Note!
An ECG is often insufficiently informative in older patients or women. In most cases, such patients feel fairly mild pain, and in some there is no pain at all, which significantly complicates the diagnosis of the condition. Deviation from the standard course is also possible in the presence of dysfunction of the endocrine system.
If you doubt the exact diagnosis and need additional information, the doctor will definitely take blood to detect markers of acute myocardial infarction. This method of clarifying the condition allows you to prevent medical errors even in cases where the clinical picture is very blurred.
Markers: what are they?
Diseases of the heart and blood vessels are directly related to impaired quality of blood flow. Doctors have found that the likelihood of death due to malfunctions is higher if the patient suffers from vascular blockage, heart failure, or an abnormal rhythm of contraction of the heart muscle. It was also found that the best prognosis is for those patients who went to the hospital in time for a heart attack, and doctors were able to immediately make a correct diagnosis. A quick, accurate diagnosis and taking measures to improve the patient’s health help minimize the likelihood of complications. When clarifying the diagnosis, the blood must be checked to identify the presence of biological markers in it.
Markers of myocardial infarction in the blood are protein structures, from the concentration and state of which one can conclude how severe the patient’s condition is. The state of the markers changes over time, which also helps reveal how long ago the heart attack began. The analysis can determine whether angina pectoris is present or whether necrotic processes have begun. Consequently, the diagnosis will be made accurately, which means the treatment program will be chosen correctly.
Ultrasound of the heart (echocardiography)
Echocardiography is an instrumental method that allows one to study morphological and functional changes in the heart and its valves, as well as the volume of its cavities and the movement of blood through them. The importance of cardiac ultrasound lies not only in its ability to diagnose myocardial infarction, but also to identify possible complications. These include the following:
- heartbreak;
- thrombotic processes;
- pericarditis;
- aortic dissection;
- pulmonary embolism (PE).
Nuances of the question
Cardiac markers of myocardial infarction are highly specific and sensitive to necrotic processes occurring in the heart muscle. A sufficient number of markers for diagnosis in the circulatory system is observed as soon as pronounced symptoms of the pathological condition appear. A level sufficient to clarify the diagnosis remains for a long time.
Nowadays, doctors do not have information about the existence of some universal marker of myocardial infarction, an indicator that would provide accurate information about the patient’s condition both at the very beginning of the development of a heart attack and as it progresses. Early markers, as is known, are observed only in the first few hours after the development of a heart attack, while late ones manifest themselves after 9 hours and beyond. To clarify the diagnosis, it is necessary to analyze both groups of indicators.
Changes in blood formula and body temperature
Myocardial infarction is also characterized by changes in the blood. In clinical analysis, an increase in the number of leukocytes, that is, leukocytosis, is observed. A shift of the formula to the left and aneosinophilia may also be observed.
Severe leukocytosis is an unfavorable clinical sign.
A change in skin temperature towards its decrease can be observed with the development of acute heart failure. This phenomenon is most characteristic of the upper and lower extremities - hands and feet. However, with a large-focal location of the infarction, an increase in body temperature is observed. It is observed towards the end of the first day of the disease, remains in low-grade levels and remains thus for 3-5 days.
Biochemistry and indicators
Markers of myocardial infarction over time are the first parameter for which the blood of a patient admitted to the cardiology department is checked. In particular, myoglobin, a pigment localized in soft tissues, indicates an early process. Normally, the weight of the substance is about 18 kDa. In the first two hours of a heart attack, the concentration of this compound increases sharply, and after a day it is completely eliminated through urine. Modern technologies are such that determining the concentration of the specified pigment is possible in just 10 minutes.
It must be taken into account that myoglobin is concentrated primarily in skeletal muscles, and the concentration of this compound is determined by the efficiency of kidney function. Myoglobin gives a certain idea of necrotic processes in the heart muscle, but the data is not complete and accurate enough, so in practice it is rarely used as the main early marker of myocardial infarction.
What else do you have?
A marker of myocardial infarction is creatine phosphokinase (CPK). This substance is normally found in the muscles, so it is rarely used to determine a heart attack and only as an additional signal - the CPK parameter itself cannot give an accurate idea of the ongoing processes. Normally, CK is observed in the blood plasma 4 hours after the onset of the acute pathological condition.
