general information
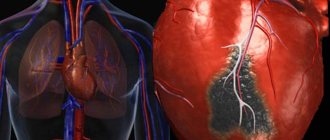
The difference between a large-focal lesion and a small-focal lesion is the size of the lesion in the coronary artery .
A small focal infarction can go completely unnoticed; it can be diagnosed several months or years after its appearance. Also, a small-focal infarction produces much fewer complications than a large lesion. A large focus of myocardial infarction indicates partial or complete death of the muscular wall of the heart . In the classification of myocardial infarction, when all the muscles of the heart are affected, it can be called transmural. The death of the heart muscles is extremely dangerous for a person, because the heart begins to contract incorrectly (that is, it does not work correctly).
Large-focal infarctions can occur independently or form from small-focal necrosis (tissue death). About 30% of all cases develop into a large-focal form. The disease is common among men because they develop atherosclerosis earlier. In women, heart attacks are common between the ages of 50 and 70 and account for about 40% of all sudden deaths.
Description of the disease
To function normally, heart cells need oxygen and nutrients. It is thanks to oxygen that the heart contracts and maintains the functioning of the circulatory system. If for some reason the cells do not receive the required amount of oxygen, they die.
A small focal infarction is characterized by the appearance of one or several areas of dead myocardial tissue. They are usually located in the back or side wall area. These damages impair heart function.
With a small-focal heart attack, small areas of the heart muscle die.
Most often, the pathology occurs in men. But over the years, the risk of violations also increases in women. Especially in old age.
Risk factors
- Bad habits (smoking, alcohol).
- High blood pressure, hypertension.
- Rheumatism affecting the membranes of the heart.
- Infectious diseases caused by streptococci, staphylococci.
- An increase in cholesterol in the blood, which forms atherosclerotic plaques.
- A significant decrease in high-density lipoprotein cholesterol in the blood, which collects “bad” cholesterol from the walls of the arteries.
- Decrease in triglyceride levels (cells take energy from it for life).
- Significant decrease in physical activity.
- Age changes, retirement age (men after 40, women after 50).
- Male gender.
- Environmental pollution in the place of residence.
- Diabetes, obesity.
- Heart diseases.
- Diseases of the immune system.
- Previously suffered small-focal and large-focal infarctions.
What are the features of the disease?
Sufficient compensation of cardiac function due to intact tissues and the absence of comorbid background (concomitant diseases) contribute to the development of an atypical “blurred” clinic and other signs of small focal infarction.
Clinical features
The formation of a necrosis zone is accompanied by the development of aseptic inflammation and the entry of mediators (biologically active substances) into the bloodstream, irritation of the autonomic nervous system.
Characteristic signs of myocardial infarction without a Q wave:
pain behind the sternum is less intense than with transmural pain. The duration of the attack is more than 20-30 minutes. The pain is poorly relieved by nitroglycerin; patients compare the symptoms with “a prolonged episode of exertional angina”;- temperature rise to subfebrile levels (up to 38°C);
- acute onset of general weakness;
- shortness of breath (frequent shallow breathing more than 20 times per minute);
- sweating, pallor or cyanosis - consequences of activation of the autonomic nervous system;
- transient arterial hypertension (increased blood pressure);
- tachycardia (rapid heartbeat).
In addition, there are atypical variants of the course of MI without a characteristic pain syndrome: asphyxial (starts with shortness of breath), abdominal (epigastric pain), arrhythmic and others.
Diagnostic features
The development of small focal infarction and diagnosis requires objective data from a clinical examination and additional research methods.
MethodSigns of small focal MI
| Electrocardiography (ECG) |
|
| General blood analysis |
|
| Laboratory markers of myocardial necrosis |
|
| Echocardiography (echo-CG) |
|
| X-ray of the chest organs |
|
| Coronary angiography |
|
The main criterion for diagnosing myocardial infarction is the results of the electrocardiogram, however, small-focal myocardial infarction on the ECG has nonspecific manifestations, therefore additional methods and consideration of clinical signs are used.
Localization of damage is carried out by the location of changes in electrocardiographic leads.
Differences in treatment approaches
A small-focal infarction does not cause significant hemodynamic disturbances in the acute stage, but a feature of the pathology is considered to be a tendency for the process to spread. Therefore, the therapeutic algorithm involves providing emergency medical care immediately after diagnosis.
