The essence of pathology
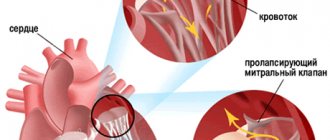
The mitral valve is located on the border between the left atrium and the ventricle.
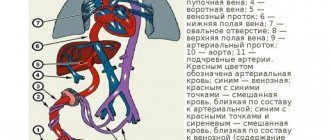
The valve consists of two leaflets, which are attached to the cavity of the left atrium and the ventricle with the help of chords. In the absence of pathology, during the diastole phase, the halves of the mitral valve sag freely downward. Thanks to this, the blood flow has no obstacles to move from the left atrium to the LV.
With the onset of the systole phase, the halves of the mitral valve rise, thereby blocking the free flow of blood, tightly closing the hole between the atrium and the ventricle.
With the development of mitral heart disease, structural and functional changes in the MV occur. As a result of this, the valves sag into the left cavity, which leads to the formation of a lumen between them.
It is through this lumen that blood has the opportunity to return from the left ventricle to the atrium. This process is called regurgitation.
Mitral regurgitation in the initial stage of its development leads to pulmonary or arterial hypertension.
Clinical picture
Rheumatic mitral stenosis is usually diagnosed in women. Mostly, patients consult a doctor with the following complaints:
- shortness of breath (accompanying physical activity of increased intensity);
- chest pain;
- sometimes – rapid heartbeat.
Shortness of breath is a consequence of increased pulmonary congestion against the background of increased release of blood into the pulmonary circle with increased physical activity. Often this symptom is supplemented by a cough (manifests itself while walking), as well as tachycardia (rapid heartbeat); when listening, an altered tone of the mitral valve opening is determined.
Combined mitral disease leaves its mark on the patients' complexion - it acquires a yellowish-pale tint, the lips become bluish. Patients with MPS look asthenic, often with features of physical infantilism. In some cases, the course of the disease is accompanied by a characteristic bright red blush on the cheeks - a consequence of the synthesis of histamine-like substances by the liver.
Valve insufficiency is extremely rarely an independent disease - it is, rather, an intermediate stage in the development of mitral and aortic heart defects (combined). After this, as a rule, stenosis occurs.
Important: with combined defects, serious disorders of the heart are diagnosed, they are extremely difficult, and in most clinical cases they cause rapid decompensation.
Causes
MVP is not an independent disease. Experts consider it a clinical-anatomical syndrome that runs parallel to other diseases.
Among the reasons that cause the development of this pathology are the following:
- Ehlers-Danlos syndrome;
- Marfan syndrome;
- congenital arachnodactyly;
- osteogenesis imperfecta;
- rubella;
- lupus;
- myocarditis;
- cardiac ischemia;
- heart attack;
- myocarditis;
- HRBS;
- hyperthyroidism;
- rheumatism;
- chest injury, etc.
If a person falls into a risk group, it is necessary to immediately undergo a comprehensive examination by specialists. This is necessary in order to avoid the development of a complex stage of pathology.
Classification
In modern medicine, mitral defects are classified according to factors such as their etiology, localization and degree of manifestation.
Based on etiology, the following types of MVP are distinguished:
- Primary. The reasons for its development are congenital disorders of the structure or functioning of the mitral valve leaflets. These processes lead to thickening of the walls of the valves, which leads to a loss of their elasticity. In rare cases, disorders may extend to the fibrous ring or chordae.
- Secondary. This type of defect develops due to the fact that a person has suffered from certain diseases, in some cases chronic (vegetative-vascular dystonia, coronary heart disease, infectious diseases, etc.). In this case, the dominance of the sympathetic tone over the parasympathetic tone occurs, which leads to an increase in the amplitude of heart contraction, disruption of the contractile function of the ventricles of the heart, and the development of tachycardia.
Based on location, mitral valve defects are divided into prolapse of the posterior, anterior, or both walls of the mitral valve.
Based on the results of the echocardiogram, data on the degree of manifestation of the defect is obtained. According to these data, the following degrees of prolapse are distinguished:
- I degree – in which the halves of the mitral valve bend by 3–6 mm;
- II degree – the level of prolapse of the valve leaflets ranges from 6–9 mm;
- III degree - at this stage of the defect, the halves of the MV sag by more than 9 mm.
Separately, I would like to highlight combined mitral disease, which is simultaneously accompanied by a narrowing of the opening between the LA and LV, as well as mitral valve insufficiency.
This type of MVP is quite widespread and occurs in approximately 50% of all patients.
As mentioned earlier, the mitral heart is accompanied by a process such as regurgitation. Based on the volume of reverse blood flow, the pathology is divided into three degrees:
- 1st degree - the process of regurgitation occurs only at the level of the halves of the mitral valve;
- 2nd degree – the level of regurgitation reaches half of the left atrium;
- 3rd degree - the wave of reverse blood flow reaches the opposite apex of the atrium.
The choice of the most effective treatment method depends on how accurately the type and degree of mitral valve disease is determined.
