Cause of death in cardiomyopathy
Cardiomyopathies are a large group of pathological conditions that lead to myocardial dysfunction and, in advanced form, to sudden death.
Experts identify several mechanisms for the typical development of cardiac lesions, which unite all types of cardiomyopathies. There are many reasons for the development of pathology, and they may be associated with myocardial disorders or do not depend on them at all. Cardiomyopathy is considered a very common disease in modern society, it occurs in 3 people per thousand of the population.
Until recently, the term “cardiomyopathy” did not include pathological lesions of blood vessels and valves of the myocardium, but since 1995, according to WHO recommendations, this concept has become applicable to all pathologies accompanied by functional disorders of the myocardium. Although most cardiologists do not classify the chronic form of arterial hypertension, valve defects, cardiac ischemia and other independent pathological conditions as cardiomyopathic varieties. Because of this, there are still discussions about the classification of diseases.
The root causes of the formation of cardiomyopathy
Cardiomyopathy is classified as a pathology of unknown etiology. It is impossible to establish the exact reasons for the formation of deviations. The main provoking factors are shown in the table.
| Factor | Description |
| Hereditary predisposition | Cardiomyopathies are often caused by genetic abnormalities. Cardiomyocytes include a large number of proteins that are involved in the contractile process. Any defect received in utero can cause abnormalities in the functioning of the entire muscle. Pathology forms independently. That is why it is classified as a primary lesion. |
| Infectious lesions | Many doctors are inclined to believe that cardiomyopathies are formed under the influence of certain infectious diseases. This is confirmed by the presence of specific antibodies in patients. The main root causes include hepatitis C and herpes sore throat. Changes occur in DNA. |
| Autoimmune disorders | Autoimmune disorders can be caused by various pathologies. Cardiomyopathy develops rapidly. The prognosis is often unfavorable. |
| Idiopathic fibrosis | Myocardial cells are replaced by connective tissue. The walls become less elastic and dense. |
Toxic cardiomyopathy occurs due to drinking alcohol and smoking. The accumulation of harmful substances significantly increases the risk of developing pathology. The disease may be a consequence of intoxication of the body.
Smoking and alcohol cause toxic cardiomyopathy
The environment has a huge impact on the body. Cardiomyopathy can be triggered by external factors that can affect DNA. These include chemical emissions, radiation emissions, etc. In women, the pathology is usually caused by the period of gestation and pregnancy. Sometimes menopause can act as a provoking factor.
People with various bad habits are at risk of developing cardiomyopathies.
Why do cardiomyopathies occur?
Since such pathologies include all myocardial lesions, as a result of this, the causes of cardiomyopathic disease become quite extensive and varied. If dysfunctional heart disorders arise as a result of other diseases, then they say that a specific, secondary cardiomyopathic form has developed. If cardiomyopathy does not have a specific cause, then its primary form develops.
Primary form
In general, the following causes of primary pathology are distinguished:
- Viral infections
Most experts are of the opinion that the development of certain cardiomyopathic forms is facilitated by certain infectious pathologies of viral etiology. Proof of this theory is the presence of specific antibodies in the patient’s body. Some viruses (cytomegalovirus, hepatitis virus, Coxsackie virus, etc.) affect cardiomyocyte DNA chains, disrupting their activity, which subsequently causes the development of cardiomyopathic pathology.
- Genetic causes
Often the development of a pathological cardiomyopathic condition is caused by genetic disorders. Cardiomyocytes (myocardial cells) contain a significant amount of proteins that affect the contractility of the heart. If, due to any genetic reason, disturbances in protein metabolism or synthesis occur in myocardial cells, then the functions of all cardiac sections are disrupted.
- Primary cardiac fibrosis
Fibrosis is a pathological process in which myocardial muscle tissue is gradually replaced by connective tissue cells. This replacement is called cardiosclerosis. With its development, the myocardial walls lose their former elasticity and become unable to contract. As a result, cardiac functions are impaired.
- Autoimmune disorders
As a result of various pathogenetic processes, autoimmune mechanisms are launched, which are almost impossible to stop. In such a situation, cardiomyopathy rapidly progresses, and its prognosis becomes unfavorable. For primary forms of pathology, symptomatic therapy is used, aimed at compensating for myocardial insufficiency, but not at eliminating provoking factors, since they remain undetected.
Secondary form
The secondary form of cardiomyopathies can be caused by many factors:
- Lesions of the heart muscle of infectious etiology;
- Myocardial ischemia;
- Pathology of accumulation;
- Hypertension;
- Electrolyte imbalance;
- Pathologies of an endocrine nature;
- Systemic connective tissue pathologies;
- Amyloidosis;
- Toxic poisoning;
- Neuromuscular pathologies;
- Cardiomyopathy in pregnant women.
Treatment of alcoholic cardiomyopathy
If the diagnosis is confirmed and the patient is diagnosed with alcoholic cardiomyopathy, treatment should be started as soon as possible, since therapy will not bring results in the later stages. Therapy is carried out in 3 areas:
- complete exclusion of alcohol;
- treatment of heart failure;
- elimination of metabolic disorders.
Doctors warn that if the patient continues to drink alcohol, treatment of alcoholic cardiomyopathy will not make sense, since the basis of any therapy is complete abstinence from alcohol. In most cases, the same regimen is used to combat pathology as in the treatment of heart failure caused by any other disease. Typically patients are prescribed:
- aldosterone blockers;
- beta blockers;
- angiotensin-converting enzyme inhibitors or indirect anticoagulants;
- diuretics (prescribed only for severe swelling).
Additionally, metabolic treatment is carried out using drugs such as Mildronate, Neoton, Trimethazine. These drugs minimize the symptoms of heart failure, increase the ejection fraction of the left ventricle and prevent subsequent dystrophic changes in myocardial structures. If drug therapy does not produce results, surgery is prescribed. The method is selected individually for each patient.
