Pathomorphology of alcoholic cardiomyopathy
The pathological picture of the disease is quite characteristic, although it has many similarities with other types of cardiopathy.
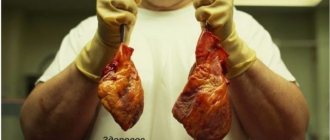
At autopsy, the heart is usually enlarged, hypertrophy of the walls is observed, the cavities are expanded, often due to the right ventricle. The weight of the organ can reach 600g.
Fatty degeneration and interstitial edema are usually present. Wall thrombi can be found in the chambers. The myocardium is flabby, clay-colored, with small scars. Coronary arteries are unchanged in most cases. On microscopic examination, the myocytes are enlarged, and there is a lot of nonfunctional connective tissue between them. There are signs of edema and fatty degeneration.
In the photo you can see a photo of the heart of a patient with alcoholism:
Alcohol and atherosclerotic heart disease
Considering the pathological effects of alcohol on the microvasculature described above, changes in capillary walls, and electrolyte imbalance, it becomes obvious that atherosclerotic heart diseases (coronary artery disease, angina pectoris, ischemia, heart attacks) are more common in patients who drink alcohol excessively. It should also be noted that these heart diseases are much more severe. Alcohol often provokes complications of coronary artery disease (necrosis, or death of the heart muscle).
Forms of the disease and symptoms
Depending on the prevailing clinical manifestation, there are three types of pathological deviation.
Classic or true variety
Most common among patients suffering from alcoholism. Characterized by a vivid picture, recovery is carried out in a hospital.
An approximate list of signs:
- Severe paroxysmal pain in the heart. Burning, pulling, pressing. Observed regularly. The duration of each episode is from 2 to 20 minutes, accompanied by other symptoms. The next moment may come a few days after drinking a large amount of alcohol. A paradoxical reaction is also typical: if the patient does not drink for 2-3 days, the condition worsens. Increased manifestations are observed at night.
- Dyspnea. With little physical activity, and after some time in a state of complete rest. There is a disturbance in gas exchange, which affects all organs and systems.
- Panic attack. At the time of the next attack, the patient may feel strong fear for life. Motor agitation increases, the person rushes about, unable to find peace. It may be dangerous.
- Arrhythmia. Of minor nature. A clinically common variant is sinus tachycardia. Over time, it may degenerate into another, more complicated form (see below).
Pseudo-ischemic type
It disguises itself as classic ischemic heart disease, but has a longer duration of attacks. Development is determined by taking the next dose of alcohol. A spontaneous course is possible, unrelated to alcohol consumption.
An approximate list of symptoms:
- Severe, prolonged pain in cardiac structures. Chest pressure lasts from several minutes to hours. Discomfort increases with physical activity. Tolerance to mechanical activity drops significantly.
- Edema of the lower extremities. As a result of the formation of persistent heart failure. Celebrated in the morning, a relapse occurs in the evening, which distinguishes the process from the renal one. The face is also enlarged, which is quite typical.
- Arrhythmia. In the form of sinus tachycardia, just like last time.
- Shortness of breath is more intense and occurs at complete rest, even in a lying position.
- Dilatation (stretching) of the heart is noted, in the later stages to significant sizes.
Recovery is carried out conservatively, the operation does not make sense. In extreme cases, transplantation is indicated, but this is a special measure. A patient with indications for a transplant may not live to see treatment.
Arrhythmic form
The most formidable and aggressive in terms of speed of development and likelihood of death.
Despite the fact that organic defects form in a relatively late period (1-3 years from the onset of the deviation), formidable symptoms arise:
- Combined arrhythmia. A combination of acceleration or deceleration of contraction frequency and fibrillation, group extrasystole and other phenomena is possible. The probability of stopping the work of a muscular organ is about 60% without treatment, over the course of one or several years.
- Dyspnea.
- Chest pain.
- Heaviness in the legs, varicose veins.
- Weakness, drowsiness, tertiary mental disorders.
- Decreased performance.
- Dizziness.
- Cephalgia (headache) and other manifestations.
Additional possible points:
- Hyperemia of the facial skin. The patient turns red, coughs, hiccups, or has difficulty breathing.
- Hand tremors. A person cannot perform small movements that require precise coordination. Motor skills decrease.
- Yellowness of the sclera of the eyes. A dangerous manifestation that indicates damage to the liver structures. We need to look for gastrointestinal pathologies.
- Change in body weight. In both directions, it depends on the characteristics of the individual patient.
- Redness or blueness of the nose as a result of varicose veins of small vessels. A classic situation that reveals a drunken alcoholic.
ACM manifests itself with approximately the same symptoms from the cardiovascular, excretory, and respiratory systems. Clinical signs are nonspecific; a detailed examination is required, preferably in a hospital.
