Summer is the season with the longest and hottest days. This is also the time when most travel takes place. More and more people with chronic conditions want to travel and are seeking medical help for this.
The question of when you can fly on an airplane after cardiovascular pathologies is always decided individually. Before any trip or holiday, patients with chronic health conditions should schedule a medical examination to discuss with their doctor whether they can travel and what health recommendations they should follow while traveling.
Who shouldn't fly
Travel is not recommended for patients with cardiovascular diseases during periods of exacerbation. These are the following types of illness: decompensated heart failure, angina with frequent chest pain, periods of high blood pressure that cannot be controlled by drug therapy. In the first month after acute myocardial infarction, after cardiac or vascular surgery, travel should be postponed.
Avoid travel to altitudes above 1500 m and in very warm and humid areas. An increase in altitude can lead to an imbalance in the cardiovascular system of a patient with hypertension or coronary heart disease (angina pectoris, myocardial infarction). Long trips are not recommended when you have to spend 12-16 hours on the road.
Ideally, patients should always have a copy of their most recent examination or medical record of the ailments they suffer from and what treatment they are receiving. Treatment does not stop with rest, because illnesses do not take vacations. Heart patients take with them a supply of medications as prescribed by their doctor. You need to take as much as is enough for the entire trip (especially if you have to travel outside the country).
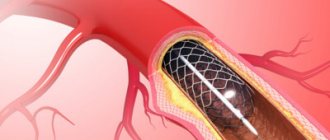
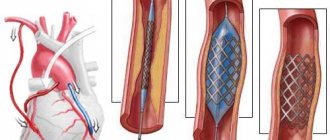
Rehabilitation after stenting
Stenting of the heart arteries can greatly improve the patient’s quality of life, but this operation does not stop the atherosclerotic process and does not completely cure coronary heart disease.
Rehabilitation after stenting of the heart arteries includes: drug therapy, physical therapy, diet, lifestyle changes in general: quitting smoking, normalizing body weight if necessary.
The doctor selects drug therapy and exercise therapy for each patient individually.
Who can fly
Airplane travel is not prohibited for patients with heart disease if the disease is properly diagnosed, treated and stabilized, and provided that precautions are taken. On board an aircraft, patients with cardiovascular disease may require aisle seating to be able to perform light exercise (on long journeys) and may require oxygen if necessary.
Classification of heart attack
If obstruction occurs in arteries of medium and small caliber, a small focal infarction develops. Located under the inner (subendocardial) or outer (subepicardial) membrane. It responds well to treatment, and complete clinical restoration of cardiac function is possible.
When can you fly on an airplane after a small focal heart attack? The early rehabilitation period takes 14 days. After 2 weeks of recovery, in the absence of complications, flights are allowed.
Blockage of the main coronary arteries leads to necrosis of the entire thickness of the wall of the left ventricle or septum - transmural infarction (large focal). Often leads to serious complications:
- acute aneurysm;
- gross conduction disturbances of the nerve bundles of the heart;
- acute heart failure, cardiogenic shock;
- myocardial rupture, hemotamponade of the cardiac membrane;
- acute cardiac arrest.
If enough time has passed after the heart attack, there are no complications, the body has fully recovered and is functioning normally, the person can easily fly on an airplane
When can you fly after a large focal myocardial infarction? Considering the extent of damage to the heart muscle and natural heart failure, the rehabilitation period lasts six months. With effective treatment, stable electrocardiogram readings, and the absence of acute complications, you are allowed to fly on an airplane 6 months after a heart attack.
Possible risks
The risk of prolonged air travel is the risk of blood clots forming in the veins of the lower extremities due to lack of mobilization during flight, dehydration and small space that does not allow movement. There is also a risk in patients with obesity, varicose veins, and a history of thrombophlebitis on long trips. Hydration and regular leg movements will greatly reduce this risk.
It is impossible to say when two different people can fly. Different situations may occur. Air transport is the safest means of transport for hypertensive patients, but a patient with controlled blood pressure can travel by almost any mode of transport. In most patients, blood pressure tends to decrease during periods of high fever, due to insufficient hydration and vasodilation. Thus, blood pressure drops below normal levels, accompanied by symptoms such as headaches, dizziness.
Proper hydration and drinking at least 2 liters of fluid per day, visiting a cardiologist to adjust antihypertensive medications can prevent these situations. You should not try to change your medication dose alone. The attending physician will take into account both the condition of the heart and other conditions that matter, and the climatic characteristics of the holiday destination. We must remember that cardiac patients are more susceptible to dehydration than others.
Flying after a heart attack can be risky, especially in the summer. Through sweat, you lose a number of minerals that your body needs. Thus, potassium losses may be asymptomatic in a healthy person, but can cause palpitations and cardiac weakness, especially if diuretic therapy is carried out in parallel. Coffee and alcohol should be avoided in summer because they can dehydrate the body.
