Elderly heart attack. Features of the flow
A heart attack in the elderly proceeds atypically and has its own characteristics, manifested by the absence of its bright emotional coloring.
1. Myocardial infarction in older people is preceded by a long history of angina pectoris. 2. It is not the anginal variant that is characteristic, but the equivalents of pain (discomfort in the left arm, the area of the scapula, the lower jaw, unpleasant sensations in the epigastric region, dizziness, weakness, and faintness are characteristic). Often, a heart attack in the elderly occurs under the “masks” of a respiratory disease, gastrointestinal diseases, or thoracic radiculitis. 3. The time of onset and duration of pain changes: delayed manifest pain syndrome - from several tens of minutes to several hours. 4. Myocardial infarction can be provoked by meteorological factors, for example, significant changes in atmospheric pressure, temperature or humidity. Also, heavy food, causing fullness and bloating of the intestines, is often a provoking factor for angina pectoris. 5. In the elderly, exacerbation of coronary insufficiency is often associated with increased blood pressure. 6. The percentage of comorbidity is high (a combination of heart attack and pneumonia, heart attack and stroke, heart attack and exacerbation of cholelithiasis). And also the development of a heart attack is often accompanied by an exacerbation of dysfunction of other organs - the stomach, intestines, and gall bladder. 7. Diabetes mellitus is often detected for the first time against the background of a heart attack in the elderly, and in the stage of decompensation. 8. Myocardial infarction is often combined with cerebrovascular insufficiency, therefore, against the background of myocardial infarction, psychoses often develop, explained by a sharp violation of cerebral circulation. 9. The painful form of myocardial infarction is often accompanied by the rapid development of acute left ventricular failure. 10. Elderly people more often develop cardiogenic shock, the mortality rate of which reaches up to 90%. 11. Myocardial infarction in old age acquires a recurrent course. 12. Up to 50% of myocardial infarctions in old age are repeated. 13. Echocardiographic signs of infarction in elderly patients differ from those in middle-aged people by a larger area of zones of hypo-/a-kinesia, more frequent registration of myocardial dyskinesia, a greater increase in the size of the heart chambers and a decrease in contractility of the heart muscle. 14. When performing coronary angiography, a multi-vessel lesion is often detected, collaterals are developed. 15. Due to the atypical clinical picture, and, accordingly, the late presentation of patients, specific revascularization of the coronary artery (thrombolytic therapy, percutaneous coronary intervention) is rarely carried out, therefore the development of post-infarction aneurysms and mechanical complications of the infarction (external and internal ruptures, ruptures, separations of the heads of papillary muscles) is typical. development of severe valvular insufficiency, high pulmonary hypertension.
Treatment of a heart attack in elderly patients also has its own characteristics: During myocardial infarction, careful and attentive care is as important as the use of medications. Relatives do not always come to see elderly patients; medical personnel have to replace the hoopoe of loved ones. Patients need mental peace, they need to be protected from anxiety. The room should be quiet. It is necessary to talk with the elderly patient and instill faith in a speedy recovery.
In the treatment of elderly patients, an important role belongs to the early gradual activation of patients in order to avoid the development of complications of bed rest (thromboembolic complications, hypostatic pneumonia, hypo-, atony of skeletal muscles, intestinal atony). Activation includes sitting down, dosed passive and active movements of the arms and legs, breathing exercises, and only then verticalization and walking. It is necessary to monitor bowel function, as constipation is often observed during bed rest. Foods that cause bloating, which negatively affects heart function, should not be given. Meals should be fractional. During the first days, urination and defecation should be done in bed. Excessive loads during defecation can lead to the development of serious life-threatening complications: myocardial ruptures, acute left ventricular failure, repeated severe anginal attacks, rhythm and conduction disturbances, thromboembolic complications, including PE. The use of systemic stimulants, synthetic and herbal, osmotic laxatives is not recommended; preference should be given to topical preparations - suppositories and microenemas, they act locally in the large intestine, the effect occurs quickly.
Features of drug therapy for hypertension in the elderly: - When carrying out analgesic therapy, one should take into account the increased sensitivity to narcotic analgesics (morphine, fentanyl), which can cause depression of the respiratory center and muscle hypotension. The drugs should be administered in fractions, under the control of respiratory rate and blood pressure. — Starting doses of drugs should be half as much as in young and middle-aged patients. — Dose titration is carried out more slowly under the control of blood pressure and heart rate, glomerular filtration rate. — Elderly patients often experience decreased liver and kidney function (which can increase the toxicity of standard doses of medications), postural (when taking an upright body position) and postprandial (caused by food intake) hypotension, as well as increased blood pressure lability. — Target SBP in elderly patients is ≤ 140 mmHg. In patients with cerebrovascular diseases (dyscirculatory encephalopathy of II-III degree, hemodynamically significant stenosis of the main arteries of the head, who have suffered a stroke or TIA), it is possible to reduce SBP to 140-150 mm Hg. – It is also necessary to take into account the lower limit of blood pressure (110-115/70-75 mm Hg), in order to avoid aggravation or development of cardiac as well as cerebral ischemia due to impaired autoregulation of cerebral vessels. In addition, some patients may have poor individual tolerance to lower blood pressure levels. — In elderly patients, it is advisable to use a staged (stepwise) scheme for lowering blood pressure. — It is necessary to monitor renal function and blood electrolyte composition, especially during treatment with diuretics and/or ACE inhibitors. — Use a simple treatment regimen (one tablet once a day) to increase adherence to treatment.
