Troponin is a special Ca2+-sensitive protein that is found in the myocardium and skeletal muscles, and is absent in smooth muscles. Its main function is to regulate the contraction of muscle fibers.
It was discovered in 1944, but the understanding of its structure and functional features, and the receipt of the name, occurred in 1965. In the presence of a sufficient amount of calcium, troponin proteins “force” the muscles to contract, and in the absence of calcium, they, on the contrary, prevent this process.
In addition, troponins prevent the formation of new “extra” vessels.
Components of myocardial troponin and its integration into actin filaments of the heart
Cardiac troponins consist of 3 parts, and those found in skeletal muscles - of 4 parts. In a person with a healthy myocardium, 95% of these proteins are in a bound state, and the remaining 5%, represented by I and T fragments, are free and located in the cell cytoplasm, while they are practically absent in the blood.
When parts of the heart muscle die or are damaged, these troponin molecules inevitably enter the blood. Today it is generally accepted that normally the upper value for T-troponin cannot exceed 0.1 ng/ml, and the upper reference value for I-troponin is <0.29 ng/ml.
Troponin test - what is it?
Troponin test is a biochemical test that detects the protein troponin in the blood.
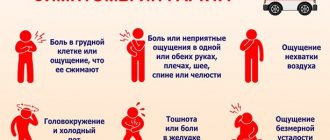
It is no secret that heart disease poses a serious threat to human life. It is important that the diagnosis of heart disease is difficult due to the identity of the symptoms.
The patient’s statement “my heart hurts” does not mean anything. And it may not even relate to heart disease specifically. But diagnosing some heart pathologies, including myocardial infarction, is extremely important due to the need for an immediate response.
Time kills. This is more important than ever for some heart diseases. Failure to take action within a short time will result in death.
Troponin - what is it?
Troponin is a highly specific marker of damage to the heart muscle (myocardium). In this regard, a troponin test is performed in cases of suspected myocardial infarction (MI), acute coronary syndromes, and unstable angina.
By their nature, troponins are small protein structures that are part of the troponin complex in striated muscles and are involved in the processes of regulating the contraction of muscle fibers. Based on their structure, troponins are divided into two types:
- troponin I;
- Troponin T.
Also secreted are troponins found in skeletal muscles and myocardium. Immunoassay methods are used to identify cardiac-specific troponins.
For reference. It should be noted that for cardiac-specific troponins the difference between their concentrations inside muscle tissue and in blood plasma is much higher than for myoglobins and many enzymes.
Due to this, the troponin test for myocardial infarction is the most accurate and sensitive test than other biochemical tests and can be used for the differential diagnosis of acute chest pain.
At the moment, laboratory diagnosis of myocardial infarction is based on detecting an increase in the level of cardiac-specific troponins I and T. An ECG is used to confirm the diagnosis.
For reference. The troponin test for a heart attack is highly sensitive not only due to the cardiac specificity of troponins, but also because the level of troponins in the blood increases significantly within 4-8 hours after the patient experiences acute chest pain.
The maximum increase in troponin levels is observed after 12-48 hours.
This makes it possible not only to use the troponin test in the early diagnosis of a heart attack, but also to monitor the severity of myocardial damage over time.
What is troponin?
Structure
Muscle tissue contains proteins responsible for the contraction of the structural and functional elements of muscles - myofibrils. These include actin and tropomyosin. The protein troponin also helps them with this. There are three types of troponins:
- troponin I;
- troponin C;
- Troponin T.
Each of them has its own role in the process of muscle contraction, but more on that later.
In laboratories, troponin may be abbreviated. For example, troponin I - TrI, troponin T - TrT.
Where is?
Troponin proteins are found in the striated muscle tissue that makes up skeletal muscles, such as the biceps and triceps. These proteins can also be found in the heart muscle. This allows troponins to be diagnostically significant indicators.
In the other type, smooth muscle tissue, there are no troponins.
What functions does it perform?
It was already mentioned above that each type of troponin plays its role in ensuring the contraction of myofibrils. Troponin T simply binds to tropomyosin, which wraps around the actin molecule. Troponin I inhibits the activity of the enzyme, as a result of which the interaction between actin and myosin does not occur. Troponin C is a protein that can bind calcium ions.
Muscle contraction requires energy in the form of ATP, as well as calcium ions.
Reduction process
When it is necessary to contract a muscle, a signal arrives through the nerve cells, resulting in the release of calcium ions in the cell. Calcium binds to the troponin C molecule. This causes other troponin molecules to be “disturbed,” which leads to a conformational change with tropomyosin. This leads to the fact that a place opens on actin (another muscle tissue protein) where the myosin molecule can interact with it. This is the beginning of muscle contraction.