Patients with pacemakers, cardiac resynchronization devices and electrical defibrillators must undergo special checks made in accordance with aircraft operating schedules.
You can fly on an airplane only if you are absolutely sure that you are in a safe condition. To ensure an enjoyable holiday without any untoward health events, visit your doctor before departure and follow the recommendations you receive. People with heart disease are rarely able to fly safely on airplanes. The stress of check-in, customs clearance, boarding, immobility in the cabin, fear of theft and decreased oxygen levels in the blood are all unfavorable conditions for people with fragile hearts. Hypertensive patients need to fly by plane in such a way that they can quickly get to the tail compartment. Here he can warm up and do a couple of simple exercises to get his blood flowing.
How to make a safe flight after surviving myocardial necrosis
It is impossible to definitively answer the question: is it possible to fly on an airplane after a heart attack? The past illness imposes a strict ban on upcoming travel only if the rehabilitation period has not yet ended.
Myocardial infarction means damage to the heart in which necrosis of an area of the heart muscle occurs. Depending on the volume of damage, there are large and small focal forms, extensive (transmural), intramural, subendocardial, subepicardial infarction.
The duration of the rehabilitation period ranges from several weeks for small-focal heart attacks and several months for large heart attacks. During the recovery period, the motor regimen is expanded, physiotherapeutic measures and exercise therapy are carried out.
Not everyone with high blood pressure knows whether hypertensive patients can fly on an airplane. Hypertension and an airplane are hardly compatible concepts. People who have a problem with high blood pressure are not recommended to use air transport, since in such cases there is a considerable risk of a heart attack or hypertensive crisis.
The fact is that during takeoff or landing there is a sharp change (drop or jump) in atmospheric pressure. Before flying anywhere, people with high blood pressure need to carefully prepare for such a trip in order to minimize the stress on the body during travel.
Despite the fact that an artificial environment is created in aircraft cabins, a special microclimate that makes it possible to regulate air humidity and temperature, during landing and takeoff the atmospheric pressure changes greatly.
Changes in atmospheric pressure during takeoff and landing are felt even by a person who does not have problems with blood pressure, so at this time you need to sit with your mouth slightly open and yawn. To prevent unpleasant symptoms, passengers are offered drinks, because small swallowing movements make it easier for a person to tolerate surges in atmospheric pressure.
Flying on an airplane with hypertension is also dangerous because the volume of oxygen is significantly reduced during the flight, and this, in turn, causes an increase in blood pressure. For hypertensive patients, this condition can become critical, as it often provokes a heart attack.
A long flight not only increases blood pressure - a person spends a lot of time in one position in an airplane seat, and the legs may swell during long periods of sitting. This occurs due to a drop in the normal rate of blood circulation in the extremities - due to compression, the arteries and veins become very narrow.
It should be noted that during the flight, the air humidity in the cabin is greatly reduced, and due to the reduction in oxygen volumes, oxygen starvation may begin: a disruption in the functioning of the gastrointestinal tract occurs, and a dry throat is felt, causing a cough. You cannot fly by air under the following conditions:
- mental illness;
- recent heart attack or heart surgery;
- with uncontrolled arterial hypertension;
- with thrombosis or thrombophlebitis;
- with pneumonia.
Patients suffering from these pathologies should change air travel to a safer option. But if you still need to fly, you need to consult a doctor before boarding the plane - he will tell you how to avoid possible complications.
But the question of whether it is possible to fly on an airplane with hypertension should not always be answered in the negative. This is acceptable, but it all depends on the stage at which the disease is. For example, you cannot stay on an airplane if you have stage 3 or 4 hypertension, after severe vascular complications (heart attack, stroke).
If the doctor has allowed you to fly and high blood pressure in this case is not particularly dangerous, then you can go on an air trip, taking into account some recommendations and rules that will help reduce the load on the body.
With modern airlines you can order this device several days before your flight. In most cases, it is paid separately as it is an additional service. The reason for submitting an application for a pillow may be a special recommendation or prescription from the attending physician.
It's best not to fly alone. So, on board with a patient suffering from hypertension, there should be a loved one who knows what measures to take if necessary (if the condition suddenly worsens).
We invite you to familiarize yourself with the recommendations disseminated by Aeroporti di Roma (the organization that controls Rome's airports), compiled under the leadership of Dr. Carlo Racani.
Conditions of increased stress on the heart in patients with chronic heart failure can cause deterioration in its functioning and the appearance of symptoms.