Symptoms of the disease
The danger of alcoholic cardiomyopathy is that at the initial stage the disease does not cause any specific symptoms. In most cases, the only thing that worries the patient is periodic attacks of pain in the heart. As the pathology progresses, the following symptoms appear:
- Dyspnea. It will appear not only with moderate physical activity, but even at rest.
- Swelling in the legs. In advanced cases, swelling can even appear on the thighs and other parts of the body.
- Irregular heart rhythm, feeling of a strong heartbeat in the chest.
- Discomfort in the chest area.
- Accumulation of fluid in the abdominal cavity.
- Loss of appetite.
- Reduced amount of urine when emptying the bladder.
- Problems concentrating.
- Increased fatigue, poor tolerance to physical activity.
- Cough with sputum production.
- Frequent dizziness.
If most of these symptoms are observed, this indicates irreversible damage to the heart and vascular system, as well as advanced heart failure, which are practically untreatable.
Alcoholic cardiomyopathy symptoms and treatment
Alcoholic cardiomyopathy is a special case of dilated cardiomyopathy. Most often, alcoholic cardiomyopathy occurs in men who abuse strong alcoholic drinks (vodka, cognac, whiskey), wine or beer for more than ten years.
As a rule, this disease appears in the stronger half of humanity between the ages of 30 and 55 years. In women, alcoholic cardiomyopathy is observed much less frequently. However, compared to men, women require a shorter period of alcohol abuse to develop the disease.
Alcoholic cardiomyopathy occurs in different socioeconomic strata of the population, but the disease is most common among the lower strata.
The disease develops gradually. In many patients, pronounced clinical symptoms appear after a fairly long asymptomatic period, during which the disease can only be identified with the help of special instrumental studies, and primarily echocardiography.
Symptoms of alcoholic cardiomyopathy
With alcoholic cardiomyopathy, patients experience constant heart pain; during physical activity, rapid heartbeat, shortness of breath, increased sweating, general weakness, and fatigue. Initially, these symptoms appear the next day after drinking a large amount of alcoholic beverages, then during the period of abstinence they decrease significantly, but with prolonged use of alcohol they do not completely disappear.
Subsequently, the disease progresses, shortness of breath and palpitations become constant. Many patients develop swelling in their legs and have attacks of suffocation at night. All these symptoms are signs of severe heart failure.
Treatment of alcoholic cardiomyopathy
Treatment of alcoholic cardiomyopathy is carried out simultaneously in three areas: complete abstinence from drinking alcohol, prevention and treatment of heart failure and correction of metabolic disorders that were caused by alcoholic cardiomyopathy.
If the patient does not give up alcohol, then the treatment will not give a positive result, since giving up alcohol is the basis of therapy for any stage of this disease.
Treatment of heart failure caused by alcoholic cardiomyopathy is almost no different from the treatment of a similar disease of another etiology.
Patients are prescribed:
- aldosterone blockers,
- beta blockers,
- angiotensin II receptor blockers or angiotensin-converting enzyme inhibitors, indirect anticoagulants or antiplatelet agents,
- in the presence of edema, diuretics.
Also, for alcoholic cardiomyopathy, metabolic therapy is carried out using drugs such as neoton, mildronate, trimetazidine and others. These drugs improve the symptoms of heart failure, increase the left ventricular ejection fraction and affect the regression of dystrophic changes in the myocardium.
If conservative therapy does not give the desired effect, then surgical intervention is used. Surgical treatments include biventricular pacing, mechanical devices to support left ventricular function, cardiomyoplasty, and heart transplantation.
Forecast
The patient’s further health depends on the severity of the symptoms upon initial detection, how effective the treatment is, and whether he strictly follows all the doctor’s instructions and recommendations. With complete abstinence from alcohol, adherence to work and life schedule, moderate physical and psychological stress, the prognosis is usually moderately favorable.
Clinical stages and forms
Medical scientists gave a detailed description of a disease such as alcoholic cardiomyopathy in the 70s of the 20th century. Various forms of the disease and stages of its course have been described.
This is important for doctors, as it allows them to more accurately present the picture of pathological changes in the heart and throughout the body and select the most appropriate treatment.
Forms of alcoholic cardiomyopathy
- Classical,
- Pseudo-ischemic,
- Arrhythmic.
In the classic form of cardiomyopathy, a person is bothered by the following symptoms:
- pain and interruptions in the heart,
- dyspnea,
- increased heart rate.
In the pseudoischemic form, the leading symptoms are pain in the heart, which can manifest itself both with and without physical activity. In the arrhythmic form, rhythm disturbances come to the fore, which are manifested by tachycardia and interruptions in heart function. These disorders can be so serious that the patient may feel dizzy and even lose consciousness during an attack of arrhythmia. Death may occur suddenly.
Stages of the disease
- The first stage with episodic manifestations. It develops with alcohol abuse for 10 years.