Types of cardiomyopathies
Among specialists, the most common classification of cardiomyopathic forms is according to their clinical picture. These forms differ in manifestations and structural disorders of the myocardium. Cardiomyopathy, depending on the mechanism of its development, can be:
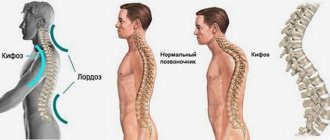
- Hypertrophic - when the walls of the myocardial chambers become thicker, the chambers themselves may remain the same volume or slightly decrease. Such a pathological condition leads to hemorrhage in the pulmonary circulation, a decrease in left ventricular volume, cardiac ischemia, and arrhythmic complications;
- Specific - when myocardial lesions develop against the background of any pathologies, and are not primary in nature. In this regard, ischemic, allergic and other cardiomyopathies of a specific form are distinguished;
- Dilation is the most common cardiomyopathic form, caused by pathological expansion of the heart chambers;
- Restrictive – characterized by a strong decrease in the elasticity of the myocardial walls, which develops mainly against the background of myocardial fibrosis;
- Unclassifiable - This form of cardiomyopathy usually has symptomatic features of several forms at the same time, which makes it difficult to specifically classify.
Types of deviation
There are 2 main types of cardiomyopathy:
- primary;
- secondary.
Primary is a pathology, the causes of which are almost impossible to restore. Secondary cardiomyopathy is also called specific. It is possible to clearly establish the root cause of the deviation.
In some cases, taking antibiotics can provoke the development of pathology.
Secondary cardiomyopathy has several forms:
- Alcoholic. Occurs with excessive consumption of alcoholic beverages.
- Infectious. Triggered by viruses and bacteria. Leads to disruption of the structure.
- Medicinal. Associated with the use of medications. More often occurs after taking antibiotics.
- Toxic. Caused by intoxication of the body with various chemicals.
- Dishormonal. Caused by hormonal imbalances in the body.
- Post-radiation. Appears after radiation therapy.
- Stressful. Caused by strong shocks.
- Peripartum cardiomyopathy. Forms after pregnancy in girls.
Cardiomyopathy of mixed origin is a pathology that combines several causes of manifestation. Treatment is selected depending on the form of the deviation.
Anxiety and stress can also cause heart problems
The primary complex of pathologies is:
- stagnant;
- hypertrophic;
- retractive;
- arrhythmogenic dysplasia of the right ventricle.
Congestive pathology is characterized by an enlargement of all cavities of the heart. The contractile function of the myocardium decreases. The deviation can appear in people over 30 years of age. Doctors say that the root cause of the pathology is infections, toxic poisoning, hormonal imbalances and autoimmune disorders. Most often due to hereditary predisposition. The pressure in the lungs and cavities of the heart increases. The boundaries of the organ are expanded. Deformation of the chest occurs. The left ventricle is hypertrophied.
In hypertrophic cardiomyopathy, the myocardial walls thicken
Hypertrophic cardiomyopathy is characterized by thickening of the myocardial walls. It is considered a hereditary pathology. It appears more often in men. The muscle layer of the ventricle hypertrophies, that is, the heart enlarges mainly on the left. The push moves. The size of the cavities decreases. The myocardium contracts worse.
Restrictive cardiomyopathy is an infrequently diagnosed pathology. The ventricles relax inadequately. There is no pronounced hypertrophy. Congestive insufficiency of blood flow occurs. There is severe shortness of breath. The patient experiences weakness even with the most minor strength loads.
Arrhythmogenic cardiomyopathy is characterized by the replacement of cells in the right ventricle with adipose tissue. The pathology is rare and poorly studied. Capable of developing during adolescence. The myocardial walls become thinner.
When replacing muscle tissue with fat, arrhythmogenic cardiomyopathy is diagnosed
Possible cardiomyopathic complications
Cardiomyopathy primarily affects the myocardium, although the consequences of the development of pathology affect various cardiac sections, the disruption of which affects the heart completely. With the development of pathology, the risk of developing many complications increases, which can lead to the death of the patient. Therefore, these conditions must be avoided. Such dangerous complications include:
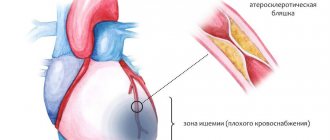
- Heart attack
This pathological condition is necrosis of a certain area of the myocardium, which developed due to insufficient blood circulation. This complication is considered a dangerous manifestation of the development of cardiac ischemia. Hypertrophic cardiomyopathy is more often than other forms complicated by myocardial infarction, since in it the heart experiences acute deficiency in nutrition and oxygen.
After a heart attack, the formation of connective tissue areas occurs on the myocardial tissue, which leads to post-infarction cardiosclerosis, and in its advanced form, to death.
A developed heart attack makes itself felt by chest pain, sometimes radiating to the left forearm or lower jaw. Patients' skin color often becomes pale, they suffer from shortness of breath and cold sweat, and their pulse is irregular and weak. If therapeutic intervention was timely, then further necrotization of the myocardium can still be stopped.
- Myocardial failure
This complication is a fairly common pathological phenomenon in cardiomyopathic forms. More often than others, cardiomyopathy is complicated by chronic heart failure, the signs of which manifest themselves in the form of tissue hypoxia and decreased myocardial output. Acute myocardial failure is characterized by sudden development and is fraught with cardiogenic shock. If resuscitation measures are not taken, heart failure quickly leads the patient to death, since hypoxia is detrimental to brain cells. Myocardial failure can be diastolic and systolic in nature. Diastolic failure is based on insufficient blood supply to the ventricle at the time of its relaxation. This clinical picture is most typical for restrictive cardiomyopathy. The systolic form of failure is manifested by a weakening of myocardial contractions and a decrease in the ejection fraction. This is most typical for the dilated cardiomyopathic form.
Read also: Hypertrophic cardiomyopathy diagnosis and treatment
According to statistical data, in almost all patients (90%) cardiomyopathy is complicated by various types of arrhythmias caused by structural tissue disorders that disrupt the distribution of impulses through the cardiac tissues. The most dangerous is considered to be arrhythmia localized in the ventricles, since it is characterized by large-scale disturbances in blood pumping and often leads to the death of the patient.