Air travel can affect the course of heart failure due to the following unfavorable factors:
- a decrease in air pressure at high altitude and an associated decrease in the partial pressure of oxygen in the blood,
- low humidity in the aircraft cabin, leading to the risk of dehydration,
- worsening of other diseases that cause a lack of oxygen supply (lung diseases, anemia),
- psychological and physical stress associated with travel (queues at check-in and security checkpoints, carrying luggage, worries about flight safety)
Despite this, flying is not contraindicated for persons with chronic heart failure, but requires certain precautions.
Changes occurring at high altitude are well tolerated in cases of stable heart failure, but those at risk include those with signs of circulatory instability.
1. Have it in your hand luggage
- Sufficient amount of medications normally taken for the duration of the flight,
- Emergency medications, such as diuretics and nitrates,
- A document summarizing your medical condition
- Recent electrocardiogram
- Contacts of the attending physician
2. Have it in your luggage
- Sufficient for the duration of the trip
- the number of medications usually taken,
3. If you need oxygen inhalation during the flight, notify the airline at least a week before departure,
4. Get up and walk around frequently during the flight
5. Avoid heavy foods, caffeinated drinks and alcohol
Patients with heart failure who report shortness of breath, palpitations, and fatigue with mild exertion (ie, NYHA class 3) should be evaluated by a cardiologist before travel.
Air travel is contraindicated for passengers with symptoms of heart failure at rest (NYHA class 4).
Passengers with implanted pacemakers (pacemakers) and defibrillators must follow special recommendations.
- The correct operation of the device must be checked no later than in the last 6 months before the flight
- Always carry the necessary medical documentation with you
- Don't go through the security gate
What to do if the condition worsens
The cabin crew has the means and knowledge of first aid techniques. He is required to have an emergency medical kit on board and a defibrillator. It is also worth knowing that permission for an emergency landing is not always easy to obtain, and even if it is technically possible to land, it is still necessary that medical resources are available for medical emergencies and the ability to effectively prevent such situations.
Most major airlines have defibrillators on board. Even if the plane is pressurized, the barometric pressure on board is lower than on the ground. During flight, the pressure in the cabin corresponds to that at an altitude of 1500-2000 meters above the sea. This drop in pressure leads to a decrease in oxygen content and, as a result, expansion of gases inside the body cavities. In a healthy passenger, physiological mechanisms are compensated. For a passenger with heart disease, things happen differently.
A person who has had an uncomplicated myocardial infarction will have to wait at least two weeks before flying. In case of complications, this period will be extended to six weeks. After bypass we are talking about three weeks and 10 days after angioplasty.
Doctors recommend that travelers who have heart problems or complications of heart problems obtain insurance that covers medical expenses. It is also good to obtain travel approval from the airline with which the person intends to travel. While in-flight cardiac arrests are uncommon, crews never take sufficient precautions to avoid them.
When can you drive after a heart attack?
To avoid further spread of necrosis in the area of the heart muscle, a person who has suffered an attack should constantly be at rest. Stressful work and excessive worries must be eliminated for successful recovery from illness. In turn, surviving a myocardial infarction is not an obstacle to further employment if the victim adheres to the doctor’s recommendations during rehabilitation. The return of such a patient to the wheel should be gradual and thoughtful.
Is it possible to drive a car after a myocardial infarction?
The only limitation in choosing a field of activity is heavy physical labor, which increases the load on the heart. If rehabilitation after myocardial infarction and stenting is successful, the person can return to driving, constantly increasing the selected distance. For the first time, it is necessary to have a second driver nearby to monitor the condition of such a patient and be ready to replace him if necessary.
First of all, it should be understood that myocardial infarction is a complex, life-threatening emergency situation from which no one is immune.
A quick return to driving is hampered by concomitant pathologies of the circulatory system, namely:
- various manifestations of arrhythmia (tachycardia, extrasystole);
- pain in the heart area;
- periodic attacks of angina (increase the risk of a recurrent attack when such a patient is driving);
- severe weakness, dizziness (indicate the presence of a pathological process);
- sudden changes in blood pressure.
People who have suffered a myocardial infarction should listen carefully to their body. An unexpected increase in anxiety in a professional driver indicates an incomplete rehabilitation period. Lack of confidence in yourself and your actions precludes long-term driving.
A driver who has suffered a heart attack usually feels great at the beginning of the trip. The longer he drives, the harder it is for him, which is worth remembering during the rehabilitation period.
How long after a heart attack can you drive?
Driving a car requires increased concentration from the driver. Pain and frequent dizziness exclude such types of activities. Since after a heart attack a dead area forms on the heart, the remaining cells are forced to function in an enhanced mode, which increases possible risks. Stabilization of a sick person’s condition is accelerated by taking appropriate medications and maintaining a calm environment at home and at work.