You can suspect a heart attack at an early stage if tests show cardiac protein. Checking for this parameter is mandatory if a heart attack is suspected. In the presence of cardiac protein, we can confidently speak about necrotic processes in the body. Doctors clarified that the protein structure is necessary for the connection of carboxylic acids. In the heart muscle, this protein is contained in a fairly high concentration if a heart attack begins, but in a healthy state its content is much lower. The specificity of cardiac protein as a marker of myocardial damage is higher than the previously mentioned compounds.
Lab tests
Laboratory data, as well as instrumental data, are key in establishing a diagnosis.
General clinical blood and urine tests
Changes in general urine analysis are not specific for myocardial infarction. They can appear in the presence of severe complications that develop against the background of one or another cardiovascular disease, which is accompanied by kidney damage.
A general blood test for myocardial infarction reveals:
- anemia (decrease in red blood cells, hemoglobin);
- increased ESR, which indicates an inflammatory process in the body;
- leukocytosis.
Cardiac-specific markers
Cardiac-specific markers include:
- myoglobin (normalizes 24 hours after the onset of the disease);
- creatine phosphokinase MB fraction;
- lactate dehydrogenase;
- aspartate aminotransferase.
They are used to distinguish between unstable angina and small focal myocardial infarction.
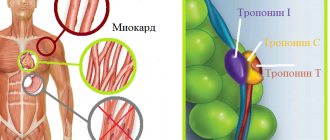
Troponin test
Troponins T and I are “fast-response” enzymes that appear in the bloodstream already in the first hours of myocardial necrosis. A negative troponin test at the onset of chest pain and after 12 hours allows one to exclude a heart attack and diagnose unstable angina in the patient.
A slight increase in troponins 6-12 hours after the onset of bleh is regarded as a clinical sign of myocardial infarction, even in the absence of ECG data and characteristic symptoms.
State progress
Later markers of myocardial damage are biochemical indicators that make it possible to clarify necrotic processes. Usually they can be detected within six hours from the onset of the pathological condition, some - later. One of the classic markers is lactate dehydrogenase (LDH). This is a cytosolic protein structure, which is currently one of the main indicators that help the doctor detect cellular damage characteristic of a heart attack. At an early stage, an analysis for LDH does not make sense, since concentrations in the circulatory system sufficient to make a diagnosis are observed quite late. The presence of LDH helps distinguish between a heart attack and angina.
Another important biochemical marker of myocardial infarction is aspartate aminotransferase. Quite high concentrations of the compound are characteristic of skeletal tissues, cardiac muscle, liver and kidneys. The necrotic susceptibility of the substance is relatively low, therefore it is not used as the main indicator in detecting a heart attack.
Differential diagnosis
Differentiation of myocardial infarction is carried out with the following diseases:
- aortic dissection;
- thromboembolism;
- acute pericarditis;
- pneumothorax;
- intercostal neuralgia;
- diseases of the gastrointestinal tract (esophagus, stomach, duodenum).
| Myocardial infarction | Angina pectoris | TELA | Pericarditis | |
| Nature of pain | Pressing, burning. May radiate to the neck, lower jaw, abdomen | Pressing, burning. There may be irradiation to the lower jaw, right and left arm, back | Dull nature of pain | Stitching, pressing pain |
| Localization of pain | Behind the sternum | Behind the sternum | Along the lateral surfaces of the chest, and in some cases - behind the sternum | Behind the sternum |
| Features of the medical history | Hereditary factor + risk factors associated with cardiovascular diseases | Hereditary factor + risk factors associated with cardiovascular diseases | Violation of the integrity of xotic structures (fractures), thrombophlebitis, malignant processes | Bacterial infections, acute respiratory viral infections and influenza |
| Additional symptoms | Shortness of breath, pale skin, tachycardia, cold and clammy sweat, dizziness and loss of consciousness, nausea and vomiting | Dyspnea | Shortness of breath, hemoptysis, vomiting, fainting | General weakness and increased pain are observed when coughing. Fever is also noted |
| ECG | The appearance of a pathological Q wave, ST segment elevation, T wave inversion | ST segment depression. In some cases, the ECG may be within normal limits | A normal ECG, but in some cases there are signs of overload of the right side of the heart | ST segment elevation |
| Other studies | Biochemical markers of myocardial infarction, scintigraphy, coronary angiography, cardiac ultrasound | Carrying out a stress ECG, coronary angiography | Ventilation-perfusion lung scintigraphy, angiopulmonography | Ultrasound of the heart |
In most cases, the diagnosis is obvious. It is confirmed by the patient’s complaints, objective examination data, laboratory and instrumental tests. Timely implementation of the necessary studies is necessary to provide the full scope of treatment and avoid the development of irreversible consequences in the heart muscle.
