your former life:
- They are assistants in assessing the ability to cope with everyday life.
- Activity in the form of walking, swimming, cycling helps improve the functionality of the cardiovascular system.
- With physical activity, the progress of atherosclerosis is inhibited, the myocardium is hardened, hypertension is stabilized, and fats are burned
Source: https://ogomeopatii.ru/odyshka-posle-stentirovanija-sosudov-serdca/
Indications
There are quite a few reasons for this:
- Cardiac ischemia . Classics of cardiology. This term refers to a secondary process in which the muscle active layer is poorly supplied with blood. Why this happens is another question.
Typically, trophic disorders develop as a result of other abnormal conditions and diseases. Whether it is a heart attack, an inflammatory process of an autoimmune nature, rheumatism or an infectious lesion. There are plenty of options.
Coronary stenting allows you to quickly and effectively restore nutrition and cellular respiration. Sometimes it’s a matter of preserving life.
- Angina pectoris. A typical condition, it is classified as pre-infarction. The bottom line is the same insufficient supply of blood to the organ. But this condition occurs in episodes. Each attack is accompanied by pain, shortness of breath, and rhythm disturbances.
Without treatment, the patient is at serious risk. Subsequent episodes become stronger, and the likelihood of a heart attack is much higher.
- Atherosclerosis of different types. As a rule, when fat is deposited on the walls of blood vessels, cholesterol plaques form. They naturally mechanically block healthy blood flow. Interferes with myocardial nutrition. In this case, the lipid deposits are removed before installing the stent, but this cannot be done if the plaques are calcified.
There is another form of the pathological process. When the coronary arteries narrow steadily, they remain in a spasmodic state for a long time. Most often, this is observed in experienced smokers and alcohol drinkers. Also in patients with hypertension and some other categories.
- Significant risk of myocardial infarction. Associated with previous diagnoses and disorders. In such patients, the likelihood of an emergency condition is much higher.
- Coarctation of the aorta. Congenital malformation. Typically, narrowing of the largest artery at its exit from the left ventricle. Blood flow is seriously complicated. Stenting is performed immediately after the pathology is detected. Age doesn't matter. This is an obvious advantage of the procedure. Without medical care, the risk of death is high.
- Conditions after a heart attack. Stent placement can be an effective measure of secondary prevention and at the same time treatment if the patient has suffered an acute circulatory disorder, but the cause remains in place.
There are many indications. But all of them, one way or another, come down to processes when the coronary arteries (also the aorta) are not able to do their job. Due to narrowing or blockage.
Why is there low blood pressure after a heart attack?
The occurrence of heart attacks at low pressure (hypotension) can be caused by the following factors:
- relapse of cardiac dysfunction (for example, if hypotension is provoked by a history of necrosis of the myocardial zone);
- a sharp jump in blood pressure;
- vascular pathologies, etc.
However, even with normal or low blood pressure, its level decreases after a heart attack. The lower limit of systolic pressure is fixed 24-72 hours after the development of pathology.
Low blood pressure after a heart attack persists in the acute, subacute and cicatricial stages. The cause of hypotension is a decrease in the resistance of the entire vascular system and the contractility of the heart due to the formation first of a zone of necrosis, and then of a scar in place of the functional tissue.
When a large volume of the heart muscle is damaged, cardiogenic shock develops: the upper pressure reaches values below 80 mm Hg, the patient experiences weakness, dizziness, fainting, sudden cooling of the extremities, and frequent weak heartbeat.
Changes in blood pressure indicate the risk of recurrent blood supply disruption. For patients whose pressure after a heart attack stabilizes within several days and remains within normal or elevated values, the treatment prognosis is positive.
Important information: Consequences of extensive myocardial infarction and chances of survival
Contraindications
There are not many reasons to refuse the procedure.
- Intolerance to iodine preparations. The stenting operation is performed under radiographic control. This is necessary for precise advancement of a thin surgical instrument along the bloodstream. Allergic reactions are checked before intervention. The drug is administered subcutaneously in a minimal volume, then the body’s response is monitored.
- Significant narrowing of the lumen of the arteries. If the diameter is less than 3 mm, minimally invasive surgical treatment is not possible.
- Significant affected area. When a whole group of arteries is narrowed or a large area of stenosis is observed. There is no point, since the stent will not cover such significant volumes and will not restore blood flow. Other methods are needed.