- The second stage develops in the second decade of alcoholism. All the symptoms of heart failure appear: shortness of breath, swelling, blueness of the lips, skin of the face, feet and hands, rhythm disturbances appear.
- At the third stage, severe circulatory failure develops, accompanied by dysfunction of some internal organs.
2Pathogenesis
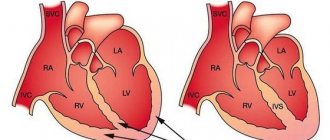
The heart is normal and affected by alcohol
The entire muscular wall of the heart is individually composed of cells called cardiomyocytes. At the cellular level, those pathological processes occur that ultimately lead to a decrease in the systolic function of the heart. The toxic effect of acetaldehyde and ethanol appears on different cell structures. In simple terms, all pathological changes can be characterized as follows:
Toxic metabolites of alcohol suppress the activity of transport proteins responsible for the entry of ions into the cell to ensure the processes of excitation and contraction of the heart. As a result, cells lose potassium and become overloaded with sodium and calcium.
Contractile proteins lose their properties and cannot participate in performing an important function - myocardial contraction. Disorders of fatty acid oxidation (peroxidation). Free fatty acids (FFA) are a source of energy for cardiomyocytes
But under the conditions of the toxic influence of alcohol metabolites, their “safe” oxidation pathway is inhibited, FFAs are metabolized with the formation of harmful substances - peroxides and free radicals. These substances can damage cell membranes, leading to myocardial dysfunction. "Catecholamine stress." By drinking alcohol, a person exposes his heart to so-called stress. The adrenal glands release large amounts of catecholamines, which increase the oxygen demand of the heart muscle, driving the heart into conditions of oxygen deficiency. Under such conditions, proper oxidation of fatty acids, conduction of impulses and ion transport are disrupted.
Diagnostic methods
The process of making a diagnosis consists of collecting complaints and anamnesis and examining the patient. They resort to further examination:
- if the heart is enlarged;
- noises are heard during auscultation;
- veins in the neck are dilated;
- legs swollen.
Also read: Post-infarction Dressler syndrome
The doctor finds out how much and in what quantities the patient determines alcohol and prescribes laboratory and instrumental tests.
Laboratory examination
Tests cannot confirm the problem, but they can help determine how damaged other organs are. To do this, they take blood for general and biochemical examination, perform liver tests, and test the blood for cholesterol. Based on the test results, a conclusion is made about the condition of the organs that could be affected by this disease.
Instrumental examination
To identify alcoholic heart damage, they resort to:
- Chest X-ray. During the procedure, X-rays are used to produce images of the heart and lungs. The doctor examines the images and evaluates the size of the organs and the presence of fluid in the cavities.
- Electrocardiography. During the procedure, electrical signals are recorded and the presence of irregularities in the heart rhythm and abnormalities in the left ventricle is detected. In some cases, daily Holter monitoring is performed.
- Echocardiography. The examination is based on examining the heart using ultrasound. The procedure makes it possible to identify structural and functional failures.
- Load tests. The patient should exercise on a bicycle ergometer, treadmill or squat. After this, record a cardiogram and check how much the body can tolerate the load. This allows us to assess the extent to which the disease has affected the stability of the cardiovascular system.
- Computer and magnetic resonance imaging. These procedures can determine the size and efficiency of the heart.
- Catheterization. The heart is examined through the vessels.
Based on the examination results, appropriate treatment is prescribed.
What happens to the myocardium of drinkers?
When alcoholic cardiomyopathy occurs, the pathological anatomy is approximately as follows: under the influence of ethylene compounds, myofibrils and their fibers die. In their place, connective scar tissue begins to grow (damaged areas heal). As a result, the myocardial layer grows in volume (hypertrophies), and the size of the cardiac cavities increases.
Now the blood flow from the veins and arteries changes its normal rhythm of movement. Doctors say that cardiac ischemia begins, that is, a delay in blood flow. The altered myocardium does not have time to contract as rhythmically as before. A disease called heart failure appears. Both it and ischemia can lead to a heart attack.
Deadly changes in the myocardium do not occur immediately or suddenly. You need to drink bitters regularly for at least 5 years for alcoholic cardiomyopathy to begin to manifest itself. The photo shows the heart of a teetotaler (right) and a beer lover (left).
How changes happen
Alcoholic drinks destroy the heart muscle through the following mechanism:
- the process of protein production in cardiomyocytes is disrupted;
- fatty acid esters are collected inside cells;
- heart cells are damaged;
- the structure is disrupted, deformation of heart cells occurs;
- spasm of the coronary arteries occurs;
- the work of the hormonal system responsible for fluid exchange is activated.