Nuances of analysis
As standard laboratory markers of myocardial infarction, cardiac protein structures involved in contractile processes, and especially troponins, should be noted. Due to their high specificity, the identification of these structures during analysis helps to quickly diagnose a heart attack, and therefore provide the patient with qualified care earlier. Based on the content of these structures, the doctor can predict the development of the condition and assess the patient’s chances of survival and cure.
When determining clinical myocardial infarction, it must be remembered that enzyme activity is not always explained by this particular condition, but may indicate other disturbances in the functioning of the heart, as well as non-cardiac diseases. Only a comprehensive examination makes it possible to establish an accurate diagnosis and differentiate it from conditions explained by medical interventions (certain examination methods and injected drugs). A sudden increase in the amount of enzymes is possible during thrombolytic therapy, since biologically active structures are washed out of the cardiac tissue. In order for the analyzes to be as accurate and detailed as possible, the activity of different substances should be determined over a period of time. Several research methods are known - in each clinic, doctors independently decide in favor of turning to one or another option of work.
Indicators and change over time
The earliest marker of myocardial infarction, myoglobin, increases in the first couple of hours after the attack, and reaches its highest levels after 6 hours. After a day the parameter returns to normal.
CK increases after 4 hours, the highest levels are observed after 16 hours. After two days the values return to normal.
AST is a marker of myocardial infarction, increasing after (on average) 10 hours, and reaching a maximum by the second day. By the seventh day, the indicators return to normal.
LDH reacts later than others. The enzyme is activated approximately 24 hours after the initial attack, and the highest levels are detected on average 4 days after it. Closer to the 14th day, the LDH content decreases to a stable normal value.
An analysis for CPK-MB isoenzyme, I and T troponins is required. Rapid detection of infarction is often practiced through immunological testing to determine troponin-T parameters. This protein structure is observed in the muscle fibers responsible for contraction and in the fluid inside the cells. During analyses, maximum values can usually be observed within three hours after an attack, and on the third day there is a second peak value. After 1.5-2 weeks, the value stabilizes and drops to normal.
Enzyme diagnostics of MI
Enzymatic diagnosis of myocardial infarction is based on the following enzymes and isoenzymes.
1. Main markers:
- LDH (lactate dehydrogenase);
- AST;
- CC (creatine kinase);
- Fraction MB of isoenzyme KK;
- Myoglobin;
- Troponins T and I.
2. Additional enzymes:
- MV-KK isoforms;
- Myosin light and heavy chains;
- Glycogen phosphorylase;
- Carbonic anhydrase III.
It is important to know!
The method described above for studying the patient’s condition makes it possible to determine markers of myocardial infarction, indicating not only large, but also small foci of damage. This is especially important given that doctors regularly have to work with people suffering from unstable angina - analysis of markers helps to make an accurate diagnosis and formulate a prognosis. It is known, for example, that with a normal concentration of troponin-T, up to 95% survive, and during the period of being under hospital observation, acute infarction does not occur.
To do the test, you need 150 µl of blood. The liquid is applied to the strip intended for this purpose and after 20 minutes the results are checked. During a heart attack, the protein is detected in an amount of 0.2 ng/ml or higher, that is, the strip will have two lines. With one line, the result is considered negative. To exclude an erroneous result, the study is repeated after a few hours. It is permissible to do such testing even before a person is admitted to a cardiology clinic.