How long the recovery period will last for a particular person, how long he can live after an attack, depends on many factors
Recovery after myocardial infarction occurs in several stages:
- inpatient treatment - requires 7 to 10 days of stay in the intensive care unit, the sick person is prescribed bed rest and a strict diet;
- assistance from a cardiologist - such a patient is left in the cardiology department for a week or two, such treatment includes taking medications on a schedule and physical therapy;
- rehabilitation itself - falls during the period of scarring (the pathological process can be observed on the ECG from 1 month to six months), during which time the victim visits a sanatorium or is treated at home under the supervision of a local doctor.
By law, people who have suffered a myocardial infarction are granted sick leave for up to 4 months. Recovery times vary depending on the size of the affected area of the myocardium, possible risks, the presence of complications and the age of the individual.
In young people, recovery occurs faster due to a stronger vascular wall and higher elasticity of the coronary arteries. The quality of rehabilitation largely depends on the behavior of the patient himself.
Health indicators affecting the ability to drive a car
A full life involves daily adaptation to various environmental factors. Adaptive capabilities after a myocardial infarction are somewhat reduced. If the victim led an active lifestyle before the attack, a ban on playing sports or driving a car can negatively affect his psychological health. During an objective examination, it is worth assessing not only the activity of the heart, but also the function of other body systems in order to eliminate possible risks.
First aid
Patients with cardiovascular pathologies are at risk of developing thrombosis and thromboembolism during the flight. These situations are complicated by all sorts of unfavorable factors, such as excess weight, hypercholesterolemia, smoking and alcoholism. In the absence of normal blood supply to the most important organs, such as the heart and brain, large-scale death of cells in these organs can begin. How to suspect thromboembolism? This is indicated by the clinical picture. A person feels compression behind the sternum, palpitations, shortness of breath, and general weakness.
If you are planning a trip to the sea, it is better to consult with a specialist in advance about what kind of transport you should use and whether it is worth the risk of boarding a plane. Patients with myocardial infarction can safely go to sea, but at least 6 months must pass from the moment the diagnosis is made. Sea air, of course, has a positive effect on the body, heals and strengthens it. But significant changes in temperature can aggravate certain symptoms. This is why summer vacations are not recommended for patients with myocardial infarction who have only recently suffered one.
Significant heat can adversely affect people with any type of heart disease. It helps increase blood pressure. If after hot weather a person is immersed in cool water, the blood vessels spasm. The result is an attack of angina. That's why, if you have a heart attack, it is better to choose autumn or spring for travel. You can also, as an alternative, resort to traveling to the mountains or visiting sanatoriums located relatively nearby.
Diet after stenting
The diet after stenting includes foods rich in vitamins and fiber, but sharply limits the content of animal fats and the content of quickly digestible carbohydrates.
It is not recommended to eat fatty lamb, beef, pork, butter, lard, mayonnaise and spicy seasonings, sausages, cheese, caviar, pasta from non-durum wheat, chocolate, sweets and baked goods, white bread, coffee, strong tea, alcohol and beer, carbonated sweet drinks.
It is recommended to consume fresh vegetables and fruits, fresh juices, boiled poultry, fish, cereals, durum pasta, cottage cheese, fermented milk products, and green tea.
Prevention of adverse situations
If at least six months have passed since the heart attack, you can fly safely, but a preliminary consultation will still not hurt. To avoid unexpected troubles, you should think through your upcoming trip in detail. You need to contact your doctor and tell him about your plans. He will conduct a comprehensive examination and decide whether to go to the sea, to the mountains or somewhere else, or to postpone the trip for a certain period of time.
It is quite possible that the cardiologist will prescribe special medications that you will need to take before the flight, possibly during the flight and after landing. All this is done in order to control myocardial function and keep blood pressure at a normal level. Nutrition should remain correct, as well as drinking regime. Giving up bad habits is also important. All this together will reduce the risk of complications. A few days before flying, you need to take Corvalol, motherwort, valerian root and other sedatives.
It is important to prevent anxiety syndrome, when a person worries that he will become ill in the salon. To reduce anxiety, you can put Validol under your tongue before boarding a plane. Thanks to this, the takeoff can be postponed with minimal losses.
You also need to pre-assemble a first aid kit for your carry-on luggage. What should I put there? Mandatory components should be, in addition to sedatives, antiplatelet agents. They help thin the blood and create unfavorable conditions for the formation of blood clots. Nitroglycerin should also be put there. It belongs to the category of nitrates and prevents the symptoms of angina pectoris.
Antihypertensives are presented in large quantities on the pharmaceutical market. That is why the modern drug must be selected by a doctor. He is based on his experience and the presence of side effects. An example of such drugs is Captopres. This is a means for accelerated assistance to the heart and blood vessels. Thanks to it, the pressure is reduced quickly. Antiarrhythmic drugs are always included in the first aid kit. One of the best drugs in this group today is Amiodarone. It normalizes heart rhythms.
