If a child has a viral disease, the level of monocytes in the blood increases. Let's look at what to do in this case.
We come across varieties of leukocytes when undergoing medical tests. For the full functioning of the immune system, the level of monocytes plays an important role. Due to certain abnormalities in the child’s body, monocytes can be either overestimated or underestimated.
Let's consider in what cases monocytes in a child's blood are elevated and what measures parents need to take.
The role of monocytes in a child’s body
Mononuclear cell of the leukocyte series - monocyte
Monocytes are one of the most active participants in the immune system in the body of both adults and children. Being mononuclear subtypes of leukocytes, they help the body fight viruses and bacteria, and also eliminate dying cells in the process of natural tissue renewal. They are larger in size than other protein compounds of the immune system and are capable of destroying the largest particles of pathogenic material.
Functions in the child's body:
- detection of harmful substances;
- notifying other cells about the penetration of foreign elements;
- absorption of destructive cells;
- cleansing the site of origin of the pathogenic factor;
- assistance in the restoration of damaged tissues;
- liberation of the body from dead cells;
- storing information for the subsequent production of antibodies.
Cell functions
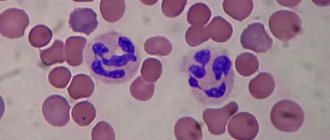
Blood contains many types of cells that perform different functions, from transporting oxygen to producing antibodies. Blood cells can be divided into red and white - lymphocytes and erythrocytes. Red blood cells make up the bulk of cells circulating in the blood and carry oxygen. White blood cells fight infection and digest the remains of destroyed cells.
Leukocytes are divided into 3 main groups: granulocytes, monocytes and lymphocytes. Immunity can be compared to an army. Monocytes in it will play the role of “heavy artillery”, neutrophils - “private soldiers”, lymphocytes can be called “officers”.
What are lymphocytes
Lymphocytes are an important category of blood cells for the immune system because they can repeatedly fight harmful microorganisms, providing reliable protection to the body.
Lymphocytes and monocytes live longer than other blood cells—sometimes even several years. Their destruction occurs in the spleen. The function of lymphocytes depends on their specialization.
Lymphocytes are divided into several categories:
- T cells. They make up 75%. T cell receptors recognize protein antigens.
- B cells - 15%.
- NK cells. Their share is 10%.
Each category has its own purpose.
What are monocytes
Monocytes are white blood cells that are involved in fighting infections. They absorb and destroy various microorganisms. When they leave the blood, they turn into macrophages, which fight infections and dispose of dead cells. Monocytes are able to move quickly and freely penetrate the walls of capillaries, entering the intercellular space. There they catch harmful microorganisms and neutralize them.
Important information: What is MPV or mean platelet volume (blood test interpretation)
These are active cells. They are formed in the bone marrow. These cells do what is impossible for other white blood cells - they eliminate microorganisms even in a highly acidic environment.
The norm of monocytes in the blood of children
Normal values in children differ from those in adults
Depending on the age of the child, reference values change. Newborns have more monocytes in the blood, since the immune system is just being formed, and the body is ready to repel any infection. Gradually, the activity of immune cells decreases; by the age of 16, their level becomes the same as in adults.
When calculating the level of monocyte circulation in the blood, several values are used. The first is the specific gravity in the total number of all cells of the immune system, the second is the number of monocyte units in 1 liter of blood.
| Child's age | Specific Gravity (%) |
| 1 day | 3-12 |
| 1 Week | 4-15 |
| 1 month | 4-12 |
| 6 months | 4-11 |
| 1 year | 3-10 |
| 6 years | 3-9 |
| 10 years | 2-9 |
| 16 years | 1-8 |
Reference values for the total number of monocyte units in the blood:
- children under 16 years old - 0.05 - 1.1 *10 9/l.
How to normalize monocyte levels
Monocytosis and monocytopenia cannot be cured, because these are not independent diseases, but only the body’s reaction to other pathologies. To normalize the level of monocytes in the blood, it is necessary to establish the root cause of their imbalance. When the primary disease is defeated, the level of monocytes in the blood will automatically recover. But this does not mean that the quantitative and qualitative composition of blood should not be controlled. On the contrary, a general blood test should be taken at least once a year.
In addition, do not forget about basic preventive measures to ensure that the level of various blood cells in a child is close to normal:
- watch what he eats - improper and unbalanced nutrition will definitely affect his overall health;
- from early childhood, accustom your child to the fact that for health you need to drink plain water throughout the day;
- strengthen children's immunity - reasonable hardening, regular physical exercise should become the best helpers in the development of a healthy body;
- do not overload the child either physically, mentally, or psychologically - all stress should alternate with rest.
And the most important thing is to regularly take tests and visit a pediatrician, so that if a problem arises, you do not allow it to develop.
Date: 07/22/2016.
What is monocytosis
The monocyte “protects” the body by absorbing foreign agents
The onset of inflammatory phenomena in the body provokes an increase in the activity of monocytes. Monocytosis is an increased circulation of monocytes in the plasma. This term is not a disease, but its consequence.