- Thromboembolism
Any cardiomyopathy is fraught with thrombus formation, which is associated with disturbances in blood flow between the chambers of the myocardium. The stagnation and turbulence that forms in the vessels contribute to the activation of the blood clotting system, as a result of which blood cells stick together and a blood clot forms. If this thrombus leaves the myocardial cavity and becomes fixed in any of the vessels in the periphery, then thromboembolism is diagnosed. This condition disrupts blood supply, provokes tissue death and can lead to the death of the patient.
The most dangerous thromboembolic forms are considered to be: ischemic stroke (death can occur when a blood clot enters the brain area), pulmonary arterial thromboembolism, intestinal necrosis, thrombosis of the vascular system of the extremities.
- Pulmonary edema
This complication is a consequence of severe blood stasis in the pulmonary circulation. Typically, this condition develops if cardiomyopathy is localized in the left half of the myocardium and is stagnant.
If the left half of the heart cannot cope with the incoming volume of blood, then its excesses accumulate in the pulmonary vessels. This promotes vascular dilation, as a result of which blood plasma begins to leak and accumulate in the alveoli.
The patient develops symptoms such as respiratory distress, moist rales, and pinkish sputum. If in such a condition the patient does not receive urgent medical assistance, then pulmonary edema in a short time leads to death due to cessation of blood circulation and breathing.
The prognosis of cardiomyopathy is often unfavorable, since the pathology is dangerous due to the progression of myocardial failure, thromboembolic and arrhythmic complications (tachycardia, ventricular extrasystoles, atrial fibrillation, etc.), myocardial conduction disorders, and sudden coronary death. According to statistics, when dilated cardiomyopathic form is diagnosed, only a third of patients survive 5 years. Long-term survival of patients is possible only in the case of a heart transplant, which is complicated by the high cost of the operation and the lack of donor organs. Unfortunately, specific preventive methods for cardiomyopathic pathologies have not yet been developed.
Symptoms
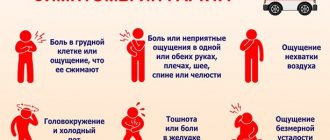
The clinical picture of HCM includes a typical triad of symptoms:
- chest pain;
- rhythm disturbances;
- syncope - fainting.
Pain in the heart region is very similar to that of angina pectoris (pulling/squeezing pain behind the sternum, aggravated by physical activity), because it is caused by myocardial ischemia. Its characteristic difference is that it not only does not improve after taking Nitroglycerin, but can become even stronger. This is explained by the fact that the drug dilates blood vessels, which lowers blood pressure. This makes the heart beat faster. A high heart rate reduces the diastole phase, during which blood supply to the myocardium occurs.
Fainting or pre-fainting conditions (dizziness, darkening of the eyes, a feeling of “lightheadedness”) occur due to obstruction of the left ventricular outflow tract by thickened myocardium, as a result of which the blood supply to the brain deteriorates. Various arrhythmias also cause fainting.
The patient feels heart rhythm disturbances as attacks of rapid heartbeat and “interruptions.” With HCM, dangerous arrhythmias quite often develop: paroxysmal ventricular tachycardia, ventricular fibrillation, atrioventricular block.
In the later stages of the disease, signs of chronic heart failure appear:
- general weakness, rapid fatigue;
- shortness of breath, which worsens when doing physical work or lying down;
- a feeling of heaviness or aching pain in the right side under the ribs due to an enlarged liver;
- swelling of the legs, especially noticeable in the evenings.
I would like to note that the presence of symptoms and its severity depend on the degree of thickening of the walls of the heart and the rapidity of development of this process, which proceeds differently for everyone. Sometimes HCM quickly leads to disability, and someone may experience a completely asymptomatic course, which accompanies a good prognosis.
A person with HCM may feel completely healthy for a long time and not experience any discomfort. The first symptoms are usually the sudden onset of chest pain or loss of consciousness during sports. If someone in your family has been diagnosed with HCM and you suddenly experience heart pain with dizziness, see your doctor as soon as possible.
With hypertrophic cardiomyopathy, symptoms may not appear for a long period of time. Typically, the first signs of the disease appear between the ages of twenty-five and forty years. Today, doctors identify nine forms of the clinical course of this heart disease:
- Lightning fast.
- Mixed.
- Pseudovalve.
- Decompensation.
- Arrhythmic.
- Heart attack-like.
- Cardialgic.
- Vegetodystonic.
- Asymptomatic.
Thus, with the non-obstructive form of the disease, only minor symptoms are observed. There are no disturbances in the outflow of blood. Shortness of breath and interruptions in the functioning of the heart muscle may occur. During physical exercise and stress, pulse irregularities can be observed.
The symptoms of obstructive hypertrophic cardiomyopathy are more pronounced. Seventy percent of patients experience the development of anginal pain. The vast majority of people suffering from this heart disease experience shortness of breath (approximately ninety percent of cases). Half of the patients complain of dizziness and fainting. It is also possible that:
- transient arterial hypertension;
- heart rhythm disturbances;
- atrial fibrillation;
- extrasystoles;
- paroxysmal tachycardia.
Hypertensive cardiomyopathy in elderly patients may also be accompanied by arterial hypertension. The exact number of patients is unknown, but some data suggest that the phenomenon is quite common among older people with this heart disease.
In some cases, this disease in patients is accompanied by cardiac asthma and pulmonary edema. But, despite all the symptoms described above, quite often the only manifestation of HCM in patients is sudden death. In this case, for obvious reasons, it is not possible to help the patient.
The type of disease affects the symptoms of hypertrophic cardiomyopathy. With non-obstructive, the patient does not feel discomfort because the blood flow is not impaired. This form is considered asymptomatic. With obstructive form, the patient exhibits symptoms of cardiomyopathy:
- dizziness;
- dyspnea;
- high pulse;
- fainting;
- chest pain;
- systolic murmur;
- pulmonary edema;
- arterial hypotension;
- a sore throat.