Principles of treatment of small focal MI:
relief of a painful attack (narcotic analgesics), if there is no effect - intravenous administration of nitroglycerin;- oxygen therapy;
- beta blockers (atenolol, metoprolol) - drugs that lower blood pressure, heart rate with an antiarrhythmic effect;
- angiotensin-converting enzyme inhibitors (ACEIs): ramipril, enalapril. Used to prevent cardiac remodeling after a heart attack;
- anti-atherosclerotic drugs - to stabilize the plaque, which most often causes impaired blood flow.
In order to prevent the spread of the necrosis zone and the development of transmural infarction, reperfusion methods (restoration of blood flow) are used:
- thrombolytic therapy (alteplase) – drugs that dissolve blood clots in the lumen of the coronary arteries;
- balloon angioplasty - expansion of the blocked lumen using a balloon inflated under high pressure inserted through the radial artery;
- stenting – placing a metal frame in the area of a damaged vessel during endovascular intervention.
Percutaneous vascular manipulation is considered the gold standard for the diagnosis and treatment of acute coronary syndrome.
Causes
Any myocardial infarction appears as a complication due to coronary heart disease, its most acute form. The reasons can be listed in more detail:
- Ischemic disease.
- Atherosclerosis.
- Vascular thrombosis.
- Patients' blood viscosity is usually increased. This is often associated with coronary disease, but can also be an independent cause.
- Severe spasms of the arteries.
- Hypertension.
- Angina pectoris.
- A person has several risk factors.
- Nervous exhaustion, constant stress.
- Emotional turmoil.
Diagnostics
To make a diagnosis, electrocardiography is first performed. Signs of large-focal myocardial infarction on the ECG are clearly visible. Using the study, you can determine the area of ischemic damage and necrosis, and monitor changes in the myocardium depending on the period of the infarction.
Also read: How long do people stay in hospital after a heart attack? An ultrasound of the heart or echocardiography is also performed. The procedure is necessary to exclude complications of a heart attack and identify concomitant pathologies.
You can't do without coronary angiography. This is an X-ray examination using contrast. With its help, you can accurately determine where and how much the coronary artery has narrowed. This is the gold standard for diagnosing coronary heart disease. The procedure is performed to select treatment tactics.
During the study, contrast is injected into the right or left coronary arteries using an angiographic catheter. This substance fills the entire lumen of the vessel, and the doctor receives all the information about its internal relief. During the procedure, the patient is under the influence of ionizing radiation.
Diagnosis of the disease also includes a blood test. This is necessary for:
- determining the level of leukocytes;
- erythrocyte sedimentation rate;
- enzymatic activity of blood.
An electrocardiogram together with blood tests will help determine the type of infarction and the duration of necrosis.
Danger
A large lesion complicates treatment. The mortality rate from this disease in the first hours, when its most acute form passes, is no more than 40% . Damage to a large number of tissues leads to their death (necrosis). This prevents the heart from functioning normally.
Large-focal infarction is dangerous due to the appearance of an aneurysm, cardiac rupture, heart failure, thromboembolism, and ventricular fibrillation. Often, complications after such a heart attack can be complex , leading to a deterioration in the patient’s quality of life.
Consequences
Large-focal myocardial infarction leads to serious complications, therefore it has a very negative effect on the patient’s body as a whole. The consequence of any myocardial infarction is a change in heart rhythm. Some patients learn about the disease (its mild form) after undergoing an electrocardiogram (ECG).
Heart failure can occur when the heart contracts abnormally due to scarring of the myocardium because contraction function is partially lost.
If too large a scar grows , a sac-like protrusion may appear on the wall of the vessel - an aneurysm. It can only be treated surgically. If surgery is not performed, the aneurysm will burst.
conclusions
After being hospitalized for a heart attack, patients often become depressed. They begin to worry about whether they will be able to resume full physical, social, occupational and sexual activities. Large-focal infarction is indeed an extremely dangerous disease with many complications. However, this does not mean that such patients are prescribed strict bed rest for the rest of their days. Prompt provision of qualified assistance, competent cardiac rehabilitation and the patient’s conscientious attitude towards treatment are the three components of a successful recovery and the prevention of life-threatening consequences. Be healthy!