Heart patients on board an aircraft are often embarrassed to report their deteriorating health to the crew. However, do not be embarrassed, as timely assistance can lead to a further comfortable flight. Long-term travel by air is very inconvenient even for a healthy person, and there is no need to talk about someone who has had a heart attack and suffers from hypertension. Rarely does anyone manage to avoid blood stagnation in the lower extremities. This is explained by the forced position of the body, which is constantly in the same position.
Medications after stenting
After stenting, it is imperative to take medications prescribed by the cardiologist, such as Plavix or Zilt, and aspirin, to prevent blockage of the stented vessels by a blood clot. The treating cardiologist will select the duration of administration and dosage individually.
And also, in the presence of concomitant diseases, for example hypertension - drugs that lower blood pressure, cholesterol-lowering drugs for high cholesterol levels in the blood, and other necessary medications that were taken before heart stenting.
Stenting and airplane flights
Only the attending cardiologist, who has observed the patient from the very beginning, has the right to discuss whether it is possible to fly by plane after a heart attack. It happens that the operation is performed as planned. This means that no complications such as a heart attack have previously occurred. But if stenting and heart attack go hand in hand, then it is necessary to allow enough time for the patient to recover. If he has only recently left the hospital, he is strictly forbidden to fly. If a lot of time has passed since the surgical intervention, a person can easily afford to fly somewhere by plane.
And yet it is important here in travel planning. It is necessary to constantly keep in touch with your treating cardiologist and undergo a special examination. The specialist will also give advice on taking medications before and during the flight. The American Heart Association states that you should not fly if:
- Less than six months have passed since the heart attack, if it was accompanied by complications, and if uncomplicated, less than 2 weeks.
- A person has signs of heart failure that cannot be corrected with pills.
- Complex forms of arrhythmia were discovered.
- Arterial hypertension is difficult to treat with drugs.
- If you have angina with unstable symptoms.
How long do they live after cardiac stenting?
Stenting is carried out in order to restore the patency of the narrowed coronary (coronary) artery, which nourishes the heart, supplies it with oxygen, and thereby return the vital organ to normal functioning.
Stenting in some cases is a modern alternative to open surgery – coronary artery bypass grafting.
Stenting does not cure coronary heart disease, but removes the consequences of this disease. The patient's life expectancy depends on many factors, including concomitant pathology. And also in what specific situation the stenting was performed.
What is the extent of heart damage? But most of all, the duration depends on the patient’s own attitude. If he changes his lifestyle and follows all the doctor’s recommendations and prescriptions, he will live a long and fruitful life, counting in decades.
Coronary angiography of the heart vessels is an X-ray examination of the arterial vessels of the heart using a radiopaque substance, which makes it possible to identify the location, degree and nature of narrowing of the internal lumen of the arteries.
This highly informative diagnostic method is used to clarify the diagnosis of a patient with IHD (coronary heart disease). It allows the doctor to choose the most appropriate treatment strategy (coronary stenting, balloon angioplasty, coronary artery bypass grafting or drug therapy) for this serious disease, which can lead to serious complications.
Types of coronary angiography
Depending on the scope of the study, traditional coronary angiography can be:
- general: examination of all coronary vessels is performed;
- selective: targeted examination of only one or several coronary vessels is performed
Currently, coronary angiography of the arteries of the heart can be performed using a computed tomograph. This technique is called CT coronary angiography or MSCT (multispiral computed tomography of the coronary vessels).
After the administration of a radiocontrast agent, the patient is placed in a multislice computed tomograph. This technique successfully competes with traditional coronary angiography, since it can be performed in a shorter time and does not require hospitalization of the patient.
Each of the above methods has its own indications and has its own disadvantages and advantages; only a doctor will be able to determine the necessary type of examination of the heart vessels.
Coronary angiography of the heart vessels is prescribed in cases where, according to clinical and non-invasive instrumental diagnostics, the patient has a high risk of developing complications of coronary artery disease, or the drug therapy used for atherosclerotic vascular lesions is ineffective.
Indications for prescribing coronary angiography of the heart vessels may include:
- symptoms of coronary artery disease (new or unstable angina);
- identifying signs of myocardial malnutrition or changes of ischemic origin identified on an ECG or Holter ECG monitoring;
- positive tests with physical activity (treadmill test, TES, VEM, stress Echo-CG);
- ineffectiveness of drug therapy for angina pectoris;
- identification of dangerous rhythm disturbances;
- post-infarction angina (the appearance of angina attacks immediately after a myocardial infarction);
- myocardial infarction (the procedure is performed urgently in the first 12 hours of the disease);
- differential diagnosis with heart diseases that are not associated with damage to the coronary vessels;
- asymptomatic course of IHD;
- preparation for open heart surgery;
- preparation for kidney, liver, lung and heart transplantation;
- aortic pathology;
- suspicion of infective endocarditis;
- hypertrophic cardiomyopathy;
- previous chest trauma;
- Kawasaki disease.