Complications
The sooner qualified assistance was provided to the patient, the fewer consequences there are.
In the post-infarction period complications arise:
- cardiogenic shock,
- pulmonary edema,
- pericarditis,
- thromboembolism,
- cardiac asthma,
- shortness of breath and swelling of the legs are signs of heart failure,
- myocardial rupture.
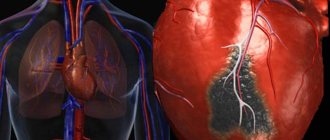
Complications are associated with the fact that with a transmural infarction, the damage involves a large part of the heart muscle.
Elderly heart attack. Features of the flow
A heart attack in the elderly proceeds atypically and has its own characteristics, manifested by the absence of its bright emotional coloring. 1. Myocardial infarction in older people is preceded by a long history of angina pectoris. 2. It is not the anginal variant that is characteristic, but the equivalents of pain (discomfort in the left arm, the area of the scapula, the lower jaw, unpleasant sensations in the epigastric region, dizziness, weakness, and faintness are characteristic). Often, a heart attack in the elderly occurs under the “masks” of a respiratory disease, gastrointestinal diseases, or thoracic radiculitis. 3. The time of onset and duration of pain changes: delayed manifest pain syndrome - from several tens of minutes to several hours. 4. Myocardial infarction can be provoked by meteorological factors, for example, significant changes in atmospheric pressure, temperature or humidity. Also, heavy food, causing fullness and bloating of the intestines, is often a provoking factor for angina pectoris. 5. In the elderly, exacerbation of coronary insufficiency is often associated with increased blood pressure. 6. The percentage of comorbidity is high (a combination of heart attack and pneumonia, heart attack and stroke, heart attack and exacerbation of cholelithiasis). And also the development of a heart attack is often accompanied by an exacerbation of dysfunction of other organs - the stomach, intestines, and gall bladder.
7. Diabetes mellitus is often detected for the first time against the background of a heart attack in the elderly, and in the stage of decompensation. 8. Myocardial infarction is often combined with cerebrovascular insufficiency, therefore, against the background of myocardial infarction, psychoses often develop, explained by a sharp violation of cerebral circulation. 9. The painful form of myocardial infarction is often accompanied by the rapid development of acute left ventricular failure. 10. Elderly people more often develop cardiogenic shock, the mortality rate of which reaches up to 90%. 11. Myocardial infarction in old age acquires a recurrent course. 12. Up to 50% of myocardial infarctions in old age are repeated. 13. Echocardiographic signs of infarction in elderly patients differ from those in middle-aged people by a larger area of zones of hypo-/a-kinesia, more frequent registration of myocardial dyskinesia, a greater increase in the size of the heart chambers and a decrease in contractility of the heart muscle. 14. When performing coronary angiography, a multi-vessel lesion is often detected, collaterals are developed. 15. Due to the atypical clinical picture, and, accordingly, the late presentation of patients, specific revascularization of the coronary artery (thrombolytic therapy, percutaneous coronary intervention) is rarely carried out, therefore the development of post-infarction aneurysms and mechanical complications of the infarction (external and internal ruptures, ruptures, separations of the heads of papillary muscles) is typical. development of severe valvular insufficiency, high pulmonary hypertension.
Treatment of a heart attack in elderly patients also has its own characteristics: During myocardial infarction, careful and attentive care is as important as the use of medications. Relatives do not always come to see elderly patients; medical personnel have to replace the hoopoe of loved ones. Patients need mental peace, they need to be protected from anxiety. The room should be quiet. It is necessary to talk with the elderly patient and instill faith in a speedy recovery.
In the treatment of elderly patients, an important role belongs to the early gradual activation of patients in order to avoid the development of complications of bed rest (thromboembolic complications, hypostatic pneumonia, hypo-, atony of skeletal muscles, intestinal atony). Activation includes sitting down, dosed passive and active movements of the arms and legs, breathing exercises, and only then verticalization and walking. It is necessary to monitor bowel function, as constipation is often observed during bed rest. Foods that cause bloating, which negatively affects heart function, should not be given. Meals should be fractional. During the first days, urination and defecation should be done in bed. Excessive loads during defecation can lead to the development of serious life-threatening complications: myocardial ruptures, acute left ventricular failure, repeated severe anginal attacks, rhythm and conduction disturbances, thromboembolic complications, including PE. The use of systemic stimulants, synthetic and herbal, osmotic laxatives is not recommended; preference should be given to topical preparations - suppositories and microenemas, they act locally in the large intestine, the effect occurs quickly.