General understanding of heart valve defects
Aortic valve stenosis
Heart valve defects are congenital or acquired defects of the valve apparatus, leading to its dysfunction. Acquired defects are much more common, and the left half of the heart is mainly affected, so defects such as tricuspid valve stenosis are quite rare. Changes in the structure of the valves or underlying structures that regulate their function lead to hemodynamic disturbances.
Acquired heart valve defects predispose to the development of the disease - infective endocarditis, arrhythmias and conduction disturbances and, ultimately, to heart failure. Heart valve defects can be divided into two groups: insufficiency and stenosis.
Valve insufficiency is a condition in which the valves do not sit close together when they close, causing blood to flow backwards.
Stenosis is a condition in which there is a narrowing of the opening blocked by the valve, which entails a decrease in the incoming blood volume.
Cases where insufficiency and stenosis affect one valve are usually called the development of a combined defect. When two or more valves are affected - combined.
Symptoms
As a rule, stage I mitral valve disease occurs without any symptoms. It can only be detected by undergoing a comprehensive medical examination.
As for other cases, patients complain of the following symptoms:
- weakness;
- fast fatiguability;
- short-term headaches;
- dizziness;
- fainting conditions;
- attacks of suffocation;
- pain in the sternum;
- strong heartbeat;
- rheumatic pains;
- feeling of suffocation, etc.
Among the most common symptoms, most patients note pain in the heart area, which has varying degrees of duration and intensity. As a rule, these pains become more severe with increasing physical activity.
As for children, primary mitral valve disease is often accompanied by the development of inguinal or umbilical hernias, dysplasia of the hip joints, scoliosis, flat feet, and uneven development of body parts. All these symptoms indicate that the child has MVP.
If one or more symptoms are detected, it is recommended not to waste time and undergo a medical examination.
Diagnostic methods and principles of treatment of mitral valves
When examining a patient with mitral valve damage, the doctor performs auscultation. At the same time, he pays attention to the specific auscultatory noise in the heart area. Heart murmur, as a symptom of its damage, is an indication for a comprehensive examination. If mitral valve disease is suspected, the following is performed:
- ECG;
- chest x-ray;
- echocardioscopy;
- consultation with specialized specialists (cardiac surgeon, cardiologist).
Other studies may also be prescribed depending on the degree of valve damage and the presence of other diseases in the patient.
If a defect is detected - mitral regurgitation or stenosis, at the stage of minimal changes, conservative therapy and dynamic monitoring of the patient's condition are prescribed. Drug treatment must be combined with surgical treatment. Therapy uses antiarrhythmic drugs, anticoagulants (to prevent thromboembolic complications), as well as drugs that help eliminate the root cause of the disease.
Isolated and combined mitral heart defects always require surgery - the only question is when. Indications for surgical treatment are:
- signs of heart failure of functional class III – IV, which developed against the background of the defect;
- 2 – 3 stage of regurgitation;
- severe sclerosis, deformation of the valve leaflets;
- ineffective treatment of rheumatic carditis, infective endocarditis.
Among the options for surgical interventions are valve-sparing (comisorotomy for stenosis, comessuroplasty for insufficiency) and valve replacement.
After surgical treatment, the affected valve is sent to the pathological department for examination. In case of insufficiency, the macropreparation contains foci of fibrosis and proliferation of vegetations; in case of stenosis – fibrosis and thickening of the walls of the mitral ring.
For mild mitral valve prolapse, no treatment is required; for severe valve prolapse, beta-blockers are prescribed. These patients undergo annual examination with mandatory cardiac ultrasound.
Diagnostics
Diagnosis of mitral valve disease is quite difficult. One of the difficulties is that stage 1 mitral valve disease occurs without obvious symptoms. Therefore, a medical examination will be required.
Pathology can be detected using a number of methods:
- Electrocardiogram. This is one of the most commonly used methods for diagnosing the disease. Based on its results, it is possible to determine various types of disturbances in the functioning of the heart, which manifest themselves in extrasystole of the ventricles of the heart, paroxysmal tachycardia, bradyarrhythmia, and disruption of the atrioventricular conduction process. As for children, specialists can observe signs of sinus tachycardia in them.
- Using a cardiovisor. This method allows you to determine dysfunctions of the heart muscle, which cannot be detected through an electrocardiogram. This makes it possible to identify symptoms of pathology in the early stages.
- Phonocardiography. The use of this method makes it possible to determine the late or mid-systolic click, which is adjacent to the 2nd tone.
- Echocardiogram. This technique allows you to diagnose the disease in the initial stage of its development. Its use makes it possible to obtain an image of the heart and its valves in a two-dimensional image, in which specialists can see the presence of thickening of the walls of the mitral valve leaflets, an increase in the size of the left ventricle or atrium, prolapse of the halves of the mitral valve, an increase in the diameter of the fibrous ring or the length of the tendon filaments, an aneurysm at the interatrial septum.
- Radiography. During this method, the image shows a bulging of the pulmonary artery arch and a reduced size of the heart. This method is especially often used to diagnose combined type mitral valve disease.
Only a comprehensive medical examination using several methods gives the clearest picture of the mitral heart.