Attention! Cardiomyopathy is not the most dangerous complication for alcohol abusers. Addiction can lead to various complications from the cardiovascular system, and heart rhythm disturbances are possible. Patients with such changes are more likely to have heart attacks, and with alcoholic cardiomyopathy, instant death is possible.
Under the influence of ethyl, the heart increases significantly in size and becomes fatty. This condition involves the accumulation of lipids, that is, fats, in the myocardial tissue. This complication is often observed in patients who abuse alcohol. The disorder is difficult to correct and leads to various complications.
ACM has forms and stages, they are discussed in the table:
| Form | Description |
| Classical | The key symptom is heart failure. |
| Pseudo-ischemic | Acute pain is observed in the retrosternal region, changes are visible on the cardiogram, such as ischemic ones. |
| Arrhythmic | Attacks of shortness of breath, shortness of breath, and chest pain often occur. These symptoms are accompanied by changes in heart rhythm. |
| Stage | Description |
| First | It differs in duration, progress stretches for 10 years or more. Changes in the structure of the myocardium are not observed. Characterized by minor changes in well-being, for example, headaches, insomnia, shortness of breath. A significant change is a disruption in the flow of metabolism. |
| Second | The myocardium increases in size, hypertension appears, edema appears, and blue discoloration of certain areas of the face and body is observed. Damage to the kidneys and liver is observed. |
| Third | Heart cells die beyond repair. Cardiosclerosis progresses, accompanied by changes in heart rhythm and accompanied by chest pain. |
Diagnostics will help to accurately establish the form and stage of progress; depending on the indicators, a treatment regimen is determined.
Diagnostics
To confirm the diagnosis of alcoholic cardiomyopathy, the patient is prescribed a consultation with a narcologist and a cardiologist. After examining the patient, he may be prescribed the following additional diagnostic methods:
- ECG;
- echocardiography;
- Holter ECG;
- stress tests (treadmill test or bicycle ergometry);
- myocardial scintigraphy;
- blood and urine tests;
- blood chemistry.
Treatment of alcoholic cardiomyopathy is always complex. Its main objectives are to rid the patient of alcohol addiction and restore impaired myocardial functions.
The treatment package may include:
- antioxidants: vitamin E, Coenzyme Q10;
- drugs that stimulate protein synthesis in the myocardium: Mildronate, Trizipin long, Mildrazin, Vasomag;
- drugs that improve energy metabolism: Neoton, Cytochrome-C, Vazonat;
- antihypoxants: Mexidol, Armadin, Hypoxen, Mexicor;
- calcium antagonists: Verampil, Diltiazem;
- beta blockers: Anaprilin, Vasocardin, Concor;
- cardiac glycosides: Korglykon, Celanid, Strophanthin K;
- hepatoprotectors: Essentiale, Gepadif;
- angioprotectors: Parmidin, Anginin;
- potassium preparations: Potassium-normine, Asparkam, Panangin;
- diuretics: Trifas, Trigrim, Diuver;
- metabolic agents: Choline chloride, Riboxin.
A patient with alcoholic cardiomyopathy is recommended to follow a potassium diet, often spend time in the fresh air and provide himself with sufficient and acceptable physical activity (physical therapy, sports). To saturate the myocardium with oxygen, oxygen cocktails and hyperbaric oxygenation sessions can be prescribed.
By abstaining from drinking alcoholic beverages and following all doctor’s prescriptions and recommendations, treatment of alcoholic cardiomyopathy helps restore heart function and reduce its size. Therapy for this pathology in most cases is long-term and the patient’s recovery can occur after months or years. Further prognosis of this pathology depends on the degree of damage to the heart muscle.
Since ancient times, people have traditionally used alcohol to relieve stress, relax, or celebrate any joyful events in life. Indeed, from the point of view of health benefits, sometimes you can skip a glass or two of an alcoholic drink. However, if consumed regularly, alcohol causes irreparable harm to the human body.
The toxic effect of ethanol, which is contained in all alcoholic drinks, begins within a few minutes after its consumption. This is due to the action of acetaldehyde, into which alcohol is converted after entering the human body. This substance can circulate in the bloodstream for up to 8 hours. During this time, aldehyde has a negative effect on all internal organs. The heart and blood vessels are no exception.
The problem in the post-Soviet countries lies in the mentality of the people. Russian people do not know any sense of proportion and very often exceed harmless doses of alcohol consumed. Over the past couple of decades, teenagers and women have become overly addicted to low-alcohol drinks like beer. The main danger in this case lies not only in the constant supply of ethanol. During the brewing process, cobalt is added to the drink to increase foaming, which has a direct damaging effect on the heart muscle.
Alcoholic cardiomyopathy is heart damage that occurs under the toxic effects of alcoholic beverages. Basically, there is destruction of cardiomyocytes (muscle cells of the heart) and disruption of their metabolism.