Discovery History
In the sixties, a protein isolated from muscle tissue was discovered that was very similar to tropomyosin. Later it was proven that this was definitely not tropomyosin, but another muscle tissue protein. Thanks to the discovery of troponins, it has become possible to look deeper at the molecular level into the process of muscle contraction.
It was then noticed that the level of troponins specifically changes in the blood depending on various pathologies, especially when the heart muscle is damaged. Which gave impetus to using them as markers.
Features of the troponin test
Normally, the troponin test detects minimal amounts of troponins in the blood. An increase in the amount of troponins in the blood is a marker of damage to the heart muscle.
For reference. The rapid increase in the level of troponin in the blood during myocardial damage is explained by the fact that about 5% of troponins are contained in the cytoplasm of muscle cells, therefore, when the myocardium is damaged, troponins immediately enter the blood. This is precisely what allows this cardiotest to be used for early laboratory diagnosis of myocardial infarction.
The rest of the troponin in the myocardium is associated with muscle filaments, so when myocardial damage occurs, they are released into the blood gradually as damage to the heart muscle progresses.
High concentrations of troponins persist for 1-2 weeks after myocardial infarction.
It should also be noted that with successful thrombolytic therapy for a heart attack, a significant increase in troponin levels is observed (the so-called washout phenomenon). Due to this, troponin levels can also be used to monitor the effectiveness of treatment.
"Young" cardiac markers"
In the first hours from the onset of acute cardiac pathology, it is very important to correctly assess the situation and make an accurate diagnosis, because a person’s life very often depends on it. Previously, the doctor received basic information from:
- Clinical picture (severe chest pain);
- Electrocardiography (ECG) data;
- BAC – biochemical parameters (creatine kinase, lactate dehydrogenase, myoglobin, AST).
Over the last decade, relying on previous indicators (symptoms, ECG), but changing the strategy of clinical laboratory diagnostics (primarily the determination of troponin in the blood), it has become possible to recognize ischemic myocardial damage in the first hours (2 - 3 hours after the onset of signs of MI) even with minimal damage to the heart muscle. Naturally, with such an approach, the doctor gains time, begins therapeutic measures early, and thereby increases the patient’s chances of life.
In terms of specificity, methods for studying this indicator during myocardial infarction are close to 100% and noticeably prevail (if this is the first infarction) over others, also often used for damage to the heart muscle (LDH - lactate dehydrogenase, MB-CK - MB fraction of creatine kinase, myoglobin). However, with repeated MI, troponin does not react particularly well and remains at the same, albeit elevated, level, but MV-QC in this case provides the greatest amount of information.
Other cardiac markers for diagnosing myocardial infarction
For the biochemical diagnosis of infarctions, determination of the level of myoglobin and creatine kinase-MB is also often used.
Myoglobin is an oxygen-binding protein found in skeletal and cardiac muscles. The level of myoglobin in the blood increases with skeletal muscle damage and heart attacks.
Also, the level of myoglobin increases with injuries, after surgery, seizures, dermatomyositis, polymyositis, muscular dystrophy, renal failure, alcoholism, etc.
When is a troponin test performed?
Studying the level of specific cardiac markers allows us to identify destructive processes in the myocardium in patients with acute chest pain.
Due to the maximum level of accuracy and specificity, the troponin test is considered the gold standard for the biochemical diagnosis of myocardial infarction.
The troponin test allows not only to confirm or refute the presence of myocardial infarction in a patient, but also to assess the severity of myocardial damage
The study can also be used for late diagnosis of a heart attack. In cases where a patient has severe chest pain but does not go to the hospital for several days, a diagnosis of MI may be made based on elevated troponin levels.
For reference. When diagnosed early, a positive troponin test in patients with acute coronary syndrome (including cases of unstable angina) is regarded as a manifestation of severe cardiac ischemia associated with coronary thrombosis and myocardial necrosis.
High troponin levels in patients with unstable types of angina indicate an unfavorable prognosis and a maximum risk of developing a heart attack over the next 4-6 weeks.
Decoding tests
Positive troponin test
When performing a rapid test, two stripes of any intensity are interpreted as an increased Tn level.
The test data is not sufficient to make a final diagnosis; in case of a positive result, you must consult a doctor. If the result is negative after chest pain appears, it is recommended to repeat the test after a few hours.
Laboratory analysis for Tn levels is also not the basis for an accurate diagnosis, but an auxiliary marker along with ECG results, symptoms and other clinical data. In the vast majority of cases, a high level of Tn means that an MI has occurred, that is, the release of Tn was facilitated by the death of heart muscle cells.
If a patient experiences heart pain or angina attacks, but a test performed several times shows a negative result, heart damage is excluded in 95% of cases.