A patient who knows what cardiac hypertrophy is is well aware of the manifestations of the disease. These signs are explained by the fact that the disease does not allow the heart to cope with its work as before; human organs are poorly supplied with oxygen. If such symptoms make themselves felt, you should consult a cardiologist for advice.
Predictions of death from cardiomyopathy
Cardiomyopathy is a heart disease manifested by pathological changes in myocardial tissue. The disease can occur at any age, regardless of gender, but most often it is diagnosed in men.
If you do not begin timely treatment of cardiomyopathy, the disease will develop into heart failure, in which the quality of life deteriorates significantly.
In addition, the disease can lead to serious consequences, which often end in the death of the patient.
- All information on the site is for informational purposes only and is NOT a guide to action!
- can give you an ACCURATE DIAGNOSIS !
- We kindly ask you NOT to self-medicate, but to make an appointment with a specialist !
- Health to you and your loved ones!
Treatment of pathology
The cause of death is increasingly being identified as unspecified cardiomyopathy. The pathology remains asymptomatic for a long period of time. Death occurs suddenly. It is advisable to periodically undergo diagnostics for prevention.
It is possible to significantly improve the condition through the introduction of stem cells. For a long time, the only and radical method of eliminating pathology was a heart transplant. This method is not widespread. This is due to the small number of clinics and doctors who specialize in transplantation. Over 25 years, about 300 hearts were transplanted.
In some cases, radical treatments are necessary, such as a heart transplant.
The patient may not wait for a suitable donor. Stem cell treatment is considered a good alternative. They do not have specific characteristics and are universal. The therapy can improve the elasticity and performance of the heart muscle.
To improve the condition, the patient must give up bad habits. Nutrition should be reconsidered. Excludes:
Food should be balanced and healthy. Include as many fruits and vegetables in your diet as possible. It is necessary to follow a diet.
You should strictly adhere to your diet, do not eat fatty or fried foods.
There is no specific treatment for cardiomyopathy. Therapy is aimed at eliminating the risk of complications. Physical activity should be reduced. The patient is prescribed diuretics. Thanks to them, venous congestion is prevented. It is recommended to take antiarrhythmic drugs. In advanced stages, surgical intervention is indicated.
The patient should get complete rest. You cannot overwork yourself physically and mentally. The diet and basic recommendations must be followed for the rest of your life. Otherwise, complications will begin to form.
Major complications
With cardiomyopathy, irreversible processes occur in the heart that change its structure. Cardiomyocytes, the heart cells, are the first to be affected. They undergo dystrophic and sclerotic changes, characterized by thickening of the myocardial walls, stretching of the ventricles and the formation of interventricular adhesions.
All processes occurring during cardiomyopathy disrupt the inflow and outflow of blood, which entails many complications. This disease always affects ventricular function and affects the myocardium.
Based on the reasons for its appearance, cardiomyopathy is divided into primary and secondary. Based on functional changes in the myocardium, the disease is divided into four types:
Each of these types of disease has its own characteristics in damage to the heart muscle and symptoms. But they all end in serious complications, which often result in the patient’s disability or death.
The main causes of death in cardiomyopathy include the following complications:
Heart failure
The syndrome is manifested by a violation of the pumping function of the heart muscle, which leads to poor blood supply to the entire body. The clinical picture depends on which ventricle is affected.
In the case of left-sided heart failure, fluid stagnation occurs in the pulmonary circulation. The main complication in this case is pulmonary edema.
- dyspnea;
- cough (foamy or dry);
- orthopnea;
- cardiac asthma;
- attacks of suffocation;
- breathing problems (lack of air).
- swelling of the lower extremities;
- fast fatiguability;
- dyspnea;
- cough with sputum production;
- accelerated heartbeat;
- attacks of dizziness;
- pain in the right hypochondrium (associated with liver edema);
- dyspeptic manifestations;
- kidney dysfunction.
Each type of heart failure is accompanied by chronic fatigue and fatigue. Treatment of the pathology is carried out with drugs that eliminate edema, stabilize heart contractions and prevent the formation of blood clots. The same medications are used to treat cardiomyopathy.
To determine congestive cardiomyopathy, manifested by heart failure, the patient is prescribed the following diagnostic methods:
- ECG;
- radiograph;
- echocardiogram;
- Ultrasound of the heart;
- MRI;
- physical exercise testing.
What is secondary cardiomyopathy and how it is expressed, read here.
Myocardial infarction
Most often, myocardial infarction occurs with hypertrophic cardiomyopathy. The condition is the death of a section of the myocardium, formed due to poor blood supply.
A lack of blood during a heart attack is caused by the formation of a thrombus (blood clot), which clogs the vessel and prevents blood from entering the cavity of the heart and its tissues. How extensive the myocardial damage will be depends on how much blood will not flow into the organ.
Symptoms of a heart attack are increasing in nature and are manifested by the following signs:
- chest pain of prolonged and intense etiology;
- chest tightness;
- nausea;
- vomit;
- difficulty breathing;
- panic attack;
- causeless anxiety;
- dizziness;
- heavy sweating;
- loss of consciousness.
As the heart attack progresses, pain from the sternum spreads to the lower and upper parts of the body. A person feels pain in the forearm, back, jaw, and stomach. The skin becomes pale and sticky. During myocardial infarction, the pulse becomes weak and irregular.
Read also: Cardiomyopathy video
After a heart attack, adhesions form on the tissues of the heart muscle, leading to post-infarction cardiosclerosis. An advanced form of such a process will inevitably lead to the death of the patient.
Thromboembolism
Cardiomyopathy can be complicated by the development of thromboembolism - a congestive process in the blood vessels caused by a blood clot. The appearance of such clots disrupts the blood supply, provokes the death of myocardial tissue and can result in the death of the patient.
Thromboembolism can cause ischemic stroke, often fatal, due to the release of a blood clot entering the brain area. The disease can also provoke death of intestinal, lung, kidney tissue and necrosis of the extremities.