Features of drug therapy for hypertension in the elderly: - When carrying out analgesic therapy, one should take into account the increased sensitivity to narcotic analgesics (morphine, fentanyl), which can cause depression of the respiratory center and muscle hypotension. The drugs should be administered in fractions, under the control of respiratory rate and blood pressure. — Starting doses of drugs should be half as much as in young and middle-aged patients. — Dose titration is carried out more slowly under the control of blood pressure and heart rate, glomerular filtration rate. — Elderly patients often experience decreased liver and kidney function (which can increase the toxicity of standard doses of medications), postural (when taking an upright body position) and postprandial (caused by food intake) hypotension, as well as increased blood pressure lability. — Target SBP in elderly patients is ≤ 140 mmHg. In patients with cerebrovascular diseases (dyscirculatory encephalopathy of II-III degree, hemodynamically significant stenosis of the main arteries of the head, who have suffered a stroke or TIA), it is possible to reduce SBP to 140-150 mm Hg. – It is also necessary to take into account the lower limit of blood pressure (110-115/70-75 mm Hg), in order to avoid aggravation or development of cardiac as well as cerebral ischemia due to impaired autoregulation of cerebral vessels. In addition, some patients may have poor individual tolerance to lower blood pressure levels. — In elderly patients, it is advisable to use a staged (stepwise) scheme for lowering blood pressure. — It is necessary to monitor renal function and blood electrolyte composition, especially during treatment with diuretics and/or ACE inhibitors. — Use a simple treatment regimen (one tablet once a day) to increase adherence to treatment.
Prognosis, chances of survival
With extensive myocardial infarction, the prognosis is always unfavorable. The quality and life expectancy of a person will depend on the general state of health, timeliness and completeness of medical care.
About 5% of patients die during hospitalization. Over the course of a year, 36.7% of people will be hospitalized again with a heart attack, and 9% will die (5). According to other data, the overall mortality rate from heart attack is about 30%.
Factors influencing prognosis (4).
News on the topic: myocardial infarction in the elderly
Western countries have seen a steady increase in life expectancy. There are more and more elderly people in society, and the number of people suffering from dementia is correspondingly increasing. But the drugs used to treat it can be life-threatening.
In recent years, the popularity of various dietary supplements has been growing rapidly - more and more people are taking them, especially since their choice is extremely large. Among the huge range of supplements “for all occasions”, preparations containing calcium are especially popular among older people. This element is, indeed, extremely necessary for the body of older people, as it reduces bone fragility and prevents the development of osteoporosis. However, New Zealand scientists warn that excess calcium in the body can lead to no less evil than skeletal fragility: calcium, acting on the walls of the arteries, contributes to their hardening, which increases the risk of developing myocardial infarction.
Many people get hooked on advertising and start wasting money on so-called “dietary supplements,” which turn out to be useless at best. But sometimes the passion for dietary supplements can be fraught with mortal danger. As British scientists have established, drugs containing calcium, which are often taken by older people, can provoke heart attacks. Researchers recommend getting calcium from foods rich in calcium rather than taking dietary supplements.
Many representatives of the stronger sex strive to maintain their potency in old age by resorting to testosterone preparations, the main male hormone. But this method of “increasing tone” is associated with an increased risk of heart attacks and strokes.
Fish, of course, is useful not only for pensioners, but also for people of any age. However, while phosphorus is most important for a growing child’s body, other components of hake and sturgeon are of particular importance for older people.
Scientists from the United States are warning fans of diet sodas not to get euphoric about the inscription “0 calories” on the label. Such drinks, although low in calories, however, for reasons that are still unclear, increase the risk of heart attack.
Doctors recommend that middle-aged and elderly people regularly include fatty fish in their diet, as it is good for the heart and blood vessels. However, it turned out that such fish, as well as shrimp and other seafood, also help strengthen memory.
Automatic blood pressure measuring machines can now be purchased at almost every pharmacy, but many people prefer to check their blood pressure at the clinic. Meanwhile, for some diseases, home measurements are more preferable.
Symptoms, diagnosis of AMI
There are two types of symptoms of a major heart attack:
Typical manifestations of AMI include:
- weakness;
- chest pain;
- shortness of breath;
- the pulse is usually rapid, but may be irregular;
- blood pressure may rise and then fall.
Some features distinguish chest pain in the pre-infarction state from attacks of ordinary angina:
- the pain is very intense, lasts 30-60 minutes;
- radiates to the neck, shoulder, jaw and scapula;
- does not go away after taking nitroglycerin tablets.
Atypical signs of the disease in their symptoms resemble other diseases: bronchial asthma, an attack of acute pancreatitis, stroke. Atypical pain is characterized by less severe chest pain.
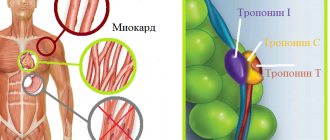
Diagnosis of AMI involves instrumental examination:
- ECG;
- Ultrasound of the heart;
- determination of myocardial infarction markers in the blood (troponin, troponin-1, CPK, AST, LDH);
- general blood analysis;
- angiography of the coronary vessels.