- Coagulopathies. Diseases in which blood clotting is impaired. The problem is solvable, the contraindication is relative. Once the condition returns to normal, surgery can be performed.
- Severe dysfunctional disorders. Respiratory, renal failure. Since the contrast enhancement drug can provoke bronchospasm or intoxication due to poor excretion.
- Inflammatory processes. Infectious or autoimmune.
There are also obvious contraindications: such as mental disorders, when the patient is not able to control behavior, and some others. In general, there are minimal reasons to refuse the procedure.
Indications for stenting surgery
Installation of a stent on the arteries of the heart has a number of indications. In each individual case, the doctor assesses the need for such an operation and prescribes it only when other methods of treatment without surgery are unsuccessful. The main indications for stenting are outlined below:
- ischemic disease in a chronic form, which is accompanied by the development of atherosclerotic plaques that block the arterial lumen by more than half;
- angina attacks that occur with light exertion;
- the likelihood of developing myocardial infarction in combination with coronary syndrome;
- myocardial infarction (extensive or small) in the first 6 hours with a stable body condition;
- re-closure of the arterial lumen after balloon angioplasty, bypass surgery and stenting.
Types of stents and their service life
There are three types of products in total. If we take the material as a basis.
Made from stainless medical steel
Most often used. To create it, inert metals are used, but they are strong enough to withstand heavy loads in vessels. There are no downsides, at least not obvious ones.
Unlike more modern analogues, they can be rejected. But this is an extremely rare situation, the likelihood of encountering such a problem is small.
They are cheap and therefore available to a wide range of patients and medical institutions. A steel stent is the most common type.
Alloy products
The fundamental difference lies in the material. It can be cobalt-chrome or platinum-chrome. They do not oxidize, do not tear away and better withstand significant mechanical loads. The cost is slightly higher, which is why such stents are used much less frequently.
Structures made of polymer materials
For example, polymer made of polylactose acid (PLLA) or coated with them are the most modern stents for cardiac vessels.
They can also act as a depot for medicines and be:
- Coated, they release a drug that reduces the likelihood of future narrowing of the artery.
- With double coating - external and internal, to heal the vessel itself and prevent thrombus formation.
- Coated with antibodies that attract endothelial cells, reducing the risk of thrombosis.
- Dissolving, made from a material that dissolves and releases a drug coating that prevents the recurrence of stenosis.
Such stents are installed when there is a high risk of relapse. The cost is significant and they are available to a small number of patients.
According to the structure of the product there are:
- mesh (made of woven mesh);
- tubular (from a tube);
- wire (made of wire);
- ring (from separate rings).
The classic option is mesh ones, which have a rounded frame that expands the lumen of the vessel.
Preparing for stenting
- General blood analysis. To exclude inflammatory processes at the moment before surgery.
- Biochemical research. Baseline values are checked, including alkaline phosphatase, liver levels, and markers of possible inflammation.
- Chest X-ray. Panoramic. The task is to exclude damage to the lungs and bronchi. Pulmonary diseases often prevent surgical treatment.
- Electrocardiography. To identify functional disorders of the heart.
- ECHO-CG is prescribed to exclude structural pathologies of the muscular organ.
- Coagulogram. Determination of blood clotting rate.
In addition to the preparatory activities themselves, general tests, specialized techniques are prescribed. Their task is to examine the surgical field in more detail. Coronary angiography is mainly used. Essentially a contrast x-ray.
All activities are compulsory. As for the latter, it is carried out with caution. There are many contraindications. Including hypertension and a group of others.
Causes of pain in the early postoperative period
Stenting is considered a fairly effective way to restore coronary circulation in cases of damage to the coronary arteries of the heart. This operation can remove the consequences of atherosclerosis, but not its cause (smoking, hypertension, dyslipidemia, age).
Therefore, angina attacks may return in the early and late postoperative periods, especially if the patient does not stop smoking, drinking alcohol, does not follow a diet, or neglects recommendations for taking medications.
Less commonly, pain syndrome is associated with damage to the arterial wall during surgery, incorrect selection of the stent size, or the formation of a false aneurysm. Postoperative blockage of the installed vascular scaffold is also possible. Its risk increases with:
- high blood coagulation activity;
- liver and kidney dysfunction;
- saccharin diabetes (the most common factor);
- arterial hypertension;
- atrial fibrillation.