The symptoms of thromboembolism depend on the location of the blockage of the vessel. If the blood clot is located in the lower extremities, the pathology is accompanied by pain and the formation of gangrene. Blockage of blood vessels in the abdominal cavity is manifested by acute abdominal pain, vomiting, and nausea.
A blood clot formed in the right ventricle or atrium can cause heart failure and congestion in the systemic circulation. If such a blockage comes off, then the process of pulmonary embolism will be inevitable, which in 70% of cases ends in death.
Thrombotic blockages formed in the left side of the heart almost always lead to myocardial or cerebral infarction.
The treatment of cardiomyopathy must include drugs that prevent the development of thromboembolism.
Cardiomyopathy is often complicated by arrhythmias, which are diagnosed in almost 90% of all patients. Arrhythmia is a pathological condition of the heart muscle in which disturbances occur in the contractile functioning of the organ.
Arrhythmia is divided into two types:
Causes of hypertrophic cardiomyopathy
Hypertrophic cardiomyopathy is most often inherited. It is based on inherited defective genes encoding the synthesis of myocardial contractile protein. Genes can mutate spontaneously due to external factors.
Since doctors have not yet fully determined the primary and secondary forms of hypertrophic cardiomyopathy, some doctors argue that a long and stable increase in blood pressure in older patients can lead to the appearance of cardiomyopathy if changes in the structure of the heart occurred during their intrauterine development.
The main risk factors are hereditary predisposition and age over 20 years.
Impact of cardiomyopathy on health
The specificity of a disease such as cardiomyopathy should be considered an exclusively negative effect on the heart muscle, without neutralization of which there is a high risk of complications that provoke the development of heart failure, which without treatment or if it is insufficient can become fatal. To understand the importance of timely diagnosis of this disease, you should familiarize yourself with the likely complications after it, as well as the likely consequences for the patient’s health.
Today, there are several varieties of this pathology, which differ to some extent in symptoms and health effects. However, all types of this disease pose a serious danger to the patient, including death. And although doctors do not have a consensus on the degree of impact of the consequences of cardiomyopathy on the cardiac system, the opinion that this disease is fatal for the majority of those affected has a completely scientific and practical justification.
The most dangerous consequences
Medical statistics also show that at an advanced stage of the cardiac lesion in question, there is a high probability of the occurrence of conditions that subsequently become incompatible with the patient’s life. Such diseases tend to quickly worsen, causing dangerous consequences during exacerbations.
However, one should not assume that when a diagnosis of cardiomyopathy is made, the only result is the inability to improve the condition and save life. With the necessary and timely therapeutic intervention, constant monitoring of one’s own condition and visiting a doctor with the necessary diagnostics, the disease can go into remission with a gradual decrease in the intensity of symptoms and an improvement in basic health indicators.
All varieties of this cardiac pathology lead to serious disturbances in the functioning of the heart muscle, which entails, without the necessary therapeutic effect, certain complications in the patient’s health with the possibility of disability and even death. Therefore, attention to the condition of the myocardium and the functioning of the cardiovascular system will allow timely detection of negative changes and prevent the likelihood of complications.
Diagnostics
Early detection of the disease and initiation of treatment reduces the mortality rate and prolongs the life of the cat. Animals at risk must undergo regular examinations by a veterinarian 2 times a year.
The main diagnostic method is echocardiography. With its help, the doctor calculates the thickness of the heart walls, monitors the operation of the valve apparatus and obtains an objective picture of the condition of the animal’s heart.
Additionally, an ECG and chest x-ray are prescribed. An ECG reveals characteristic signs of left ventricular hypertrophy. On x-rays, the doctor is able to visually see the expansion of the boundaries of the heart.
The following symptoms may indirectly indicate HCM:
• Slight increase in breathing.
• Cardiopalmus.
• Heart murmurs.
They do not have great prognostic accuracy, but they allow one to suspect the onset of the disease.
Causes of death in cardiomyopathy
Today, there are a number of the most common causes of death in the development of caryomyopathy, which especially often entail negative changes in myocardial tissue that are incompatible with life. The conditions listed below that are dangerous to the health and life of the affected person can be amenable to therapeutic correction, which will be the more successful the earlier the disease is diagnosed.
These reasons include the following pathological conditions:
- heart failure, which causes stagnation of fluid in tissues and arteries during blood circulation due to a significant slowdown in blood movement. In this case, pulmonary edema develops, which is manifested by the formation of foam in the patient when breathing, and intermittency of respiratory movements. The cause of death in this case is the rapid formation of severe tissue swelling and lack of breathing, which leads to suffocation;
- myocardial infarction - this cause is determined by the gradual necrosis of heart tissue due to circulatory disorders, and the sudden death of the patient is caused by the formation of a blood clot and its separation due to insufficient blood supply. The extent of the heart attack is determined by the duration of the period of absence of the required amount of blood in the heart. After a myocardial infarction, adhesions occur in the tissues of the heart, which, if the process lasts for a long time, inevitably leads to death;
Read also: Drugs for the treatment of cardiomyopathies
- thromboembolism, in which a blood clot (thrombus) breaks away from the walls of a blood vessel with a high probability of blockage and subsequent death. When a blood clot forms in the left ventricle of the heart, congestion occurs in the circulatory processes, resulting in heart failure. When a blood clot is found in the left ventricle, a cerebral infarction is diagnosed. In some cases, thromboembolism is accompanied by the death of part of the intestinal and kidney tissues, where tissue necrosis occurs;
- the presence of arrhythmias can be considered an almost obligatory concomitant manifestation of cardiomyopathy; in this case, both a suspension of cardiac contractility and an increase in it can be observed, which in both cases leads to a worsening of the pathology. Arrhythmias that occur with cardiomyopathy are accompanied by external manifestations such as shortness of breath, nervousness and confusion, and deterioration in perception of reality. The treatment method for arrhythmias consists of regularly taking antiarrhythmic drugs, which are also prescribed by a cardiologist for cardiomyopathy;
- Pulmonary edema is one of the most common phenomena that, in combination with cardiomyopathy, leads to death in the patient. Significant accumulation of fluid in the lungs leads to attacks of suffocation followed by death if the disease is not treated. The main manifestations of pulmonary edema should be considered the appearance of cold sweat, severe difficulty breathing, swelling and enlargement of the veins. The neglect of the condition is accompanied by the appearance of a thread-like pulse and confusion. At this stage, the patient's survival rate decreases significantly.