Prognosis and prevention
Early stages of cardiomyopathy are reversible. When you stop drinking alcohol and receive treatment, the process of restoring myocardial function can begin. Advanced expansion of the cavities of the heart is difficult to treat and has an unfavorable prognosis for recovery and life.
To prevent myocardial damage, you need to stop drinking alcohol or significantly reduce its consumption. The maximum dose of ethanol that is permissible per day is (for absolutely healthy men) no more than 30 g, and for women it is half as much. In this case, at least 3 times a week it is necessary to completely eliminate alcohol.
It should be borne in mind that taking a single large dose is worst tolerated by the body in case of malnutrition or the presence of concomitant diseases.
It is also recommended to undergo a cardiovascular examination at least once a year, ensure a healthy diet and an adequate level of daily physical activity.
We recommend reading the article about arrhythmia and alcohol. From it you will learn about whether it is possible to drink alcohol if you have arrhythmia, the consequences of drinking alcohol with atrial fibrillation, which alcohol to choose and why arrhythmia occurs after drinking alcohol in healthy people. And here is more information about how dangerous ischemic cardiomyopathy is.
Alcoholic cardiomyopathy occurs due to the toxic effects of ethanol and its metabolic products on the heart. At the same time, the muscle layer weakens, and the heart chambers expand. This leads to the development of circulatory failure, arrhythmia, and thromboembolic disorders. Treatment requires a course of use of a complex of medications that increase the energy reserve of the myocardium, restoring hemodynamics inside the heart and in the body as a whole.
Treatment
The main therapeutic factor is the complete exclusion of alcohol.
Treatment is aimed at improving metabolism, energy metabolism and stimulating protein synthesis in the myocardium.
Patients are prescribed:
- Mildronate, which stimulates protein synthesis, eliminates the accumulation of toxins in cells and restores the balance between the supply and demand of cells for oxygen;
- Cytochrome C, Neoton and multivitamins that improve energy metabolism;
- vitamin E, which suppresses lipid peroxidation in cell membranes;
- Verapamil and other calcium antagonists, which have an antiarrhythmic effect, stabilize cell membranes and improve tissue respiration;
- Parmidine or Essentiale, stabilizing lysosomal membranes;
- Mexidol or other antihypoxants to eliminate oxygen starvation;
- potassium salts, normalizing electrolyte balance;
- Anaprilin or other beta-blockers that neutralize the effects of excess catecholamines;
- diuretics that relieve swelling;
- cardiac glycosides that have antiarrhythmic and cardiotonic effects in heart failure.
Surgical treatment is indicated only in emergency cases, as complications may develop.
Alcoholic cardiomyopathy also requires frequent exposure to fresh air and a diet that includes significant amounts of protein, potassium and vitamins.
Prognosis: Can sudden death occur?
According to statistics, death from alcoholic cardiomyopathy occurs within 5–7 years from the onset of its onset in the absence of treatment and continued consumption of strong drinks. The reason for this is numerous complications in the form of thrombosis and embolism, severe forms of arrhythmia. Blood clots entering the coronary or cerebral vessels result in a stroke or heart attack. In this case, the prognosis is extremely unfavorable. This disease most often leads to sudden death in drinkers.
What is the cause of death in pathology
Excessive expansion of the cavities of the heart leads to the fact that during the period of diastolic relaxation, more blood enters the ventricles than necessary. The weakened myocardium is unable to push this volume of blood into the arterial and pulmonary network. Some of the blood remains in the cavities, which further stretches the heart wall.
Due to the enlarged chambers of the heart, the diameter of the ring to which the valves between the atria and ventricles are attached increases. Their valves cannot completely block the hole during systole, so some of the blood returns back.
Comparison of the structure of a healthy heart (left) and a heart with alcoholic cardiomyopathy (right)
Such changes in intracardiac hemodynamics disrupt the movement of blood throughout the body. Stagnation occurs in both circles of blood circulation. As these manifestations increase, the heart completely loses its ability to pump blood, which ends in the death of the patient.
In addition to signs of ineffective blood circulation, a sudden stop in contractions can result in severe rhythm disturbances in the form of flicker and fibrillation, as well as thrombosis of arterial vessels with a severe heart attack or stroke.
Treatment, drugs
At an early stage, the disease can be cured without the help of medications. It is enough to completely abandon the cause of the development of cardiopathy - drinking, and change your usual lifestyle: add light exercise (for example, walking), get rid of excess weight, quit smoking, stick to a healthy diet. If all these rules are followed, the heart muscle is restored, and even a complete recovery of the patient is possible.