Relevance of the issue
In heart diseases, the predominant percentage of deaths occurs due to acute coronary syndrome and heart failure, as well as the presence of blood clots blocking blood vessels and destabilization of the heart rhythm. Clinical myocardial infarction is minimally likely to lead to such complications if diagnosed early and accurately. The best prognosis is for a patient who goes to the clinic and receives qualified care. The approach to stabilizing the condition must be chosen individually.
To formulate the most relevant recommendations for myocardial infarction, blood is taken for analysis, during which the biochemical markers discussed above are determined. Based on the concentration indicators, one can understand what the characteristics of the pathology are in a particular case. Even if the condition is relatively mild, a heart attack requires urgent treatment, and in the future, prevention of recurrence of the situation.
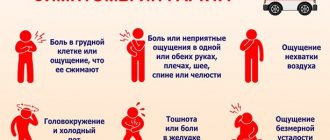
Questioning the patient
The course, form and location of myocardial infarction determine the symptoms with which the patient seeks medical help. Collecting complaints and medical history is the first thing a specialist resorts to.
The main signs of a heart attack include:
- The patient complains of chest pain. Pain syndrome can manifest itself in different ways. Some patients experience severe chest pain radiating to the left shoulder blade and arm, while others experience a painless form of the disease. This may be due to diabetes.
- Nausea, vomiting.
- Impaired consciousness (in some cases, loss of consciousness).
- Shortness of breath, the appearance of a non-productive cough.
In atypical forms of myocardial infarction, the clinical picture makes its diagnosis difficult. Differentiation from other diseases is necessary.
After providing first aid and stabilizing the patient's condition, it is important to establish risk factors for the disease and ask relatives about possible cardiovascular diseases.
Risk factors that may contribute to the development of myocardial infarction include:
- psycho-emotional stress for a long time;
- bad habits (smoking, alcohol abuse);
- arterial hypertension;
- diabetes;
- excess body weight;
- hypodynamic lifestyle;
- certain eating habits (fatty, fried, high-calorie foods);
- atherosclerotic lesions of vascular walls of various locations.
Markers: so different, but all important
It is possible to formulate adequate recommendations for myocardial infarction by assessing the state of the markers, since they are characterized by a fairly high sensitivity to necrotic processes. If symptoms increase rapidly, markers are also soon observed in the circulatory system in such quantities that an accurate diagnosis can be made. Such parameters persist for quite a long time, so doctors have enough time to determine the diagnosis.
A serious problem in medicine is the lack of information about some universal marker that would give an idea of the pathological condition both at an early stage and at a later stage. Later indicators are considered more accurate.
Problem: where and why?
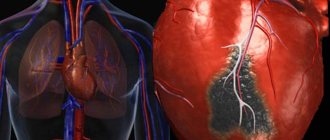
Heart attack and necrotic processes often begin due to a blood clot blocking the blood flow. A thrombus appears due to an atherosclerotic plaque. The heart muscle does not receive the necessary nutritional components, primarily oxygen, which significantly reduces vitality: on average, it is estimated at 30 minutes. If you manage to provide assistance to the patient during this period, the muscle can be saved. You can only help in intensive care, in the intensive care of the cardiology department of the clinic. In the absence of such support, tissue degeneration and necrotic processes progress and cannot be reversed. Five hours after a heart attack, the diseased area dies completely.
Clarifying the diagnosis of a heart attack in many cases is complicated by mixed symptoms and the absence of typical manifestations. The classic picture involves pain in the left side of the chest, manifestations of abnormalities on the cardiogram and the presence of biochemical markers. Clarification of the diagnosis is possible in case of disturbances in the frequency and rhythm of the heartbeat, difficulty breathing and cold sweat. Patients' skin turns pale, pain radiates to the neck, arms and hands, cramps are felt in the abdomen, and shortness of breath worries. In the absence of accurate conclusions, a biochemical blood test is required during the initial diagnosis. During such a study, it is determined exactly how severe the process is and how large the area of damage is.
Modern diagnostic methods
If there is a suspicion of a heart attack, there is anamnestic data about coronary heart disease and characteristic clinical signs, the doctor prescribes a diagnostic program. It consists of the following methods:
- electrocardiogram;
- laboratory diagnostics.
Let's take a closer look at these research methods.