Indications for a troponin test
A quantitative troponin test is performed when:
- diagnosis of myocardial infarction;
- conducting differential diagnosis between cardiac and non-cardiac causes of acute chest pain;
- the need to assess the risk of myocardial infarction in patients with an attack of unstable angina;
- late diagnosis of heart attacks in patients who did not see a doctor within several days after an attack of chest pain;
- the need to choose treatment tactics in patients with acute coronary syndrome;
- the need to monitor the effectiveness of thrombolytic therapy;
- assessing the severity of necrotic myocardial damage over time.
Norm: table
Troponin levels are usually so low that they cannot be detected by most blood tests. The presence of normal TnI and TnT levels 12 hours after the onset of chest pain means that an attack is unlikely.
The normal range of values may vary slightly between laboratories. Some medical centers use different measurements, such as the troponin sensitivity test, or test different samples. In addition, some laboratories have different cutoff points for normal and probable myocardial infarction. Talk to your doctor about the meaning of the test results.
| Characteristics of the diagnosis | Normal TnT and TnI |
| Heart failure is not confirmed | <0.4 µg/l |
| Borderline state in acute MI | 2.0 µg/l |
| Heart failure cannot be ruled out (additional tests are being performed) | 0.5 – 2.3 µg/l |
| Myocardial infarction | > 2.3 µg/l |
Note! Very rarely, people who have a heart attack will have a normal reading. Some patients with elevated levels have no visible damage to the heart. Other conditions that may contribute to elevated levels include renal failure and pulmonary embolism.
Are there any contraindications to performing a troponin test?
There are no direct contraindications to performing a troponin test. However, when carrying it out, it is necessary to take into account a number of nuances that may affect the result.
The troponin test may be falsely negative if the test is performed too early (troponin levels in the blood rise within 3-4 hours after a heart attack).
Troponin levels may be elevated in:
- patients who have recently undergone cardiac surgery;
- persons with pulmonary hypertension, pulmonary embolism, hemorrhagic stroke, renal failure, severe burns, alcohol intoxication;
- persons bitten by a scorpion or poisonous snake.
Troponin test...
This laboratory test involves determining troponin in the blood:
- Tn I (TNI) – the most specific (and early) marker present in the serum from 2 – 6 hours to a week from the onset of the pathological process;
- Tn T (TNT), which can appear in the blood 3 to 4 hours from the moment of blockage of a coronary vessel and linger in the bloodstream at a level of elevated values for up to two or even three weeks.
rapid troponin test
Troponin I
The main reason for the increase in troponin I in the blood (serum, plasma), of course, is myocardial infarction. Meanwhile, there are other circumstances, by the way, not numerous, that contribute to the destruction of the troponin complex and the release of troponin I into the bloodstream, for example:
- Chronic form of ischemic heart disease;
- Traumatic injury to skeletal muscles, in which, however, the increase in TNI levels is not as significant as in myocardial infarction or even coronary artery disease.
The concentration of TNI in blood serum (in heparinized plasma this protein is 10–15% less) during myocardial infarction has a significant increase. The kinetics of release of this protein can be characterized as a two-phase curve, where the increase in concentration begins literally from 2 hours, reaches maximum values after 15 - 20 hours (1st peak), then decreases slightly, so that after 60 - 80 hours it gives a lower level than the first – 2nd peak. In other cases, there is only one peak of troponin increase (monophasic curve). Tn I returns to normal in about a week (7th day), but sometimes this process can take up to 14 days.
dynamics of the main cardiac markers during myocardial infarction
Troponin T
Since it is known that TNT is a less specific cardiac marker than the previous protein, it can be assumed that there will be several more reasons for the increase in troponin T. And this is indeed true. The range of prerequisites that create conditions for the release of Tn T (in addition to AMI) is, at least slightly, expanding:
- Unstable angina, microinfarction;
- Damage to the heart muscle after percutaneous manipulation (coronary bypass grafting, coronary angioplasty);
- Heart transplantation (increased concentration of TNT in the blood may be present for up to 3 months after transplantation);
- Myocarditis.
differences in the dynamics of troponin levels in acute MI and unstable angina
In addition, sometimes the cause of an increase in troponin T in the blood is a pathology that is not of ischemic origin:
- Traumatic heart injuries (bruises), cardiac surgery, EMB (endomyocardial biopsy - sampling of myocardial tissue for the study and diagnosis of cardiac pathology), cardioversion (electrical pulse therapy aimed at treating atrial fibrillation);
- Cardiac or renal pathology - acute and chronic failure in the stage of decompensation;
- Hypertension, hypotension, arrhythmias, severe pericarditis;
- PE (pulmonary embolism);
- Acute cerebrovascular accident (stroke);
- Acute alcohol intoxication (chronic alcoholism does not produce such abnormalities).