Monocytosis means that there is a focus of infection in the child’s body, to which monocytes rush to destroy harmful elements. An increase in indicators above the norm is a reflection of the child’s body’s natural defense against infection. To effectively fight a pathogenic element, the immune system needs a larger number of monocytes. In diagnostics, it is a marker indicating the presence of a pathogenic factor.
Types of monocytosis in children
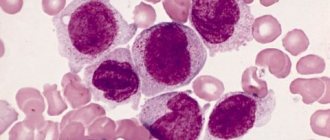
Monocytosis is divided into absolute and relative. Absolute indicates a high number of monocytes per liter of blood. Its value is determined by the level of the inflammatory process in the child’s body. With an absolute excess of monocytes, the indicators of other cells of the body’s defense system also increase.
Relative monocytosis demonstrates an increase in the number of monocytes among all immune cells. At the same time, the absolute level may remain within the normal range. Most often, a relative excess indicates the presence of diseases in the past period or suffered moral shocks.
What monocyte parameters are elevated in children?
The newborn body especially needs a strong immune system
The importance of immune cell content varies as the child grows older. The older the child, the fewer monocyte units should be present in the bloodstream. Only in the first weeks of life do the indicators increase, since the baby’s body is just getting acquainted with the millions of bacteria that live in our environment.
Values exceeding the norm (in%):
- 1 day - > 12;
- from 1 week - > 15;
- from 1 month - > 12;
- from 6 months - > 11;
- from 1 year - > 10;
- from 6 years - > 9;
- from 16 years old - > 8.
High absolute level values for a child under 16 years of age: > 1.1 *10 9/l.
Possible symptoms
Monocytosis (that is, monocytes are increased in a child) has no external manifestation. The nature of the symptoms will depend on what exactly led to the development of such a symptom.
The collective symptomatic complex may include the following conditions:
- moodiness, constant crying;
- poor appetite - the child may refuse food altogether;
- cough for more than two weeks;
- enlarged lymph nodes;
- skin rashes;
- low-grade or high body temperature, against which chills and fever will also be present;
- digestive system disorder;
- frequent urination or, conversely, anuria (the baby may cry when the bladder is emptied);
- abdominal pain;
- pale skin;
- unstable blood pressure.
Due to the fact that a newborn baby will not be able to tell what exactly is bothering him, if some of the symptoms described above are present, you should immediately contact your pediatrician for advice.
Symptoms and signs of elevated monocytes in children
A lethargic and capricious child is a cause for concern
Symptoms directly depend on the disease that caused monocytosis. In children, excess circulation of immune cells may be accompanied by symptoms:
- fatigue, drowsiness;
- irritability;
- sudden change of mood;
- temperature increase;
- decreased appetite;
- bowel dysfunction;
- nasal congestion;
- complaints of headache;
- enlarged lymph nodes;
- the presence of a rash.
Causes of monocytosis in a child
Parasitic infestations can cause monocytosis in a child
A doctor cannot make a diagnosis based solely on the presence of monocytosis. Additional examinations will be required to identify the cause of increased cell activity.
Small fluctuations are not necessarily accompanied by disease. A slight increase may be caused by injury, teething, the use of certain medications, or as a consequence of a previous illness. Indicators much higher than normal indicate the presence of pathogenic factors.
Causes:
- ARVI,
- flu,
- Infectious mononucleosis,
- parasitic infection,
- diseases of the circulatory system,
- bacterial infection
- autoimmune diseases,
- tuberculosis,
- systemic connective tissue diseases,
- recovery after an acute inflammatory process.
Possible consequences
An increased number of monocytes can accompany many diseases, so it is impossible to indicate certain complications in this case. Timely consultation with a doctor and identification of the cause of changes in the blood formula in most cases allows you to quickly cope with the disease without consequences.
Delaying diagnosis, self-medication or incorrect selection of medications can lead to complications of the underlying disease and its transition to a chronic course. In such cases, complete recovery will require 2 times more time and effort.
Diagnosis of monocytes in children
Taking blood from the heel of a newborn
An analysis for the content of monocytes is carried out in the first days of a child’s life, in the maternity hospital. Blood for diagnosis in newborns is taken from the heel. The result not only reflects the state of the hematopoietic system, but also allows you to determine whether the baby can be vaccinated at this stage.
For older children, blood is taken from a finger to determine the number of monocytes. The results of the study indicate the possible occurrence of inflammatory processes, the presence of chronic forms of diseases, and the effectiveness of previously prescribed treatment.
If the analysis indicates the presence of monocytosis, the pediatrician will issue a referral to continue the examination. Suspicion of the presence of helminths requires an additional coprogram. Any infectious disease is a reason to visit an infectious disease specialist. To identify a bacterial infection, the patient is sent to undergo a bacterial culture test.
How is the level of monocytes determined?
The monocyte level is calculated based on a complete clinical blood test. It is an indicator for the presence of most bacterial, viral and fungal infections, which may not manifest themselves for a long period of time. It is the indicator of monocyte activity that will indicate their presence.
The number of monocytes is determined in their percentage and absolute content in the blood.