There are no absolute contraindications to performing coronary angiography. This diagnostic method can be used to examine patients of any age category, regardless of their general condition. The following diseases and conditions may be relative contraindications:
- increased sensitivity of the patient to drugs for local anesthesia or components of a radiopaque substance (in such cases, they are replaced with drugs to which an allergic reaction is not observed);
- uncontrolled ventricular arrhythmia;
- uncontrolled arterial hypertension;
- low potassium levels in the blood;
- heart failure in the stage of decompensation;
- elevated temperature;
- severe renal failure.
Under the above circumstances, vascular coronary angiography can be performed only after the patient’s condition has been stabilized.
Preparing the patient
When prescribing coronary angiography of the heart vessels, the doctor explains to the patient the essence, purpose and possible side effects or complications of this diagnostic method. Before performing this diagnostic procedure, the patient is prescribed a number of examinations:
- clinical blood test;
- analysis to determine blood group and Rh factor;
- blood chemistry;
- coagulogram;
- blood tests for hepatitis B and C, Wasserman reaction and HIV;
- Twelve-lead ECG;
- Echo-CG;
- If necessary, additional examinations and consultations with doctors of related specialties are prescribed.
The patient must inform the doctor about the presence of allergic reactions to medications, chronic diseases (diabetes mellitus, hypertension, peptic ulcer, stroke or heart attack) and medications constantly taken.
Coronary angiography can be performed on an outpatient or inpatient basis in a cardiac surgery department. The doctor must warn the patient that the study will be carried out on an empty stomach. Before starting the procedure, the puncture site is prepared:
- toilet;
- shaving the wrist, armpit or groin area.
If necessary, before the procedure, the patient must take medications prescribed by the doctor.
When performing coronary angiography, the patient’s condition is monitored by a team of specialists: a cardiac resuscitation specialist and an anesthesiologist. Before puncturing the artery, the surgeon administers local anesthesia. Next, perform the following steps:
- After puncture of the femoral, axillary, brachial or radial artery (the choice of access is determined depending on the available equipment or the doctor’s preferences), a special catheter is inserted into the lumen of the puncture needle using a guide (introducer).
- After installing the catheter and introducer, the puncture needle is removed, and to prevent blood clotting, heparin is administered to the patient and the entire system is washed with a mixture of saline and heparin.
- The catheter, under the control of fluoroscopy or echo-CG, moves through the blood vessels into the upper part of the aorta.
- From this moment, the patient's blood pressure is constantly measured, and the catheter is carefully moved into the common trunk or into one of the branches of the coronary arteries.
- A radiopaque contrast agent is injected into the catheter using a special syringe, which flows through the bloodstream into the coronary vessels and fills them in a few seconds.
- Using a special angiograph apparatus, the results obtained are recorded: pathological changes in the coronary arteries, tortuosity of the chords, areas of stenosis and the reaction to contraction of the heart muscle. When taking pictures, the right and left coronary arteries are visualized.
- The results obtained can be recorded on x-rays or x-ray videotape. Using software, the results are digitized (if necessary, a three-dimensional image of the coronary arteries can be performed). A record of the results is given to the patient in the form of a written report and a record of X-ray images (on disk or film).
After completing the images, the doctor removes the system and stops the bleeding using a sterile pressure bandage, which consists of a napkin pressed with a special device to create pressure on the area of the punctured artery.
The pressure is released 15 minutes after applying the bandage, and after half an hour the device is removed and a regular pressure bandage is applied to the puncture site. The bandage is removed one day after the examination.
If there are certain indications, immediately after completion of the study, the patient may be offered reconstructive endovascular treatment: balloon angioplasty or stenting of the coronary vessels.
When performing coronary angiography through the radial artery, the patient can return home within a few hours after completion of the study. He is advised to follow a gentle regimen and limit the flexion of the upper limb on which the arterial puncture was performed.
After the procedure, to prevent possible disturbances in the functioning of the kidneys, the patient is recommended to drink plenty of fluids. If you experience severe weakness, shortness of breath, decreased blood pressure, severe pain or swelling in the puncture area, you should immediately consult a doctor.
With other types of access, the patient is under medical supervision for 24 hours and is kept in bed.