But if cardiomyopathy is detected in an advanced stage, drug therapy cannot be avoided. Only a doctor can prescribe them, after a complete examination. A list of medications used to eliminate the disease is presented in the table.
| Angiotensin-converting enzyme inhibitors | They dilate blood vessels, reduce pressure in the arteries, stimulate blood circulation, and reduce the load on the organ. |
| Beta blockers | They calm the increased heartbeat, prevent arrhythmia, and help the organ cope with large volumes of blood. |
| Diuretics | They remove excess fluid from the body, including from the lungs, which makes breathing easier. |
| Digoxin | Strengthens heart contraction, slows heart rate. Thanks to it, physical activity is easier to bear. |
| Blood thinners (aspirin, warfarin, Xarelto) | They relieve blood vessels and chambers of the heart from blood clots and improve blood circulation. |
At an early stage of the disease, the prognosis is favorable. If the patient can overcome alcoholism and lead a recommended lifestyle, then, most likely, recovery will occur, and cardiac function will be completely restored. The age of the patient plays a significant role in the recovery process - the younger the person, the faster the regeneration takes place.
But if the alcoholic seeks help too late, when irreversible damage has developed, or he does not maintain a sober lifestyle, then there is little chance of recovery. The heart will continue to deteriorate, the volume of blood pumped will gradually decrease, and severe arrhythmia occurs.
Causes
The main factor in the development of the pathological process is obvious - it is the abuse of alcoholic beverages over a long period of time. However, the question is not so obvious.
The timing of the development of cardiomyopathy in adult patients varies. It all depends on the individual characteristics of the body, resistance to alcohol (according to researchers, it is genetically determined, and men tolerate intoxication better than the fairer sex).
On average, from the beginning of abuse to the formation of at least minimal organic abnormalities in the heart muscle, 3-15 years pass.
Experienced patients do not always get sick, but sooner or later the result is the same. Acceleration of the development of the pathological process is possible within the course of some diseases in parallel.
Among them are mainly cardiac problems:
Congenital and acquired malformations of the heart. Discovered by chance, during testing for another condition, or during routine screening. Symptoms are usually completely absent.
According to various estimates, cardiomyopathy develops in a matter of years against the background of an ongoing organic defect. Moreover, the patient may not live to see the manifestation of the condition: early cardiac arrest, heart attack or other lethal phenomena are likely.
- Previously suffered necrosis of cardiomyocytes. The process accelerates significantly when drinking alcohol for a long time. If completely healthy people run the risk of relapse in approximately 20% of cases, the prospect is 2-4 years; for an alcoholic this figure reaches 40-60% and higher. Cardiomyopathy develops 70% faster. A few months or a year is enough. The heart is working hard. The likelihood of cure, even with complex therapy for alcohol cessation, is minimal.
- Inflammatory pathologies of cardiac structures. Myocarditis and others. They are of infectious origin. This leads to partial or complete destruction of the atria, blockade of the legs of His and the emergence of dangerous forms of arrhythmia.
When drinking alcohol, the process of developing cardiomyopathy takes 1-2 years. The probability of spontaneous, sudden cardiac arrest is about 50%, depending on your luck.
Treatment is surgical, in a hospital. A prerequisite for successful recovery is complete abstinence from alcohol. Ethanol should not be consumed even for preventive purposes.
Atherosclerosis of the aorta. Dangerous cardiovascular disease. Its essence lies in stenosis (narrowing) or occlusion (blockage) of the largest vessel in the body.
Often it is questionable recommendations for therapy that lead people to the bottle. But it is impossible to cure a problem that is metabolic in its etiology in this way. On the contrary, alcohol abuse leads to an even greater deterioration in ion metabolism.
Cholesterol is deposited more actively if, under the normal state of affairs, the duration of progression of atherosclerosis to a dangerous period is 5-7 years, here the period is reduced to 1-2.
Generalized disorders of the coronary arteries lead to cardiomyopathy and early infarction, which is difficult to treat due to multiple abnormalities.
Coronary insufficiency. A particular form of it is acute myocyte necrosis.
History of diabetes mellitus, other endocrine pathologies. Usually of a deficiency type, when not enough hormones are produced (cortisol, T3, T4, TSH, etc.).
Treatment in all cases is complicated by drinking alcohol:
- Ethanol provokes increased production of angiotensin-II, renin, and aldosterone. These substances narrow the lumen of blood vessels throughout the body.
- An activating effect on the hypothalamus and brain stem is also detected. Cerebral structures give a signal to the heart and blood vessels to increase tone. Working hard leads to the need to increase muscle mass.
- This is how the number of cardiomyocytes increases. The heart becomes unnaturally large. Such a bulky organ is no longer able to adequately pump blood.
Bradycardia and terminal failure of the left and, less commonly, right ventricular failure occur.
All systems suffer. Recovery is no longer possible. This outcome awaits drinkers in every case. Sooner or later.
Reasons for development
Alcoholic cardiomyopathy develops with excessive and long-term consumption of alcoholic beverages as a result of the damaging effects of ethanol and its metabolites on the structure of myocardial cells. With prolonged alcohol consumption, degenerative changes occur in the walls of the coronary arteries and nerve fibers of the heart, metabolism in the myocardium is disrupted, and myocardial hypoxia develops.