However, according to statistical data, the most common cause of death in cardiomyopathy is alcohol poisoning of the body: in this case, with prolonged and significant consumption of alcoholic beverages, tissue degeneration and significant negative changes in the functioning of organs and their systems occur.
Alcoholic form of cardiomyopathy
Death often occurs with the alcoholic form of cardiomyopathy, when the body is poisoned by the breakdown products of ethanol, which occurs under the influence of digestive enzymes. Long-term consumption of alcoholic beverages (more than 10 years in a row) in almost every case leads to the occurrence of alcoholic cardiomyopathy, which, in the absence of treatment (primarily complete cessation of alcohol intake) always ends in the death of the patient.
Symptoms such as hand tremors (tremors), bluish skin discoloration, gait instability and frequent dizziness should be considered the most characteristic of this type of cardiomyopathy. With further progression of this condition, symptoms such as increased nervousness, mood lability and frequent mood swings, attacks of tachycardia, shortness of breath even with minor exertion are noted.
Unspecified cardiomyopathy, which is one of the varieties of the disease in question, largely poses a real threat to the health of the victim, since along with the degenerative phenomena characteristic of this disease in the walls of blood vessels, their sclerotization is noted for reasons that are not established during the examination of the patient. The treatment method for this type of disease is not significantly different from the method of therapeutic treatment for other established types of the disease.
The conditions listed above, which can cause death if cardiomyopathy worsens, are largely correctable with medication. A diagram of such an effect should be drawn up only by the attending cardiologist, who will be able to take into account all the features of the course of the disease and the patient’s body, and monitor the progress and dynamics of the treatment process. Monitoring the condition and timely diagnosis in this case should be called the two most important components in determining the degree of effectiveness of the treatment.
Causes of occurrence and mechanism of development of disorders
Hypertrophic cardiomyopathy is usually caused by gene mutations.
These mutations are thought to cause the heart muscle to grow abnormally thick. People with hypertrophic cardiomyopathy also have altered alignment of the heart muscle fibers. And the cells in the fibers stop contracting synchronously, which often leads to heart rhythm disturbances. The severity of hypertrophic cardiomyopathy varies widely. Most people with hypertrophic cardiomyopathy have a form of the disease in which the interventricular septum (the partition between the two lower chambers of the heart) becomes significantly enlarged, impeding blood flow. This condition is called hypertrophic obstructive cardiomyopathy.
Another common form of the disease is cardiomyopathy without significant obstruction to blood flow. However, in this case, the elasticity of the heart muscle suffers, the myocardium becomes rigid, which reduces the amount of blood ejected by the heart into the vascular system with each contraction. This form is called non-obstructive hypertrophic cardiomyopathy.
The main cause of hypertrophic cardiomyopathy is a genetic mutation. To date, about 11 genes are known, changes in which lead to the development of the described disease. They are responsible for the production of various proteins that make up the muscle fibers of the myocardium - troponins, light and heavy chains of myosin, actin, etc. Violation of the synthesis of one of them leads to thickening of the myocardium.
Most often, hypertrophy does not develop evenly, but only in one area of the LV. Particularly unfavorable is the thickening of the upper part of the interventricular septum, which narrows the lumen of the LV outflow tract. Due to pathological growth, muscle fibers begin to be arranged randomly. This creates conditions for the circulation of nerve impulses, which contributes to the development of rhythm disturbances. In addition, the myocardium is replaced with connective tissue.
Another big problem with HCM is the occurrence of myocardial ischemia, i.e., deterioration of the blood supply to the heart muscle. There are two reasons for this: compression of blood vessels by hypertrophied myocardium and impaired relaxation of the organ (diastolic dysfunction). And, as you know, the heart itself fills with blood precisely in the diastole phase.
Hypertrophic cardiomyopathy also has rarer causes:
- hereditary diseases - Fabry disease, neurofibromatosis;
- neuromuscular diseases - Friedreich's ataxia;
- endocrine pathologies – acromegaly, pheochromocytoma;
- metabolic disorders – amyloidosis;
- use of medications - anabolic steroids, tacrolimus, hydroxychloroquine.
Hypertrophic cardiomyopathy is a primary hereditary heart disease. The type of inheritance is autosomal dominant. Patients experience hypertrophy of the ventricles of the heart in combination with a reduced volume of their cavities (although in some cases this indicator is normal).
The disease is independent of other cardiovascular diseases. With it, thickening of the myocardium of the right or left ventricle is observed. As mentioned earlier, the disease most often affects the left ventricle.
The arrangement of cardiomyocytes in patients with hypertrophic cardiomyopathy is disordered. Myocardial fibrosis is also observed. In most cases, hypertrophy affects the interventricular septum. Less commonly, the apex and middle segments of the heart ventricle (in thirty percent of cases, disorders are observed in only one segment).
The disease is considered a familial disease and is directly transmitted from one family member to another. But sometimes sporadic cases of hypertrophic cardiomyopathy occur. In both cases, the underlying cause of heart disease is a defect at the gene level.
It has been established that gene mutations that provoke the development of the disease concern myofibril proteins. However, the mechanism of this effect is still unclear. In addition, the current level of development of scientific knowledge does not make it possible to explain why people with the same mutations develop heart diseases of varying severity.
Hypertrophic cardiomyopathy affects approximately 0.2–1.1 percent of the population. Males are more likely to experience this disease (about twice as many). Most diagnosed cases are in patients between thirty and fifty years of age.
In fifteen to twenty-five percent of cases, the disease is accompanied by coronary atherosclerosis. Five to nine percent of patients suffer from infective endocarditis, which occurs as a complication of hypertrophic cardiomyopathy. In this case, the disease affects the mitral and/or aortic valve.