An electrocardiogram is a graphic representation of the conduction of an impulse along the myocardial fibers. If conductivity is impaired due to necrosis, this will be reflected in the recording. Based on changes in the ECG, the localization of the necrosis zone can be distinguished. Also, on the graph you can see the phase of the infarction - acute or subacute.
General blood analysis
There are no specific changes observed in a general blood test and therefore a diagnosis cannot be made on its basis. During a heart attack, leukocytosis develops, which occurs several hours after the start of the process and reaches a maximum by the end of the day. The elevated level lasts for several days and gradually returns to normal. Leukocytes do not increase significantly, as, for example, with infectious pathology, which allows for differential diagnosis. This is important in case of an atypical clinical picture of myocardial infarction, when the doctor may suspect several pathologies. In a general blood test, you can also see an increased ESR, which remains this way for several weeks. Eosinophils also increase and remain elevated for about a week.
Blood chemistry
Alanine aminotransferase (ALT)
Indicator of destruction of hepatocytes and cardiomyocytes. It increases with hepatitis of various etiologies, heart attack, toxic damage to internal organs. ALT is an active component of liver metabolism, an enzyme that accelerates the metabolism of amino acids. The highest concentration of the substance is found in the cells of the liver, kidneys, heart, as well as in skeletal muscle tissue. Since its localization is the cytoplasm, it is released into the blood when the cell membrane is destroyed. The more massive the area of destruction, the higher the concentration of the enzyme in the blood. The peak activity of the enzyme during a heart attack is 12 hours.
An increase or normalization of ALT levels is a marker of the condition of patients of various profiles with diseases of internal organs and soft tissues. Depending on the disease, ALT can increase moderately or acutely, for example, the highest degree of concentration is observed in hepatitis.
In case of a heart attack, the de Ritis coefficient is used, which consists of comparing the activity of AST and ALT. If the value exceeds the norm, this indicates a heart attack, and if it is below its value, necrosis of the renal tissue or the active phase of hepatitis may have developed. Naturally, a diagnosis is not made based on the ALT indicator. For this, more specific markers are used. The level of transaminases is checked in a general biochemical analysis for differential diagnosis and monitoring of the patient’s general condition.
Aspartate aminotransferase (AST)
Marker of the condition of heart and liver tissues. Increases in viral hepatitis, toxic damage to heart tissue and hepatocytes. It is also used for preventive examination, if necessary, to confirm or exclude a heart attack. This substance is responsible for the exchange of amino acids in cells, so the largest amount is found in the cells of the liver, heart, skeletal muscles and red blood cells. If the cells of these organs are damaged, transaminase is released into the blood, where its increase can be detected. There is an acceptable level of the enzyme in the blood, because organ cells are periodically destroyed, but in pathological conditions this indicator increases several times or tens of times. The peak concentration in the blood is 12 hours after the onset of a heart attack. A comparison of ALT and AST indicators is also used. Each of these enzymes increases in certain pathologies, and during a heart attack their ratio is assessed. AST is not a specific indicator for a heart attack; it complements the overall picture of laboratory testing.
Creatine kinase MB
This substance is an isoenzyme, a marker of the condition of the heart muscle. Takes part in the metabolism of creatine and creatine phosphate. This substance is contained only in the myocardium, and therefore increases in its diseases - myocarditis, heart attack, rhabdomyolysis, pericarditis. The level of the substance is a marker during the acute and subacute phases of the process. A short-term increase in the indicator is observed during cardiac surgery, which reflects the reaction of the myocardium to treatment. The maximum concentration during a heart attack is observed 12 hours after the onset. High activity indicates a significant size of the affected area. The increase in this CPK fraction is compared with the general indicator of the substance in the body. In principle, assessment of the level of CPK MB is used for early diagnosis of myocardial damage, as well as for differentiating the condition from other diseases. An increase in the marker can indicate, in addition to a heart attack, conditions such as shock, poisoning and intoxication, infectious lesions of heart tissue.
Troponin I
A protein that is found in high quantities in skeletal muscles and myocardium. There are varieties of this protein that are responsible for different phases of muscle contraction. All these proteins are cardiac-specific and indicate the state of the myocardium. Damage to cardiac myocytes leads to the release of the substance into the blood, where it can be detected using laboratory testing. The area of necrosis affects the level of increase in troponin levels in the blood. Troponin I is the most sensitive and specific for infarction. Elevated troponin persists for 5-6 days after the onset of the pathological process.