Repeated narrowing of the lumen (restenosis) is associated with the anatomical features of the arteries (less than 2.5 mm in diameter) and widespread atherosclerosis (more than 20 mm in length).
The surgical technique itself, which involves crushing an atherosclerotic plaque with the introduction of its parts into the artery wall, can serve as a source of repeated thrombus formation in this area. After plastic surgery, the artery collapses in response to stretching (negative remodeling), sometimes its lumen outside the stent becomes smaller than before the operation.
To prevent complications, special drug coatings on stents and special materials are used, which can be absorbed over time, which reduces the risk of inflammation in the postoperative period. All patients are also prescribed anticoagulant therapy and vasodilators.
We recommend reading the article about stenting after a heart attack. From it you will learn why stenting is performed after a heart attack, about angioplasty, possible complications after and about the treatment of the patient. And here is more information about rehabilitation after bypass surgery.
Progress of the operation
Surgery begins with local anesthesia. It is important to eliminate sensitivity in the projection of the femoral artery. Premedication with the use of drugs for sedation is possible. This allows you to reduce anxiety and overcome the feeling of fear.
Next, the procedure is carried out according to a clear algorithm:
- Doctors make an incision.
- A special instrument is inserted through it.
- At the same time, a contrast agent is infused intravenously. To get a clear picture on an x-ray.
- The catheter is advanced along the bloodstream to the heart.
- As soon as they reach the surgical field, they begin directly to install the stent. This is the most crucial and difficult moment. The final result depends on the technique and quality of execution.
Everything takes about 2 hours. Plus or minus. Depends on a situation.
There may be some discomfort immediately after surgery. Pain in the sternum, shortness of breath, burning sensation in the projection of the heart. This is fine.
No special correction is required. But the patient should tell doctors about all violations. To avoid complications and undesirable consequences. Because there is a risk of developing them.
After surgical treatment, the patient is placed in the intensive care unit. There he stays for a day or a little less. Depending on how the early recovery period proceeds.
Then the person is transferred to normal conditions, and after 2-3 days or less the patient is discharged. Recovery continues at home.
Basic principles of physical activity
Physical activity should lead to the following positive aspects:
- improvement of peripheral blood circulation;
- increasing reserve breathing capacity;
- increasing muscle tone;
- stimulation of metabolism in the heart muscle;
- improvement of trophic processes in the myocardium;
- the heart muscle is strengthened and its ability to contract improves;
- the number of complications decreases and they resolve more easily;
- the wound heals faster after surgery;
- rehabilitation is accelerated, blood circulation improves throughout the body, and with this the functioning of all human organs improves, vitality and mood increase, recovery and return to normal life are faster.
Rehabilitation
Restoration measures are simple. However, you need to strictly adhere to the regime; this is a matter of a qualitative return to normal.
During the first month, the following measures are indicated:
- Refusal of intense physical activity. But they cannot be completely excluded. Walking and light walks in the air are recommended. You need to carefully monitor your pulse.
- Blood pressure control. Patients with hypertension should continue to take prescribed medications.
- Avoiding overheating. In the sun or in artificially created conditions: bathhouse, sauna, hot bath.
- Patients should also not overuse salt. The diet is gentle, with a sufficient amount of fresh vegetables and fruits, lean meats. Do not use hot seasonings.
- Alcohol and cigarettes are strictly prohibited. For at least a month. The ideal option is to completely give up bad habits during this time and eliminate addictions from your life.
By the end of rehabilitation after stenting of the heart arteries, an ECG and ECHO are performed to assess the quality and results of therapy. A positive outcome is stated if the blood flow is restored or at least mostly normalized.
After surgery
After CABG surgery, patients are divided into two groups - those whose further condition is stable or complicated. In case of complications, first of all, drug therapy is carried out to bring the body out of a serious condition. If there are no complications, or they are relatively minor, then five periods are distinguished for a person recovering from CABG surgery:
- Early, from one to three days. Breathing exercises are done without body movements, the patient clears his throat, turns on the sides, movements of the feet and palms are also acceptable. Breathing exercises - inflating balloons. Classes last about ten minutes.
- The second period is called the ward period, lasting from 4 to 6 days. Movement of the arms, torso, and legs are added; you can imitate walking, but while being in a lying state. Classes last about twenty minutes.