The determining factor in the development of the disease is the amount of alcohol consumed by the patient. Epidemiological studies have convincingly proven that mortality from coronary heart disease and the amount of alcohol consumed by the patient are in a U-shaped relationship - the highest mortality is observed in people who do not drink alcohol at all and in people who abuse alcohol. People who drink alcohol moderately are less likely to suffer from coronary artery disease, and mortality from this disease is low in this group.
There is no consensus on a safe minimum daily dose of alcohol. There is also no reliable data on how long a “dangerous dose” must be taken for the development of alcoholic cardiomyopathy.
According to studies conducted in the USA, Canada and the European Union, alcoholic cardiomyopathy develops in patients with daily ethanol consumption:
- for 10 years, if the daily dose is 125 ml;
- after 5 years, if the daily dose exceeds 80 g;
- for 20 years, if the daily dose is 120 g.
Alcoholic cardiomyopathy develops in different individuals at different daily doses and at different times. There are no exact data, since people differ in their individual sensitivity to alcohol-containing drinks (it depends on the genetically determined activity of enzyme systems that are involved in the metabolism of alcohol).
According to researchers, the development of the disease is affected by any alcoholic drink consumed in excessive quantities.
Hypertrophic cardiomyopathy
This is a type of myocardial disease with an unknown etiology, which is characterized by an increase or hypertrophy of the myocardium of the left ventricle, but sometimes, but less often of the right ventricle, often with obvious asymmetry, and with obvious disturbances in the diastolic filling of the left ventricle with a pronounced absence of dilatation in its cavity and the reasons that caused this very hypertrophy. Sometimes there is isolated hypertrophy of the apical part of the ventricles or the interventricular septum. The cavity of the left ventricle is slightly reduced, while the left atrium is expanded. Hypertrophic cardiomyopathy is very common in young people; the age of such patients can be about 30 years.
There are several stages of this disease:
— First stage (pressure gradient in the outflow tract of the left ventricle is no more than 25 mm Hg, patients do not complain) — Second stage (pressure gradient in the outflow tract of the left ventricle is no more than 36 mm Hg, complaints appear during physical activity) — Third stage ( pressure gradient in the outflow tract of the left ventricle is no more than 44 mm Hg. Patients are concerned about shortness of breath and angina pectoris - Stage Four (pressure gradient in the outflow tract of the left ventricle is no more than 80 mm Hg, and sometimes can even reach 185 mm Hg. With such a stable at the height of the gradient, pronounced hemodynamic disturbances occur with accompanying clinical manifestations)
In ordinary cases, the clinical picture is represented by: 1) phenomena of hypertrophy (mainly of the left) of the ventricular myocardium; 2) the phenomenon of insufficient diastolic ventricular function; 3) phenomena of obstruction of the left ventricular outflow tract (not in all patients); 4) phenomena of heart rhythm disturbances.
The nature of heart pain in patients with hypertrophic cardiomyopathy is different. Most patients have signs of typical angina attacks. There are some known cases of the development of myocardial infarction with a characteristic clinical picture and severe pain syndrome, extremely long-lasting in nature, which corresponds to a classic heart attack. There is also shortness of breath - the most common sign and symptom of the disease. It is observed in approximately ninety percent of cases and is explained by an increase in the last diastolic pressure in the pulmonary veins, in the left atrium. This leads to impaired gas exchange in the lungs.
Fainting and dizziness often occur due to physical and emotional stress, when walking, or when quickly moving from a horizontal to a vertical position. Many patients complain of deterioration of blood circulation in the brain, which is manifested by short-term periods of switching off, consciousness of prolapse, and speech disorders. Periods of dizziness and loss of consciousness are also caused by arrhythmias and therefore, if such symptoms exist, an electrocardiogram is mandatory.
The diagnosis of the disease is determined on those facts that reveal a characteristic combination of signs of the disease and in the absence of data that indicate pathology similar in syndromes. The following symptoms are characteristic of hypertrophic cardiomyopathy: 1) systolic murmur localized along the left edge of the sternum with preserved II sound in combination; 2) in combination with mesosystolic murmur, preservation of I and II tones on FCG; 3) carotid sphygmogram changes; 4) according to ECG and X-ray examination, enlargement of the left ventricle; 5) typical signs detected during echocardiographic examination.
Beta blockers are often used to treat hypertrophic cardiomyopathy. They reduce the vulnerability of the myocardium to catecholamines, also reduce oxygen demand and pressure gradient and prolong diastolic filling time and also improve ventricular filling. Calcium antagonists may also be prescribed. If there are heart rhythm disturbances, then Cordarone is prescribed at a dosage of 600 or 800 mg per day during the first week, then 200 and 400 mg per day. And with the development of heart failure, diuretic drugs saluretics are prescribed - Uregit and Furosemide; aldosterone antagonists - Veroshpiron and Aldactone in appropriate dosages.