Complications
Coronary angiography, if all the rules for its implementation and the doctor’s recommendations are followed, is quite rarely complicated. The most common complications are:
- bleeding at the site of arterial puncture (approximately 0.1% of patients);
- formation of hematoma, edema or false aneurysm in the area of the punctured artery;
- development of arrhythmias;
- thrombosis of coronary vessels;
- allergic reaction to a radiopaque substance (it contains iodine);
- vasovagal reactions: paleness, cold sweat, decreased blood pressure, decreased pulse.
Severe complications of coronary angiography develop extremely rarely. They can become:
- myocardial infarction;
- cerebral ischemia;
- stroke;
- damage or rupture of the vessel through which the catheter is inserted;
- death (less than 0.1% of cases).
The maximum risk of complications can be observed in the following cases:
- childhood;
- patients over 65 years of age;
- stenosis of the left coronary artery;
- left ventricular failure with ejection fractions less than 35%;
- valvular heart disease;
- severe forms of chronic diseases (diabetes mellitus, tuberculosis, renal failure, etc.).
Angina attack: signs, emergency care
Life that goes on as usual after a myocardial infarction changes dramatically: old habits and hobbies often have to be forgotten, because they can become an unfavorable factor for a repeated attack of the disease.
An attack of angina can be considered a pre-infarction condition, and that is why help for severe heart pain should be provided immediately and correctly. Coordinated actions in such situations can significantly alleviate the patient’s condition and prevent the development of severe complications. In everyday life, everyone may encounter a situation where a loved one, neighbor, colleague, or just a stranger on the street needs emergency help. In this case, it is extremely important to know what signs to recognize an angina attack and how to alleviate the patient’s condition.
Cardialgia (pain) with angina pectoris develops against the background of a lack of oxygen in the myocardium, provoked by ischemia (i.e., the flow of insufficient blood to the muscle fibers due to narrowing of the coronary vessels). Oxygen deficiency in the heart muscle is especially noticeable during physical and psycho-emotional stress, because...
Signs of an angina attack are few in number, but quite characteristic and in most cases they are rarely confused with other diseases. The main symptom of this condition is sudden pain behind the sternum or to the left of the sternum, which appears after physical or psycho-emotional stress, hypothermia, and sometimes at rest.
Cardialgia is of a pressing or burning nature, and in most patients its irradiation (reflection) is observed in the left half of the body (arm, shoulder blade, stomach area, throat, cervical vertebrae, lower jaw). Sometimes the pain may radiate to the right arm. In the lying position, cardialgia intensifies.
Patients describe the nature of pain during an angina attack in different ways:
- compressive;
- pressing;
- burning;
- sharp.
The duration of pain is about 5 minutes (less often about 15-20). As a rule, after eliminating the cause that provokes it (physical activity, cold, stress), it can go away on its own or disappears within 2-3 minutes after taking a Nitroglycerin tablet.
Cardialgia with angina pectoris is often accompanied by noticeable anxiety of the patient or fear of death. During an attack of angina, the patient may experience:
- nausea and vomiting;
- pallor;
- sweating;
- dizziness;
- burping or heartburn;
- difficulty breathing or shortness of breath;
- palpitations and increased heart rate;
- rise in blood pressure;
- numbness and coldness of the extremities.
In some cases, an attack of angina occurs atypically or is not accompanied by cardialgia. These types of this disease make their recognition much more difficult.
In some patients, pain in the heart is completely absent and is felt only in the areas of its typical irradiation:
- in the shoulder blades (right or left);
- in the IV and V fingers of the left hand;
- in the left or right hand;
- in the cervical vertebrae;
- in the lower jaw;
- in the teeth;
- in the larynx or pharynx;
- in the ear;
- in the area of the upper abdomen.
In some patients, an attack of angina begins with numbness of the fourth and fifth fingers of the left hand and severe muscle weakness of the upper limb. After some time, they develop cardialgia and other signs of angina.
Patients often describe an angina attack as shortness of breath that severely limits physical activity and occurs during inhalation and exhalation. This condition may be accompanied by a cough, which gets worse when trying to move.
In some patients, an angina attack may occur in a collaptoid manner. With this course, the patient’s blood pressure sharply decreases, dizziness, nausea and severe weakness appear.
An attack of angina pectoris can make itself felt by episodes of arrhythmia, which occurs at the peak of physical activity. Such arrhythmias can be stopped by taking Nitroglycerin.
In rare cases, an angina attack is not accompanied by pain. In such cases, myocardial ischemia manifests itself as severe weakness or shortness of breath, which is caused by low contractility of the heart or incomplete relaxation of the myocardium.
All atypical forms of angina are more often observed in patients with diabetes mellitus, heart failure, after myocardial infarction or in elderly patients. The symptoms accompanying such forms of myocardial ischemia are eliminated after cessation of physical or emotional stress and taking Nitroglycerin.