Myoglobin
This is a protein that is found in muscle cells and contains iron molecules. Similar in structure to hemoglobin, an iron-containing blood protein. The function of myoglobin is also similar - it transports oxygen to myocytes, muscle cells. With necrosis, muscle cells are destroyed, myoglobin is released and enters the bloodstream, where it can be detected. Protein is excreted from the blood along with the kidneys. It can be detected in the blood within a few hours after the onset of the pathological process; within 2-3 days it can still be detected. This marker is one of the first to react, which increases its diagnostic value. With necrotic changes, it increases 7-10 times, depending on the area of necrosis. For comparison, the period of peak increase in other markers is 12 hours, while for myoglobin it is 6 hours. Normalization of analyzes occurs just as quickly. They can remain elevated for longer than a day if complications occur, for example, expansion of the area of necrosis. Sometimes new foci occur, then myoglobin increases again, which requires dynamic monitoring of the indicator. A negative test result is also important, which, in comparison with the clinical picture, allows one to exclude pathology. In addition to a heart attack, myoglobin may indicate long-term compartment syndrome. muscle pathologies, inflammatory processes.
How it works?
One of the indicators of a heart attack is resorption-necrosis syndrome. It is explained by the entry into the circulatory system of substances produced during aseptic necrosis. The presence of specific enzymes provokes fever and is reflected in blood tests by shifting the concentration of different components. Enzymes are released from myocytes whose life activity has come to an end. In the presence of such phenomena, to confirm a heart attack, it is necessary to take an analysis for cardiac-specific enzymes. If their level increases and correlates with the time periods identified by scientists, we can confidently speak about a heart attack.
Correct and quick clarification of the situation helps to differentiate those suffering from a heart attack from other people who have known heart pain. Markers, as is known at the modern level of development of medicine, are the most reliable way to identify a diagnosis. The information obtained in this way is more accurate than a cardiogram.
Inspection
During an external examination of a patient in whom ischemic damage to the heart muscle is suspected, the following may be observed:
- increased sweating;
- the skin and visible mucous membranes are pale;
- jugular veins are dilated;
- when palpating the chest, its increased sensitivity is noted;
- cyanosis may appear;
- restless behavior.
When measuring blood pressure, hypertension may be detected. In this case, the pulse palpable on the radial artery is threadlike, and upon auscultation, distant noises occur.
Most patients with myocardial infarction have a fourth heart sound. It appears in the late phase of ventricular diastole.
Heart attack: what are we talking about?
A heart attack is an acute pathological condition caused by a blockage of blood flow in a coronary vessel. After some time, necrotic processes begin (for the heart muscle - about 30 minutes). Areas of necrosis are called ischemia. The cells located here cannot conduct impulses, contract or function in any other way, that is, the element becomes inert, which leads to disruption of the entire organ. The larger the focus, the more important cells for life were affected, the more strongly the heart attack will affect the person’s future.
With a heart attack, there is a risk of death already in the first minutes of an acute condition, but some suffer it without consulting a doctor, and do not even suspect their illness. Specific features depend on the form. There are two main classes: small lesions and large ones. A large one is also known as a Q-infarction, since a specific wave appears on the cardiogram that is absent in a healthy person. It indicates a deep dysfunction of the cardiac structures. Sometimes this same condition is called transmural infarction, that is, a pathology in which necrosis has spread along the wall throughout its entire thickness. Full recovery, even after a long time, is impossible: a scar appears. As a rule, pathology provokes serious consequences.
A small focal infarction (non-transmural) is diagnosed when necrotic processes do not penetrate through the myocardial wall, and there is no characteristic wave on the ECG. Some patients recover completely after such a heart attack, the heart works as before the pathology. Others have consequences, but they are quite mild.
There are several options for localizing the area of necrosis: in the right or left ventricle, in the atrium. The latter is the least common, and the most typical option is damage to the left ventricle. It is possible that the integrity of one of the sections of this area or several areas may be damaged. The most dangerous is a circular infarction, that is, a condition that affects all ventricular walls at the same time.