- The third period is characterized by low training loads, from 7 to 15 days, that is, from a week to two. Breathing exercises are performed both statically and using arms and legs; you can walk, but not much. Classes last about 30 minutes.
- In the fourth period (from 16 to 25 days) you can do physical activity of moderate difficulty. You can walk more, and it is useful to speed up and slow down; the head and torso are involved in the exercises. Classes last about forty minutes.
- In the fifth period after CABG, complicated training is allowed; it lasts from 26 to 30 days, when they are usually discharged from the hospital. Lesson duration is up to 50 minutes. It is useful to climb the stairs and go outside.
Possible complications
Negative consequences are extremely rare. Basically, negative results are associated with the actions of the patient himself. If he does not comply with the regime, does not adhere to the doctor’s recommendations, the risks increase many times over.
Possible complications include:
- Thrombosis. When blood vessels are damaged, blood can thicken and clog their lumen. Thrombosis is the most common of all complications after stenting. To prevent such a scenario, doctors prescribe anticoagulants or milder drugs based on Aspirin, and other modern analogues. They are not taken for long, only while there are risks.
- Acute disruption of blood flow in the myocardium - infarction, as a consequence of thrombosis.
- Severe pain. To varying degrees, discomfort is always present. But this is a temporary disturbance.
- Dyspnea.
- Heaviness in the chest.
- General poor health. This is normal. It lasts from a day to several. Then it goes away without outside help.
Complications are unlikely, especially if the patient responsibly follows the doctor’s instructions.
Methods of dealing with pain
The intensity of discomfort in the heart can be affected by:
- complete cessation of smoking and alcohol abuse;
- proper nutrition with the exception of fatty foods of animal origin, partially hydrogenated oils (margarine, sauces, industrial desserts), sweets;
- the menu must necessarily include: fish, nuts, legumes, lean meat, low-fat dairy products, whole grain cereals, fresh and boiled vegetables;
- dosed physical activity to improve the adaptation of the heart muscle to the presence of a stent;
- control and correction of blood pressure, blood sugar and cholesterol.
Watch the video about rehabilitation in cardiology:
A prerequisite for maintaining adequate patency of the coronary vessels is the use of:
- anticoagulants (Warfarin);
- antiplatelet agents (Thrombo Ass, Plavix, Curantil);
- vasodilators (Cardiket, Monocinque, Diacordin);
- lipid-lowering drugs (Simgal, Liprimar).
Properly selected drug therapy improves the rheological properties of the blood and relieves spasm of the coronary vessels, thus reducing the causes of pain in the heart after stenting. If necessary, Nitroglycerin along with an Aspirin tablet may be additionally recommended to relieve attacks.
Forecasts
Prognostic assessments are generally favorable. The operation was well tolerated, the likelihood of negative effects is minimal.
After the intervention, patients return to normal life. If treatment was carried out at an early stage of ischemia, there is every chance of complete recovery and getting rid of the pathology.
Stenting of the coronary vessels of the heart is an effective method of restoring blood flow in the organ. The risks are minimal. They are fully compensated by the effect of the operation. But the patient must adhere to the rules of rehabilitation. The results depend on the moment when the correction is made.
Features in men and women
The clinical picture of pathology in patients of different sexes is different:
- In men, in the most acute stage, hypertension and tachycardia are recorded, the nature depends on the course of the disease. Hypotension is observed the next day after the cessation of blood supply to the heart area.
- During a heart attack, a woman’s upper blood pressure may be low or normal. The pulse often changes slightly. Hypertension in the most acute stage of the lesion is not an exceptional or rare phenomenon, however, the absence of severe pain and sudden changes in blood pressure and heart rate are observed more often in women than in male patients.
The characteristic chest pain, increased pulse rate and pressure during myocardial infarction in men allows for timely diagnosis of the pathology and resort to effective first aid methods. The erased clinical picture and the absence of significant changes in the levels of heart rate and blood pressure prevents a correct diagnosis without additional laboratory and instrumental tests, therefore, in women, necrosis of the heart muscle is more often complicated by severe cardiac dysfunction and death.
In addition to the manifestations, the risks of pathology also differ: myocardial infarction in women under 65 years of age occurs 2.5-3 times less often than in men of the same age group. This is due to both lifestyle (stress, nutrition and timely treatment) and hormonal factors. In patients over 65 years of age, the gender difference in the risk of this cardiac disorder decreases.