First aid
Most often, pain in the environment with angina appears during walking or other physical activity. In such cases, the patient should immediately stop moving and take a comfortable sitting position. If cardialgia occurs during sleep, you need to sit up in bed and lower your legs down.
During an attack of angina, it is prohibited to stand on your feet, walk, or perform any activities involving physical exertion. The patient needs to ensure a flow of fresh air, remove clothing that restricts breathing, and ensure the most comfortable temperature conditions.
A person experiencing cardialgia needs to take a Nitroglycerin or Nitrolingvala tablet under the tongue. Also, to eliminate an attack of angina, medications in the form of sprays can be used: Isoket or Nitrominate. They are injected under the tongue, and one injection constitutes one dose of the drug. After taking these nitrate drugs, the patient can be asked to take one crushed Aspirin tablet, and in the presence of signs of emotional arousal, Corvalol or Valocardin.
It is recommended to call an ambulance during an angina attack in the following situations:
- angina attack occurred for the first time;
- the nature of the attack has changed (it has become longer, the pain is more intense, shortness of breath, vomiting, etc. have appeared);
- cardialgia was not eliminated by taking Nitroglycerin tablets;
- the pain in the heart intensifies.
To more quickly relieve an attack of angina after taking the drugs described above, it is recommended to perform a light massage (or self-massage) of the face, neck, back of the head, shoulders, wrists, left half of the chest and knee joints. Such actions will allow the patient to relax and eliminate tension.
Often an attack of angina is accompanied by a severe headache. To eliminate it, the patient can take a tablet of a non-narcotic analgesic (Baralgin, Spazmalgon, Analgin, Sedalgin).
After such activities, it is necessary to count the pulse and measure blood pressure. With severe tachycardia (more than 110 beats per minute), the patient needs to take 1-2 tablets of Anaprilin, and with a pronounced increase in blood pressure - 1 tablet of Clonidine (under the tongue).
Pain in the heart after taking Nitroglycerin or other nitrate drugs should be eliminated within 2-3 minutes; if there is no such effect, the patient must repeat taking one of the drugs. During one attack, the patient can be given no more than three tablets of Nitroglycerin and Nitrolingvala or no more than three injections of Isoket or Nitrominate.
Usually, after the measures taken, the angina attack disappears within 2-5 (less often 10) minutes. If cardialgia is present within 15 minutes after taking Nitroglycerin, it is necessary to urgently call an ambulance, since this condition of the patient can lead to the development of myocardial infarction.
If an attack of angina pectoris was eliminated on its own, the patient is advised to limit any physical or emotional stress, maintain bed rest and call a doctor.
The patient or his relatives should be aware that if signs of low blood pressure are detected (with collaptoid angina), taking drugs from the group of organic nitrates (Nitroglycerin, Isoket, etc.) is contraindicated. The following signs may indicate hypotension:
- the patient experiences severe weakness;
- dizziness;
- pallor;
- cold sweat.
In such cases, the sequence of actions should be as follows:
- Lay the patient down.
- Call an ambulance.
- Give him a crushed Aspirin tablet.
- To reduce pain, you can use tablet analgesics (Baralgin, Sedalgin, etc.).
We suggest you read: Green tea increases or decreases blood pressure
Emergency care for a prolonged attack of angina can only be provided by a doctor.
If necessary, Nitroglycerin is taken again (1-2 tablets under the tongue), followed by intravenous jet administration of non-narcotic analgesics (Baralgin, Maksigan, Analgin) with 50 ml of a 5% glucose solution. To enhance the analgesic effect and provide a sedative effect, antihistamines (Pipolfen, Diphenhydramine) or tranquilizers (Seduxen, Relanium) can be used.
In the absence of pain relief, the patient is administered narcotic analgesics (Promedol, Morphine hydrochloride, Omnopon) in combination with Droperidol or a tranquilizer. Also, neuroleptanalgesia (intravenous administration of Thalomonal or a mixture of Fentanyl and Droperidol) can be used to eliminate pain in the heart.
With a pronounced decrease in blood pressure, which often occurs after taking drugs from the group of organic nitrates (Nitroglycerin, Isoket, etc.), the patient is administered a solution of Poliglyukin (intravenously, 50-60 drops per minute). If there is no effect, administration of 0.2 ml of a 1% Mezaton solution may be recommended.
When stopping an attack of angina pectoris, which occurs against the background of a persistent rise in blood pressure, antihypertensive and vasodilator drugs (Dibazol, Papaverine, Platiphylline, etc.) can be used.
After stabilizing the condition of a patient who has suffered an attack of angina, he is recommended to undergo a dynamic electrocardiographic examination and a number of other diagnostic procedures. Based on the data obtained, the doctor will be able to prescribe further treatment for coronary heart disease.
How to help with an angina attack. Cardiologist V. A. Abduvalieva tells