Most patients suffering from this heart disease die due to sudden death. The risk of such death depends on the age of the patient and a number of other factors. In most cases, sudden death due to hypertrophic cardiomyopathy occurs in childhood and young adulthood. Hypertrophic cardiomyopathy rarely causes death in children under ten years of age.
Most often, death during the disease occurs when the patient is at rest (up to sixty percent).
Electrical instability of the heart (ventricular fibrillation) is the most common cause of death in patients with hypertrophic cardiomyopathy. Instability can be caused by:
- Morphological changes taking place in the myocardium (fibrosis, disorganization).
- Premature excitation of the LV or RV through latent pathways.
- Ischemia.
In some cases, sudden death in hypertrophic cardiomyopathy occurs due to conduction disturbances. A similar problem arises due to complete atrioventricular block or the development of sick sinus syndrome.
Prognosis for cardiomyopathy
Such a pathological condition as a violation of the condition and functioning of the myocardium with the manifestation of changes in its tissues is a serious lesion of the cardiovascular system, in which a number of irreversible consequences are noted, often leading to the death of the patient. The survival rate for any type of this disease is about 25-30%. In the absence of the necessary therapeutic and medicinal effects, the survival rate is significantly reduced.
The average life expectancy for any type of cardiomyopathy is 5-8 years. Giving up bad habits, intensifying daily life, introducing healthy standards of living and nutrition will prevent the worsening of the current disease and prolong the patient’s life. However, when diagnosing this lesion, you should constantly be under the supervision of the attending cardiologist, follow all his recommendations and adhere to the chosen method of treatment.
Treatment methods and life expectancy
The disease often develops in young men who do not control physical activity and in obese people. Without therapeutic therapy and limitation of exercise, the prognosis will be sad - cardiac cardiomyopathy leads to sudden death. The mortality rate among patients is approximately 2-4% per year. In some patients, the hypertrophic form becomes dilated - an increase in the chamber of the left ventricle is observed. According to statistics, the average life expectancy for hypertrophic cardiomyopathy is 17 years, and for severe forms it is no more than 3-5 years.
Treatment of hypertrophic cardiomyopathy includes medical and surgical methods. Medicines are designed to maintain the condition and remove the symptoms of increasing complications. Only a heart transplant can completely rid a person of the disease. But there are other surgical interventions that make the patient’s life easier:
- ventricular septal myectomy is an effective and frequently used method, which involves the removal of a thickened section of the interventricular septum;
- septal alcohol ablation - injection of ethyl alcohol into areas of hypertrophied myocardium, which leads to their death and a decrease in the thickness of the walls of the left ventricle;
- resynchronization - installation of special electrodes in the heart that send appropriate signals. The peculiarity is that thanks to the procedure, the excitation wave comes with a slight delay and first captures the apex, then the septum of the organ, as a result of which the pressure in the left ventricle decreases and the degree of obstruction of its outlet section decreases.
There are strict indications for surgical treatment of hypertrophic cardiomyopathy:
- high pressure in the LV outflow tract at rest (more than 50 mm Hg);
- pronounced thickening of the LV wall (more than 30 mm);
- vivid clinical symptoms (pain, fainting).
To relieve the symptoms of hypertrophic cardiomyopathy, I prescribe the following medications:
- beta-blockers (Bisoprolol, Metoprolol) are effective medications that reduce the severity of clinical manifestations (shortness of breath, heart pain, palpitations) and slow down the progression of the disease. They reduce heart rate and improve blood supply to the myocardium. However, it is always necessary to start taking them with small doses. If the heart rate slows to 55 beats per minute or lower, you should immediately reduce the amount of the drug consumed;
- calcium channel blockers (Verapamil, Diltiazem) - I prescribe them if the patient has contraindications to taking beta blockers (bronchial asthma, chronic broncho-obstructive pulmonary disease, AV blockade of the second and third degrees);
- potassium-sparing diuretics (Spironolactone) - they are used in the development of chronic heart failure to remove excess fluid from the body;
- I use diuretics (Torasemide, Hydrochlorothiazide) for severe symptoms of blood stagnation: constant shortness of breath, severe swelling of the legs, accumulation of fluid in the chest and abdominal cavities;
- anticoagulants - many patients with HCM often develop atrial fibrillation, which increases the risk of blood clots and stroke, so they need to take blood thinning medications (Warfarin, Dabigatran, Rivaroxaban);
- antiarrhythmic drugs - almost all patients with HCM experience life-threatening rhythm disturbances, for the purpose of controlling which Disopyramide, Amiodarone, Sotalol can be prescribed.
Patients with HCM should never use vasodilators (medicines that cause blood vessels to dilate). These include nitrates, AFP inhibitors, sartans, as well as calcium channel blockers: Amlodipine and Nifedipine. These medications cause reflex tachycardia, that is, they literally “make” the heart beat faster, which only aggravates the disease, so I try to avoid prescribing them.
There are patients who have a very high risk of sudden cardiac death - they have already had similar cases in their family, they faint and have severe rhythm disturbances on the ECG (frequent extrasystoles, constant supraventricular and ventricular tachycardia, etc.). Such patients may be shown:
- implantation of a cardioverter-defibrillator - sewing a special device under the skin of the chest that can immediately stop the rhythm disturbance that has arisen. It allows you to reduce the risk of death from arrhythmia to almost zero;
- radiofrequency catheter ablation – laser destruction of areas of pathological impulses.
Treatment options
To increase the effectiveness of health procedures, it is necessary to consult with multidisciplinary specialists, because the clinical manifestations of this disease are quite diverse.
If the clinical picture of the disease manifests itself clearly, VKPM is treated with the following:
- activators of myocardial metabolism;
- B vitamins;
- β-blockers;
- antiarrhythmic drugs;
- anticoagulants;
- potassium salts;
- cardiac glycosides;
If the patient's condition threatens his life, the heart rhythms are disturbed, it is recommended to implant a pacemaker or cardioverter-defibrillator.
In the most complex and advanced cases, a heart transplant may be required.