In rare cases, the cause of an increase in TNT is dystrophic lesions of skeletal muscles (myopathies), but for some reason atrophic changes of neurogenic origin do not increase this indicator.
Comparing the kinetics of Tn T with the movement of other enzymes under similar conditions, one can notice that it has its own characteristics and differences:
- 3-4 hours after the onset of pain, an increase in TNT in the blood is noted, which is due to the state of blood flow in the ischemic area;
- 3–4 days, the troponin level continuously rises, increasing its values 40 times or more, reaches a maximum (approximately 4 days of illness) and stops;
- At the peak of maximum values, the concentration of troponin T remains for about a week;
- After a 5-7 day plateau, the TNT content in the blood begins to slowly fall, but its level remains at elevated levels for up to 2-3 weeks.
With active and successful thrombolytic treatment, as a rule, two peaks are observed on the graph of changes in troponin T concentration (hours, days):
- The first peak appears 14 hours after ischemic myocardial damage;
- The second peak corresponds to the fourth day of AMI and has a level lower than the 1st peak.
It should be noted that troponin in the case of an uncomplicated (favorable) course of MI may show a decrease in concentration already on days 5–6 and remain elevated (by day 7) not in all patients.
Video: example of a rapid troponin test
Troponin test - instructions for use
Since the troponin test is most often performed for emergency reasons, no special preparation is required.
Attention. However, in cases where the study is carried out to assess the quality of thrombolysis and the effectiveness of treatment, it is recommended to take blood after a 4-hour fast.
At the moment, test systems have been developed that allow performing a troponin test “at the patient’s bedside”. The sensitivity and accuracy of rapid methods is comparable to the classical quantitative troponin analysis.
In this regard, a rapid troponin test has a high diagnostic value in the primary diagnosis of a heart attack.
For reference. The absence of an increase in troponin levels in patients with acute coronary syndrome makes it possible to exclude the presence of myocardial infarction with more than 90% probability.
Normally, the level of troponins in the blood is not determined or is detected in minimal quantities:
- up to 0.01 ng/ml in patients from three months to 18 years;
- up to 0.026 ng/ml in patients over 18 years of age.
In infants during the first three months of life, troponin is not detected.
Features of the troponin test
In acute coronary syndrome, the troponin test rises above 0.26-0.29 ng/ml.
During a heart attack, the troponin test rises above 2.5 ng/ml.
The troponin test is performed using immunochemiluminescence or immunochromatographic analysis. Venous blood is used for the study.
For reference. The average price of a troponin test in a laboratory is about 1,100 rubles. Test strips for performing an express test, on average, cost about 2,000 rubles.
In the laboratory, a quantitative troponin test is performed, which shows the level of troponins in the blood.
Troponin test reliability
Modern rapid tests are capable of determining the level of TnI (cardiac troponin I) in serum, plasma and whole blood preparations.
The sensitivity threshold of the test is:
- 93% when troponin levels increase to 0.1 ng/ml;
- 97% when the level of troponin in the blood increases to 0.2 ng / ml;
- almost 100% when the troponin level in the blood increases above 0.5 ng/ml.
Since the maximum level of troponin increase in the blood is observed 12-24 hours after a heart attack and persists for 7-10 days, rapid tests can also be used for late biochemical diagnosis of a heart attack.
The disadvantage of rapid qualitative tests is the inability to assess the level of troponin increase in the blood; therefore, in addition to the qualitative test, a classic quantitative test is performed.
Types of troponin
Troponins are proteins that in the human body are localized in the myocardium and skeletal muscles, responsible for cellular metabolism and contractility. These substances are heterogeneous in their structure and are represented by several modifications:
- Troponin-I (in the analysis can be designated as Tn I, Tn I, TNI) is a classic version of troponins that circulates through the bloodstream in a free state as full-fledged molecular chains and inhibits other varieties: it is present in the blood in minimal quantities, an increase in the concentration of the substance indicates usually about heart damage;
- troponin C (Tn C, Tn C, or THC) plays the role of capturing and inactivating calcium, the ions of which are extremely active and can easily penetrate cells, increasing blood pressure: the growth of the substance is dangerous for hypertensive patients, since vascular tone is disturbed and interruptions in the functioning of the heart occur;
- Troponin T (Tn T, Tn T, TNT) binds a special protein, tropomyosin, which controls the contractility of the myocardium: its presence in the blood guarantees the ability of the heart to work autonomously; with the growth of this troponin, the heart can simply stop.
Troponins I and T are predominantly localized in the myocardium, that is, they are the main cardiac markers.