What is cardiomyopathy?
The disease is a myocardial lesion characterized by thickening (hypertrophy) of the heart muscle or enlargement of the heart chamber (dilatation). As a result, congestion develops in the circulatory system, which further aggravates the patient’s condition.
Morphological structure of the alcoholic heart:
- The organ increases in size, while the walls of the ventricles hypertrophy unevenly.
- Effusion accumulates under the epicardium, which is often associated with fatty tissue, which often completely covers the myocardium.
- In the thickness of the heart muscle, fatty degeneration often forms together with focal sclerosis.
- Dilatation is mainly determined in the chamber of the left ventricle, and its greater severity is observed against the background of chronic heart failure.
Diagnostics
It is often difficult to make a diagnosis of alcoholic cardiomyopathy, because when turning to a cardiologist or therapist, patients try to hide the fact of alcohol abuse until the last minute.
Therefore it is necessary:
- ask relatives;
- If they mention the patient’s alcohol dependence, schedule a consultation with a narcologist.
A physical examination reveals:
- during a general examination - anxiety or inhibited behavior, pallor and cyanosis of the skin of the fingertips, nose, ears, upper chest, puffiness of the face;
- upon palpation (palpation) – increased sweating, swelling of soft tissues, coldness of the hands and feet, swelling and pulsation of the vessels of the neck;
- with percussion (tapping) – an increase in the size of the heart (due to hypertrophy or dilatation of its chambers);
- during auscultation (listening with a phonendoscope) – pathological systolic and diastolic noises, which indicate structural changes in the heart muscle and heart valves.
Instrumental research methods that are used in the diagnosis of alcoholic cardiomyopathy are:
- electrocardiography (ECG) – graphic recording of the bioelectric potentials of the heart. It is the main diagnostic method for this pathology. An ECG reveals rhythm disturbances and signs of organic myocardial damage, which can signal the toxic nature of the disease;
- 24-hour Holter monitoring – graphical recording of the bioelectric potentials of the heart for 24 hours. Allows you to detect changes in bioelectric potentials that were not detected during an ECG;
- bicycle ergometry – conducting an electrocardiographic study after physical activity (pedaling). Prescribed in the absence of contraindications and critical manifestations of the disease;
- echocardiography - ultrasound of the heart. Using this research method, the condition of the coronary arteries and valve apparatus is studied, myocardial hypertrophy and dilatation, a decrease in blood flow velocity are detected, and pressure in the chambers of the heart is determined. The method is used for the differential diagnosis of cardiomyopathy and pericarditis (inflammation of the heart sac);
- X-ray of the chest organs - this reveals signs of enlargement of the chambers of the heart, sometimes dilatation of the ascending aorta. The method is used to study the condition of large vessels and identify pathological neoplasms. It can also be used to suspect the development of valvular heart defects.
Laboratory research methods are additional in the diagnosis of alcoholic cardiomyopathy. This:
- general blood test - as this disease progresses, signs of anemia are determined (decreased number of red blood cells and hemoglobin);
- biochemical blood test - decrease in the amount of total protein, change in the ratio of protein fractions (albumin, globulins and others);
- blood gas analysis - there is an increase in the amount of carbon dioxide and a decrease in oxygen levels.
How does ethanol affect the heart?
Today, some companies claim that small amounts of alcohol are not harmful, and even beneficial for the body. Is this really true?
Numerous studies have proven the mythical nature of this assumption that alcohol has clear benefits for the heart. In fact, the amount of alcohol consumed is directly proportional to the severity of symptoms associated with certain diseases of the cardiovascular system and other organs. In particular, often, while drinking alcohol, there is an increase in blood pressure and, as soon as the patient stops abusing alcoholic beverages, blood pressure decreases or even returns to normal.
The harm of alcohol to the heart is confirmed by the following studies:
- Canadian scientists observed more than 3 thousand men who were 35-79 years old for 11 years. All patients were not diagnosed with any heart or vascular disease before the start of the study. The results showed that in the control group there were more strokes that occurred due to alcohol consumption. If the patient was additionally diagnosed with diabetes mellitus or was in a drunken state, then the dangerous influence of ethanol increased several times.
- Another study involved an ambulance service. Based on the statistics she provided, it was determined that in many cases alcohol was the cause of atrial fibrillation.
Thus, it turns out that ethanol has a negative effect on the body and on the cardiovascular system in particular. In significant doses it can lead to atrial fibrillation, heart attacks, and cardiomyopathy. At the same time, there is no minimum dose of alcohol in which it would be completely safe, so those who want to be healthy should avoid alcoholic beverages altogether.