The prognosis of VCMP is unfavorable and depends on how the primary disease progresses and the severity of complications associated with the heart. The ability to work of patients with this diagnosis is impaired.
What it is?
Alcoholic cardiomyopathy is a secondary myocardial disease that is caused by alcohol consumption. Occurs due to the toxic effect of ethanol on myocardial cells. Causes heart failure, often accompanied by myocardial ischemia.
There is an increase in all parts of the heart muscle, as well as stretching of the walls of the chambers and partitions, which become thin and lose their tone. The disease is often detected in men who abuse alcohol.
Drug treatment
It is most often not possible to influence the cause of the disease. Therefore, treatment of dilated cardiomyopathy is pathogenetic and symptomatic:
- To stop the processes of wall stretching and sclerosis, angiotensin-converting enzyme inhibitors and sartans are used. These drugs eliminate the influence of RAAS hormones - dilate the arteries, reduce the load on the heart, improve nutrition, and promote the reverse development of hypertrophy.
- Beta-blockers - slow down the rhythm, block ectopic foci of excitation, reduce the effect of catecholamines on heart tissue, and reduce the need for oxygen.
- In the presence of stagnation, diuretics are used, and diuresis, potassium and sodium levels in the blood must be monitored.
- If there are rhythm disturbances, such as a permanent form of atrial fibrillation, then it is customary to prescribe cardiac glycosides. These medications lengthen the time between contractions and the heart stays in a state of relaxation longer. During diastole, the myocardium receives nutrition and is restored.
- Prevention of blood clot formation is mandatory. For this, various antiplatelet agents and anticoagulants are prescribed.
Treatment of dilated cardiomyopathy is daily and lifelong.
Reasons for development
The main cause of the disease is the consumption of large doses of alcohol for more than 10 years. In order for cardiomyopathy to develop, it is enough to take 100 ml of pure ethanol regularly. The pathology is detected in 50% of people with alcoholism, and in 20% of them the disease ends in death.
The disease is most often found in men over 45 years of age, but women are also susceptible to it, in whom the pathology develops more quickly. If in men it manifests itself after 10 years of regular use of ethanol, then in women it occurs after 4-5 years. The disease affects people with coronary heart disease, diabetes and hypertension.
IMPORTANT! Heart failure from alcohol intake develops faster than cirrhosis and mental disorders.
The disease is often detected among the lower socio-economic stratum, but often wealthy people who abuse alcoholic beverages receive this diagnosis. Due to the long asymptomatic period, it is difficult to detect it at the beginning of its development and begin timely treatment.
What is cardiomyopathy
The essence of selectivity is that only the heart muscle changes structurally and functionally, but the important parts of the body associated with it, for example, the coronary arteries and the valvular apparatus of the heart, do not undergo changes.
Advances in understanding the essence of cardiomyopathies were marked by the 1980 classification, which referred to the unknown origin of pathologies of the heart muscle. And only in 1996, by the decision of the international society of cardiologists, the definition of cardiomyopathies as various myocardial diseases, which are characterized by disturbances of cardiac activity, was put to rest.
The diseases are characterized by pathological changes in the myocardium, which are manifested by heart failure, arrhythmia, fatigue, swelling of the legs, and a general deterioration in the functioning of the body. There is a significant risk of developing serious heart rhythm disturbances that can be fatal.
Surgery
Sometimes the patient’s condition is so advanced that life expectancy is predicted to be no more than one year. In such situations, a heart transplant operation is possible.
More than 80% of patients tolerate this operation well; according to studies, 5-year survival is observed in 60% of patients. Some heart transplant patients live 10 years or more.
Alternative types of surgical intervention are the introduction of a cardiac casing or cardiac tie. These methods prevent further stretching of the heart.
If there is emerging valve insufficiency, annuloplasty is performed - the stretched valve ring is sutured and an artificial valve is implanted.
Surgical treatment of dilated cardiomyopathy is actively developing and new possibilities of surgical interventions are being explored.
Prognosis and complications
Death from cardiomyopathy is not uncommon. The disease is constantly progressing. It is impossible to stop the pathogenic process. If you follow your doctor's recommendations, it is possible to maintain a satisfactory condition. 5 years after diagnosis, only a third of patients remain alive. That is why it is necessary to strictly follow all the doctor’s instructions.
Cardiomyopathy often provokes myocardial infarction
Cardiomyopathy often provokes complications:
- heart failure;
- myocardial infarction;
- arrhythmias;
- swelling in the lungs.
Often the pathology leads to the formation of prolonged heart failure. Oxygen starvation occurs in the internal organs. Failure to provide immediate assistance can result in death. Myocardial infarction is an acute necrosis that occurs due to lack of oxygen. More often, the complication occurs with hypertrophic cardiomyopathy. There is a lack of vitamins and microelements in the body.
During a heart attack, the skin becomes pale. Breathing becomes difficult. There is excessive sweating. Arrhythmias are observed in almost all patients with cardiomyopathies. The complication is caused by a structural change in the tissue. The conduction process is disrupted.
Also, this pathology often causes fluid stagnation in the lungs.
Swelling in the lungs is formed due to stagnation of biological fluid - blood. Blood flow is disrupted. The amount of pumped substance decreases. The excess accumulates in the vessels of the respiratory organs. Gradually they increase.
The complication manifests itself in the form of coughing, wheezing and sputum production. Without immediate help, death occurs almost instantly. If symptoms of cardiomyopathy occur, consult a doctor immediately.
This video will tell you more about the symptoms and causes of myopathy:
Causes of cardiomyopathy (primary diseases)
This disease is often caused by:
- strong medications;
- alcohol intoxication;
- drug overdose;
- diabetes mellitus;
- trichinosis;
- various viruses;
- mucopolysaccharidosis;
- gout;
- pancreatitis;
- leukemia;
- myopathy;
- liver cirrhosis;
- hyperparathyroidism;
- malabsorption syndrome;
- sarcoidosis.
There are different forms of secondary cardiomyopathy, it is expressed as: