Causes of pain
An angina attack is a reaction of the heart muscle to oxygen deficiency. This condition develops due to atherosclerosis of the coronary vessels. Their walls become covered with plaques, the blood supply to the myocardium deteriorates, resulting in pain. This condition is a consequence of coronary heart disease.
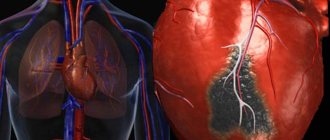
With angina pectoris, the nutrition of the heart muscle is significantly reduced. However, blood still flows through the vessels, albeit in a small volume. During a heart attack, nutrition to the heart muscle stops completely. Dead areas form on the myocardium. Therefore, a heart attack is accompanied by much more severe pain.
The following factors can trigger a heart attack:
- physical fatigue;
- emotional stress;
- smoking;
- binge eating;
- hypothermia;
- high blood pressure.
Often, the pain of angina goes away on its own during rest, when the patient is at rest. This is not uncommon in patients with cardiac ischemia. However, if pain occurs for the first time, it requires emergency care. An anginal attack is a signal from the body about a serious problem in the cardiovascular system.
In advanced cases of ischemia, pain appears not only when there is a load on the body. An attack can occur in a state of complete rest.
Causes of anginal pain
Pain in the heart area can not only be of a cardiac nature, but also signal diseases of other internal organs
As mentioned above: painful sensations are often short-term in nature, but can persist for up to several hours, causing palpitations, fear, suffocation and weakness of the human body.
All anginal pains are divided into several main groups. They can be:
- Cardiological origin, caused by problems in the circulatory system and heart disease.
- Non-cardiac diseases resulting from pathological changes in organs that are located near the heart, for example, with cervical or thoracic osteochondrosis, injury to the pectoral muscles or ribs, gastritis or ulcers, and respiratory diseases.
Pain syndrome with angina pectoris
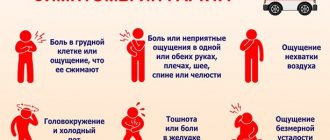
During an attack of angina, the following symptoms are observed:
- After exposure to adverse factors, a person feels severe chest pain. Patients characterize this sensation as squeezing or squeezing. Unpleasant sensations radiate to the shoulder, shoulder blade or jaw.
- A person's heart rate increases.
- The patient experiences shortness of breath.
- General health worsens. There is severe weakness and increased sweating.
The pain syndrome can last from a few seconds to several days.
In some cases, an atypical course of an anginal attack is noted. This means that the pain does not appear in the heart, but in other parts of the body:
- in the upper abdomen;
- in the hands (in particular, in the fingers);
- in the shoulder blades;
- in the neck;
- in the throat;
- in the jaw;
- in the left ear;
- in the teeth.
With atypical symptoms, the disease is very difficult to diagnose. After all, there is no pain in the heart. Typically, such attacks are observed in patients with diabetes, heart failure, and the elderly.
Some patients experience weakness in their arms and numbness in their fingers before an attack. And only after some time does pain develop.
A heart attack is not always accompanied by hypertension. It can proceed according to the collaptoid type. At the same time, the patient’s blood pressure drops sharply, weakness, nausea and dizziness appear.
Anginal myocardial infarction
Chest pain
or precordial localization, not treated with nitroglycerin; shortness of breath or suffocation; nausea and vomiting; headache; increased sweating and heart palpitations; a feeling of fear of death, less often - severe weakness, dizziness, palpitations, fever up to 38 ° C (in the first 24-48 hours), an increase in the number of leukocytes and ESR.
There are three typical types of onset of myocardial infarction:
.
Anginal status
(severe attack of St) occurs in 90% of cases. Essentially, this is a pain collapse. The cause of pain is the emerging acidic metabolites (powerful provocateurs of pain), irritating the nerve endings in the ischemic myocardium surrounding the central zone of necrosis.
Patients usually complain of prolonged substernal, strong, often unbearable, increasing, wave-like pain in the heart (in the central part of the sternum or epigastric region). One long painful attack or a series of them may occur, with each subsequent one stronger than the previous one.
Unlike ST, the pain is more intense, longer lasting (more than 30 minutes, and in a third of cases - more than 12 hours) and is not relieved by nitroglycerin. People often cannot find a place for themselves in pain, they groan and describe it in their own words, such as: “the center of the chest was squeezed in a vice,” “crushed with a reinforced concrete slab,” “a hot iron was applied to the heart.”
With a slow myocardial rupture, a “dagger pain” (“a prick in the heart”) may appear, but usually the pain is diffuse, with wide irradiation to the left arm (in 1/3 of cases), to the right arm (or both arms), less often to the neck , back, between the shoulder blades, stomach (mainly with MI of the posterior wall) and even in the lower jaw (like toothache). Pain may improve rapidly once reperfusion is restored.
symptoms may occur
. increased sweating, shortness of breath, fatigue, dizziness, fainting, as well as dyspepsia and vomiting (more often observed with lower MI). The severity of pain does not always correspond to the magnitude of MI.
There may be no pain in elderly patients, people with diabetes and after surgery. Thus, in a number of elderly patients, MI is clinically manifested not by anginal pain in the heart, but by symptoms of ALV or fainting, which are often combined with nausea or vomiting.
In 90% of young patients with myocardial infarction
the anginal status manifests itself clearly.
The pain in this case may be similar to that of pulmonary embolism, acute pericarditis, dissecting aortic aneurysm (pain radiates to the shoulder and is usually described as “tearing”). A differential diagnosis is made with these diseases.
After inadequate elimination of the anginal status, some patients may experience residual pain—an unpleasant discomfort in the depths of the chest, similar to a dull, dull pain.
Data from an objective examination of patients with myocardial infarction
(especially uncomplicated) are nonspecific in the diagnosis of this pathology. This examination is important to exclude diseases that can mimic “fresh” MI; distribution of patients according to risk level and recognition of developing AHF.
People are often agitated and tossing around in bed, looking for a position to relieve pain.
(unlike patients with TS who stand, sit or lie quietly), they often experience a feeling of fear of death.
Pallor and severe sweating (cold, sticky sweat) are revealed: if you run your hand over the forehead, it is all wet. Nausea, vomiting, and cold sensations in the extremities may occur.
In patients with CABG, the skin is cold, moist, and bluish in color; Pale complexion with severe cyanosis of the lips and nasolabial triangle may be observed.
Heart rhythm and heart rate
- important indicators of heart function.
Heart rate
may vary from marked bradycardia to tachycardia (regular or irregular) depending on the heart rhythm and the degree of LV failure. More often, the pulse is normal, but at first a tachycardia of 100-110 beats/min can be detected (a heart rate of more than 110 beats/min usually indicates extensive MI), which later slows down as the patient’s pain and anxiety subsides.
A normal rhythm usually indicates the absence of significant hemodynamic disturbances. All this occurs against the background of normal body temperature (a sign of increased tone of the sympathetic system).
Less common are arrhythmias (usually extrasystole, which occurs in almost 90% of patients) or bradycardia (usually in the first hours of lower MI), which is short-lived (then heart rate quickly normalizes).
Changes in blood pressure
also variable: with uncomplicated MI it is within normal limits; in hypertensive patients, blood pressure often increases on the first day in response to pain, excitement and fear (erectile phase of shock) to more than 160/90 mm Hg. Art. later (from the second day) it returns to normal
Many patients with myocardial infarction
manifestations of activation of the autonomic nervous system are observed. Thus, in the first 30 minutes of MI, in the case of a predominance of sympathetic tone (more often with anterior MI), an increase in blood pressure (in 10% of patients) or an increase in heart rate (in 15%), or a combination of both (in 10%) is noted. .
When parasympathetic tone predominates, on the contrary, bradycardia is determined, often associated with secondary hypotension (in 10%), or a decrease in blood pressure (in 7%), or a combination of both (in a third of patients). Sometimes (with extensive or repeated MI) blood pressure slowly (over 1-2 weeks) decreases. It drops sharply with CABG (less than 90/40 mmHg).
In general, a decrease in blood pressure (due to LV dysfunction, secondary venous congestion due to intravenous morphine, nitrates, or a combination of both) is an almost constant symptom of MI. The development of hypotension during MI is not always the result of CABG. Thus, in a number of patients with inferior MI and activation of the Bezold-Jarisch reflex, SBP may transiently fall to 90 mmHg. Art. and below.
This hypotension usually resolves spontaneously (the process can be accelerated by administration of atropine and placing the patient in the Trendelenburg position). As a person recovers, blood pressure returns to its original (pre-infarction) level.
When palpating the chest in the supine position, it is sometimes possible to identify signs of pathology of left ventricular wall movement and evaluate the properties of the apical impulse. In the left axillary region, a diffuse apical impulse or paradoxical protrusion at the end of systole can be palpated.
For uncomplicated myocardial infarction
The absence of physical cardiac symptoms during auscultation of the heart is typical; only a muting of the 1st tone can be noted (due to a decrease in myocardial contractility), the sonority of which is restored as recovery progresses. More often, physical data appear in the complicated course of extensive MI.
Muffling of the 1st tone, bifurcation of the 2nd tone can be determined (due to severe LV dysfunction and blockade of the left bundle branch); gallop rhythm (a 3rd additional sound appears in the diastole phase) due to severe dysfunction of the LV myocardium and an increase in its filling pressure (more often in patients with anterior transmural MI); transient rhythm disturbances (supraventricular and ventricular tachycardia); systolic murmur at the apex (due to mitral regurgitation due to ischemia and dysfunction of the papillary muscles or LV dilatation), occurring on the first day and disappearing after a few hours (less often, days); pericardial friction rub (in approximately 10% of all patients) along the left edge of the sternum (usually no earlier than 2-3 days from the onset of transmural MI).
Breathing rate
(RR) may increase immediately after the development of MI. In patients without symptoms of heart failure, it is a result of fear and pain. Tachypnea normalizes as the discomfort in the chest is relieved.
Symptoms of a heart attack
During an anginal attack of myocardial infarction, the pain syndrome is much more pronounced. A complete cessation of oxygen supply to the heart leads to a sharp deterioration in well-being:
- Heart pain becomes unbearable and prolonged.
- A person suffers from shortness of breath.
- The patient experiences severe fear.
- Blood pressure drops sharply.
- Cold sweat appears on the skin.
This condition is a medical emergency. Without treatment, myocardial infarction can be fatal.
Risk of atherosclerosis and heart attack:
- Sedentary lifestyle;
- Diabetes;
- Eating disorder;
- Problems with excess weight;
- Excessive consumption of strong alcoholic drinks;
- Arterial hypertension.
In addition, men over 45 years of age are at risk. It is among the stronger sex that heart attacks occur most often. The risk of this problem increases in women, mainly after 55 years.
A patient with an anginal form of myocardial infarction must be urgently hospitalized. The following specialists can save a patient’s life:
Highly qualified doctors really quickly recognize myocardial infarction. To do this, they examine the patient and listen to his complaints. The specialists will also ask the patient several clarifying questions:
To clarify the diagnosis, the patient is urgently given an electrocardiogram. This study allows you to determine myocardial infarction with 99% accuracy.
A patient with this diagnosis is urgently sent to the cardiac intensive care unit. Treatment begins with pain relief. To do this, doctors administer narcotic and non-narcotic drugs to the patient. When treating myocardial infarction, specialists usually set themselves the following goals:
- Restore blood flow;
- Limit the spread of tissue necrosis;
- Prevent complications from occurring.
To do this, the patient is required to be prescribed bed rest and medication. He is prescribed the following medications:
- Thrombolytics;
- Anticoagulants;
- Antiplatelet agents;
- Nitroglycerin;
- Beta blockers.
When a person’s condition can be stabilized, he is transferred to a hospital. Treatment lasts on average from 21 to 28 days. However, the time period may increase due to the occurrence of complications, as well as the size and location of the disease focus.
Source: https://bolezni.zdorov.online/kardiologija/infarkt-miocarda/anginoznaya-forma-infarkta-miocarda/
First aid
If a person has been suffering from cardiac ischemia for a long time and periodically experiences angina, then the discomfort can be relieved at home. It is necessary to provide first aid to the patient during an anginal attack:
- The patient needs to take a sitting position and not make sudden movements. If the attack occurs while the patient is sleeping, you should sit on the bed and dangle your legs.
- It is necessary to open the window to make it easier for the patient to breathe. Tight clothing must be unbuttoned.
Then it is necessary to give the patient drugs to relieve an anginal attack. The most commonly used drug is Nitroglycerin. You need to put the tablet under your tongue and hold it until it dissolves. This medicine usually works within 3 to 5 minutes. If the pain in the heart continues, then the drug is repeated. However, during one attack you can take no more than three tablets. If the pain does not stop, medical attention is needed.
Currently, they produce sprays for angina pectoris: “Isoket”, “Nitrominat”. One injection under the tongue is equivalent to taking one dose of medication. During an attack, the drug can be used no more than three times.
After taking nitrate medications, the patient should be given an Aspirin tablet to thin the blood. If the patient is very excited and anxious, then you should take Valocordin or Corvalol.
After providing emergency care for an anginal attack and relieving acute pain, you need to measure blood pressure and pulse. If your blood pressure is high, you should take a rapid-acting antihypertensive drug. For palpitations, the drug “Anaprilin” is indicated.
It should be remembered that Nitroglycerin and sprays cannot always be taken. If the attack occurs in a collaptoid form with a drop in blood pressure, then vasodilators are contraindicated. In this case, the following measures must be taken:
- Lay the patient down.
- Call an ambulance.
- Give an Aspirin tablet.
- To relieve pain, use analgesics: Sedalgin, Baralgin.
It is also necessary to immediately call an ambulance in the following cases:
- If the patient experiences an angina attack for the first time.
- If the pain is not relieved by taking Nitroglycerin and using sprays.
- If the attack is more severe than usual and the patient vomits.
- Urgent medical care is necessary for a prolonged anginal attack that lasts more than 15 minutes. This condition often leads to myocardial infarction.
- If the pain increases and is not relieved by medications.
Before the doctor arrives, the patient must remain in bed.
A cardiologist talks in detail about the rules of care for angina pectoris in the video.
An anginal attack is... Causes, diagnosis and treatment
An angina attack is severe pain in the heart area associated with myocardial hypoxia. This condition occurs with angina pectoris and heart attack.
Unpleasant sensations are localized behind the sternum and radiate to different parts of the body. They are of a pressing or squeezing nature. This symptom is always a sign of serious cardiac pathology.
Help in such cases should be provided immediately.
Causes of pain
An angina attack is a reaction of the heart muscle to oxygen deficiency. This condition develops due to atherosclerosis of the coronary vessels. Their walls become covered with plaques, the blood supply to the myocardium deteriorates, resulting in pain. This condition is a consequence of coronary heart disease.
With angina pectoris, the nutrition of the heart muscle is significantly reduced. However, blood still flows through the vessels, albeit in a small volume. During a heart attack, nutrition to the heart muscle stops completely. Dead areas form on the myocardium. Therefore, a heart attack is accompanied by much more severe pain.
The following factors can trigger a heart attack:
- physical fatigue;
- emotional stress;
- smoking;
- binge eating;
- hypothermia;
- high blood pressure.
Often, the pain of angina goes away on its own during rest, when the patient is at rest. This is not uncommon in patients with cardiac ischemia. However, if pain occurs for the first time, it requires emergency care. An anginal attack is a signal from the body about a serious problem in the cardiovascular system.
In advanced cases of ischemia, pain appears not only when there is a load on the body. An attack can occur in a state of complete rest.
Pain syndrome with angina pectoris
During an attack of angina, the following symptoms are observed:
- After exposure to adverse factors, a person feels severe chest pain. Patients characterize this sensation as squeezing or squeezing. Unpleasant sensations radiate to the shoulder, shoulder blade or jaw.
- A person's heart rate increases.
- The patient experiences shortness of breath.
- General health worsens. There is severe weakness and increased sweating.
The pain syndrome can last from a few seconds to several days.
In some cases, an atypical course of an anginal attack is noted. This means that the pain does not appear in the heart, but in other parts of the body:
- in the upper abdomen;
- in the hands (in particular, in the fingers);
- in the shoulder blades;
- in the neck;
- in the throat;
- in the jaw;
- in the left ear;
- in the teeth.
With atypical symptoms, the disease is very difficult to diagnose. After all, there is no pain in the heart. Typically, such attacks are observed in patients with diabetes, heart failure, and the elderly.
Some patients experience weakness in their arms and numbness in their fingers before an attack. And only after some time does pain develop.
A heart attack is not always accompanied by hypertension. It can proceed according to the collaptoid type. At the same time, the patient’s blood pressure drops sharply, weakness, nausea and dizziness appear.
Symptoms of a heart attack
During an anginal attack of myocardial infarction, the pain syndrome is much more pronounced. A complete cessation of oxygen supply to the heart leads to a sharp deterioration in well-being:
- Heart pain becomes unbearable and prolonged.
- A person suffers from shortness of breath.
- The patient experiences severe fear.
- Blood pressure drops sharply.
- Cold sweat appears on the skin.
This condition is a medical emergency. Without treatment, myocardial infarction can be fatal.
First aid
If a person has been suffering from cardiac ischemia for a long time and periodically experiences angina, then the discomfort can be relieved at home. It is necessary to provide first aid to the patient during an anginal attack:
- The patient needs to take a sitting position and not make sudden movements. If the attack occurs while the patient is sleeping, you should sit on the bed and dangle your legs.
- It is necessary to open the window to make it easier for the patient to breathe. Tight clothing must be unbuttoned.
Then it is necessary to give the patient drugs to relieve an anginal attack. The most commonly used drug is Nitroglycerin. You need to put the tablet under your tongue and hold it until it dissolves.
This medicine usually works within 3 to 5 minutes. If the pain in the heart continues, then the drug is repeated. However, during one attack you can take no more than three tablets.
If the pain does not stop, medical attention is needed.
Currently, they produce sprays for angina pectoris: “Isoket”, “Nitrominat”. One injection under the tongue is equivalent to taking one dose of medication. During an attack, the drug can be used no more than three times.
After taking nitrate medications, the patient should be given an Aspirin tablet to thin the blood. If the patient is very excited and anxious, then you should take Valocordin or Corvalol.
After providing emergency care for an anginal attack and relieving acute pain, you need to measure blood pressure and pulse. If your blood pressure is high, you should take a rapid-acting antihypertensive drug. For palpitations, the drug “Anaprilin” is indicated.
It should be remembered that Nitroglycerin and sprays cannot always be taken. If the attack occurs in a collaptoid form with a drop in blood pressure, then vasodilators are contraindicated. In this case, the following measures must be taken:
- Lay the patient down.
- Call an ambulance.
- Give an Aspirin tablet.
- To relieve pain, use analgesics: “Sedalgin”, “Baralgin”.
It is also necessary to immediately call an ambulance in the following cases:
- If the patient experiences an angina attack for the first time.
- If the pain is not relieved by taking Nitroglycerin and using sprays.
- If the attack is more severe than usual and the patient vomits.
- Urgent medical care is necessary for a prolonged anginal attack that lasts more than 15 minutes. This condition often leads to myocardial infarction.
- If the pain increases and is not relieved by medications.
Before the doctor arrives, the patient must remain in bed.
A cardiologist talks in detail about the rules of care for angina pectoris in the video.
Diagnostics
In case of a heart attack, an electrocardiographic examination is mandatory. This helps identify the signs and degree of ischemia. Additionally, ultrasound and x-ray of the myocardium are performed.
If a patient with myocardial infarction is admitted to the hospital, then therapy and diagnosis are carried out simultaneously. In this case, you cannot delay treatment.
Additionally, a blood test is performed for biochemical parameters. This allows you to determine cholesterol levels and the presence of atherosclerosis.
Further assistance to the patient is provided by the ambulance team. If necessary, the patient is admitted to the hospital. If the pain does not stop, then Nitroglycerin is taken again. At the same time, intravenous injections of analgesics are given:
- “Baralgina”.
- “Analgina.”
- "Maxigana".
To enhance the analgesic effect, antihistamines (Suprastin, Diphenhydramine) and tranquilizers (Seduxen, Relanium) are administered.
For high blood pressure, vasodilators are used. If an anginal attack proceeds according to the collaptoid type, then droppers with “Polyglukin” are placed.
Then the patient is given an ECG and, based on the results of the examination, medications are prescribed to treat ischemia.
Prevention
How to prevent a heart attack? Patients with cardiac ischemia should follow the following recommendations:
- Regularly visit a cardiologist and undergo an ECG examination.
- Take prescribed medications for ischemia.
- Monitor blood pressure levels.
- Avoid overeating.
- Eliminate bad habits.
- Maintain moderate physical activity.
- If possible, protect yourself from stress, and if necessary, take light sedatives (“Valocordin”, “Corvalol”).
These measures will help reduce the risk of anginal pain.
Source: https://FB.ru/article/385245/anginoznyiy-pristup—eto-prichinyi-diagnostika-i-lechenie
Diagnostics
In case of a heart attack, an electrocardiographic examination is mandatory. This helps identify the signs and degree of ischemia. Additionally, ultrasound and x-ray of the myocardium are performed.
If a patient with myocardial infarction is admitted to the hospital, then therapy and diagnosis are carried out simultaneously. In this case, you cannot delay treatment.
Additionally, a blood test is performed for biochemical parameters. This allows you to determine cholesterol levels and the presence of atherosclerosis.
Treatment methods
With the first symptoms of anginal status, you should begin to provide assistance to the patient at home:
- lay the patient down, loosen clothes, provide fresh air;
- give a sedative and nitroglycerin, create a positive mood for the patient;
- urgently call an ambulance to place the patient in a hospital.
The following methods of treating pathology are used in the hospital:
- restoration of blood flow in the affected areas with the help of medications;
- pain relief using potent analgesics;
- reduction of irreversible changes in the affected area with the help of anticoagulants;
- normalization of blood pressure with ACE inhibitors.
In especially severe cases, the patient is indicated for surgical intervention; its goal is to eliminate spasm of a vessel or blood clot. With the help of special techniques, the patient is able to completely restore the impaired blood flow.
Treatment
Further assistance to the patient is provided by the ambulance team. If necessary, the patient is admitted to the hospital. If the pain does not stop, then Nitroglycerin is taken again. At the same time, intravenous injections of analgesics are given:
- "Baralgina".
- "Analgina."
- "Maxigana".
To enhance the analgesic effect, antihistamines (Suprastin, Diphenhydramine) and tranquilizers (Seduxen, Relanium) are administered.
For high blood pressure, vasodilators are used. If an anginal attack occurs of the collaptoid type, then droppers with Polyglukin are given.
Then the patient is given an ECG and, based on the results of the examination, medications are prescribed to treat ischemia.
Treatment of anginal status
It is possible to alleviate the patient’s suffering by using narcotic drugs with the complex administration of other drugs:
The first drug that relieves spasm of coronary vessels and reduces the load on the left ventricle is nitroglycerin. Start taking one tablet. Directions for use: under the tongue. If the attack does not stop, you can take the drug again after 10 minutes.- The anginal form of myocardial infarction does not always stop even after the administration of narcotic drugs (morphine, promedol, fentanyl). Often, additional administration of tranquilizers (Sibazon) is required to relieve an attack.
Morphine significantly alleviates the condition, providing an analgesic as well as a sedative effect. It is enough to administer drugs to relieve the symptoms of painful shock.- In case of development of severe resistant pain symptoms, nitrous oxide is used. The product is supplied with air in the form of a 50% mixture.
- Heparin, which is used to prevent blood clots, also has an anti-shock effect. Fraxiparine is used to prevent vascular coagulation.
- Thrombolytic drugs dissolve the blood clot and relieve pain in the first hours. Altepalza is used according to strict indications: absence of bleeding, peptic ulcer, stroke. Thrombolytics are also contraindicated in the postoperative period and in acute stroke.
- Antiarrhythmic drugs, isoket and diuretics are administered according to indications.
- Oxygen has an analgesic effect, therefore, in order to relieve an anginal attack in the acute form of myocardial infarction, oxygen inhalation is sufficient. Oxygen is used when blood oxygen saturation decreases below 95%.
In a specialized department, in the first hours it is already possible to use surgical intervention, angioplasty, bypass surgery with stenting. Intensive therapy is continued until the anginal status ceases under the control of electrocardiographic monitoring.
Prevention
How to prevent a heart attack? Patients with cardiac ischemia should follow the following recommendations:
- Regularly visit a cardiologist and undergo an ECG examination.
- Take prescribed medications for ischemia.
- Monitor blood pressure levels.
- Avoid overeating.
- Eliminate bad habits.
- Maintain moderate physical activity.
- If possible, protect yourself from stress, and if necessary, take light sedatives (Valocordin, Corvalol).
These measures will help reduce the risk of anginal pain.
Causes
Men over 45 years of age are at risk for the anginal form of myocardial infarction. Women suffer from this pathology more often after 55 years.
A predisposing factor is often atherosclerosis of the coronary arteries. Plaques appear in the vessels that can block the lumen in them. The risk of this possibility increases significantly if the following factors are present:
- excess weight;
- low physical activity;
- diabetes;
- alcohol abuse;
- poor nutrition;
- arterial hypertension.
A heart attack can also occur due to a heart defect, when the coronary arteries arise abnormally from the aorta.
Causes
Men over 45 years of age are at risk for the anginal form of myocardial infarction. Women suffer from this pathology more often after 55 years.
A predisposing factor is often atherosclerosis of the coronary arteries. Plaques appear in the vessels that can block the lumen in them. The risk of this possibility increases significantly if the following factors are present:
- excess weight;
- low physical activity;
- diabetes;
- alcohol abuse;
- poor nutrition;
- arterial hypertension.
A heart attack can also occur due to a heart defect, when the coronary arteries arise abnormally from the aorta.
Cardiac anginal pain
Painful sensations of the anginal type can be of several types:
- Pain caused by any coronarogenic disturbance of the heart due to ischemic diseases (myocardial infarction, angina).
- Pain caused by one or another rheumatic or inflammatory disease, with VSD (vegetative-vascular dystonia), as well as as a result of heart disease or hypertension of arterial origin.
- Pain that occurs as a result of atherosclerosis, which provokes the appearance of circulatory disorders, and when there is insufficiency of oxygen in the myocardium, when acid accumulates in the muscle fibers, which contributes to the occurrence of pain in the chest.
Examinations and diagnostics
If pain in the heart occurs, an electrocardiogram is a mandatory test.
If anginal pain is a sign of myocardial infarction, then the patient is diagnosed and examined in conjunction with treatment, since a delay in treatment can cause complications, which is undesirable.
When interviewing the patient’s relatives and collecting anamnesis, the doctor takes special care to determine the duration of the illness and its nature. He also checks the disease's reaction to Nitroglycerin.
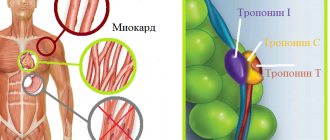
An electrocardiogram is mandatory for diagnosis, with the help of which you can find out the cause of the development of the disease. The tests include donating blood, the study of which helps to identify the presence of cardiac-specific enzymes in it, confirming the development of the disease.
If anginal pain appears due to angina pectoris, then you can eliminate it at home.
But to make an accurate diagnosis, it is best to visit a specialized doctor. During outpatient diagnostics, it is necessary to distinguish an unstable form of the disease from a stable one, and also to exclude some ailments, which include neuralgia, vasculitis, cardiac myopathy, malignant neoplasm of the pulmonary pleura and non-cardinal pathology.
The hospital uses the following diagnostic procedures for this:
In exceptional cases, a cardiac MRI may be prescribed.
First aid: features
First aid for the abdominal version of myocardial infarction is the same as for the classic anginal form of the pathology. The main problem is that the patient and his relatives rarely associate atypical symptoms with cardiac disorders. In any case, if you suspect a heart attack, you must:
- call emergency help;
- free the patient's chest from clothing, providing him with a flow of fresh air;
- comfortably sit or lay the patient down, bending his knees;
- give the patient a Nitroglycerin tablet;
- in case of delay of the ambulance team, deliver the patient to the nearest medical facility.
You can give the victim Aspirin. It is better to chew the drug - this way it will begin to act faster.
Diagnosis is complicated by the fact that nonspecific symptoms of a heart attack (fever, increased levels of neutrophils in the blood) can accompany exacerbation of chronic forms of pathologies of the digestive tract. Sometimes patients with gastralgic infarction end up on the operating table due to an erroneous diagnosis.
A special role is given to electrocardiographic research. If there is any doubt about the diagnosis, it should be done as soon as possible. Approximate information can be obtained using a hemostasiogram (blood clotting indicators). In the first hours of the development of myocardial infarction, studies of cardiac enzymes (biochemical markers of necrosis), troponin (globular protein), myoglobin (small globular protein) are indicative.
If necessary, surgical methods of therapy are indicated. One of the most effective operations is coronary artery bypass grafting. Its essence is to create a bypass path through which blood reaches the heart, bypassing the section of the vessel blocked by a thrombus.
The abdominal form of myocardial infarction does not require the use of traditional medicine - this can “blur” the symptoms of the pathology and make diagnosis even more difficult. Untimely first aid and delayed therapy can cause sudden cardiac arrest.