MONO% or MON% (monocytes) - relative content; MONO# or MON# (monocytes) - absolute quantity.
An increase or decrease in the content of mononuclear cells is considered not as a separate factor, but in conjunction with other changes in the leukocyte formula. For example, monocytosis against the background of an increase in eosinophils indicates that an allergic reaction is occurring in the body or that parasites are present (giardiasis, asthma, dermatitis). A simultaneous increase in monocytes and neutrophils indicates that the child is infected with bacteria or fungi.
Preparing for a general blood test
The young patient must be prepared for the test
A reliable picture of the content of immune elements in the bloodstream depends on proper preparation for the test.
- The day before going to the laboratory, it is necessary to limit the child’s consumption of fatty and spicy foods.
- Do not allow your body to be overloaded with physical activity.
- The baby's emotional state should be normal.
- The test is taken in the morning on an empty stomach. Only ordinary clean water is allowed.
- Avoid taking medications. If this is not possible, provide your doctor with a complete list of medications, including vitamins.
- It is recommended to take tests in newborns between feedings.
What can affect the reliability of the results?
Results that deviate significantly from the norm serve as a prerequisite for retaking the analysis. An error can creep into the indicators if the preparation went wrong.
- If the child was very worried before the blood was removed.
- If the clinical analysis is carried out urgently, not in the morning. The number of immune cells varies depending on the time of day.
- Overdose of vitamins.
- Taking certain medications. For example, phosphorus-containing drugs produce an increase in the level of monocytes.
Treatment of monocytosis in a child
In case of monocytosis, the child should be examined by a doctor
There are no medications that reduce the level of monocytes and cannot be. Immune cells do not increase without reason. If their number has increased, the child’s body needs it at the moment. The main thing is to find out the reason for the increase in activity and eliminate it.
If the prerequisite for monocytosis is a bacterial infection, the child will be prescribed a course of antibiotics. If the cause is a viral infection, the doctor will write a prescription for antiviral drugs. The addition of helminths to the microflora is a common cause of monocyte growth in children. Vitamin complexes and antihistamines are used. The highest rates of monocytes are in infectious mononucleosis (infection with the Epstein-Barr virus). Treatment with ibuprofen, vitamin therapy and immunomodulatory drugs is prescribed.
Most pathologies that cause monocytosis require a special diet. It is also recommended that the child spend more time at rest. In severe cases, the small patient will need to be admitted to a hospital.
Threat due to elevated monocytes in children
Missed monocytosis - risk of complications
If the analysis reveals an increase in monocytes, this may be a consequence of a previous illness. During the recovery period, mononuclear leukocytes continue to work to cleanse the child’s body. The doctor will prescribe a retest, which will indicate a gradual decrease in monocytes.
Increased levels of immune system elements over a long period are a sign that pathogenic processes are continuing. The causes of monocytosis in children should be treated without fail. Complications in a child’s body develop quickly and can lead to severe forms of illness.
Often, viral diseases against the background of an increase in monocytes can develop into pneumonia, otitis media, croup, and sinusitis. Damage to the liver or kidneys is the reason for untimely treatment of a number of diseases.
How to determine the indicator
To determine the numerical indicator of monocytes, a thorough blood test will be required. There are several recommendations:
- In most cases, blood is donated from a finger. Sometimes blood can be taken from a vein, but this procedure is used extremely rarely.
- The day before the test, the child should not be given medications for the underlying disease (if any). Otherwise, the result may not be accurate. If stopping the medication is not possible, you should notify the nurse before donating blood.
- Blood sampling for laboratory testing is carried out in the morning. This must be done on an empty stomach. In the morning, the child can be given a small amount of water about an hour before the procedure. If the analysis is performed on a child under one year old, then at least 2 hours must pass after feeding, otherwise the results can be considered inaccurate.
- The indicators are affected by the person’s condition, so parents should try to calm the child down. You can engage in conversation on an abstract topic.
- On the test form, it is necessary to indicate the patient’s age, since in childhood the norm of monocytes is different. For example, for children aged 3 and 11 years, the indicators will vary.
- The day before the scheduled manipulation, fatty foods are excluded from the children's diet. This is explained by the fact that such food can influence the quantitative indicator of blood composition.
After the standard blood sampling procedure, a laboratory test is performed to calculate the leukocyte formula. This determines the quantitative ratio of monocytes to other types of white blood cells. Red blood cell counts are also taken into account. In other words, elevated monocytes in a child are considered not as an independent indicator, but taking into account the general blood count.
Prevention
Walks in the open air
For the first time, the child's immune system encounters millions of harmful particles. Helping immune cells resist attack from pathogenic microorganisms can be done through preventative measures.
- Sufficient time for rest.
- Walks in the open air.
- Optimizing your diet.
- Develop the habit of washing hands and brushing teeth in your child.
- Positive emotional background.
The development of antibodies to all kinds of harmful substances occurs precisely in childhood. This process is often accompanied by inflammatory processes. This is a natural phenomenon and you should not be afraid of it. The main thing is to help the child’s body cope with the attack of viruses and bacteria through prevention and timely treatment.