Symptoms and periods
Large focal myocardial infarction can occur suddenly or develop gradually . About half of patients report the appearance of angina pectoris. It manifests itself during emotional shocks or during physical exertion.
Acute – first two hours
- Severe chest pain radiating to the left ear.
- Severe pain in the neck, teeth and jaw.
- Pain in the collarbone and shoulder blades.
- Muscle weakness.
- Dyspnea.
- A state of panic, monstrous fear due to unbearable pain.
- Increased pressure.
- Pale skin, sweating.
- Tachycardia, arrhythmia.
Acute – first ten days
- No pain.
- Temperature.
- Symptoms of heart failure.
- Low pressure.
Subacute – first month
- No pain or fever.
- My health is gradually improving.
Post-infarction – six months
The scar is completely formed, there are no symptoms.
How dangerous is it, how is small focal myocardial infarction determined and treated?
When the area of myocardial damage is small, the infarction is called small-focal. It has a milder course and a favorable prognosis.
But due to the frequent atypical clinical picture, it is not always diagnosed on time and becomes large-focal.
A patient with a suspected heart attack must be urgently hospitalized; treatment is carried out only in a hospital setting, regardless of the size of the focus of destruction of the heart muscle.
Features of small focal myocardial infarction
Since the amount of myocardial damage in small focal necrosis is small, this type of infarction often occurs without typical anginal pain or with its equivalents (arrhythmia, suffocation, abdominal pain, dizziness, severe weakness).
An important feature is minor changes in the ECG (only the T wave or ST wave in single leads). Moreover, the positive dynamics of these deviations occurs faster than with more extensive damage to the heart.
Despite the fact that this form of cardiac muscle necrosis is generally more favorable, it may not be diagnosed in time (in about a third of patients), and then the process spreads to neighboring sections. Such a heart attack becomes large, complications arise, and the risk of death increases.
We recommend reading the article about myocardial infarction on an ECG. From it you will learn about pathology and examination, stages of heart attack, atypical forms.
And here is more information about posterobasal infarction.
Causes
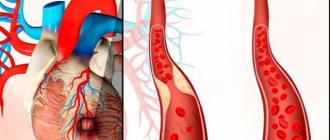
An acute form of coronary artery disease develops when a coronary artery is blocked by a thrombus; in 98% of cases it is formed when an atherosclerotic plaque is destroyed. A blood clot can form on its surface or break off, turn into an embolus and move into smaller branches with the bloodstream.
In some patients, a heart attack occurs due to spasm of the coronary vessels. An important role in the appearance of a focus of myocardial destruction belongs to the following factors:
- increased blood viscosity;
- slow blood flow;
- poor development of collateral (bypass) pathways near the ischemic zone;
- metabolic disorders in the myocardium;
- low resistance to oxygen starvation;
- deficiency of vasodilating compounds (prostaglandins, bradykinin);
- inflammatory changes in the arteries, including those of autoimmune origin.
The occurrence of acute coronary circulatory disorders is typical for patients who have predisposing conditions:
- elderly age;
- burdened heredity;
- male, but after menopause, women’s chances become almost equal;
- hypertonic disease;
- disorders of fat metabolism - dyslipidemia, increased cholesterol, obesity;
- diabetes;
- metabolic syndrome;
- constant stress;
- severe anxiety or physical stress due to angina pectoris;
- smoking, alcoholism;
- lack of physical activity.
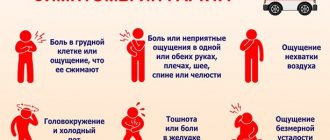
Symptoms for which you should consult a doctor
Small focal infarction most often develops against the background of unstable angina. Its symptoms may differ slightly from prolonged attacks of heart pain. In a typical case, pain occurs behind the sternum, spreads to the front of the chest, radiates to the arm, interscapular space, and the left half of the neck. Characteristics of pain syndrome:
- squeezing, stabbing or pressing sensations;
- wave-like reinforcement;
- lasts more than half an hour;
- Nitroglycerin does not relieve an attack;
- accompanied by severe weakness and sweating.
A small lesion is characterized by a less vivid clinical picture; painless or atypical forms often occur:
- localized pain in the arm, neck or thoracic spine, abdomen, forearm or hand;
- cough, shortness of breath and feeling of lack of air;
- drop in blood pressure, dizziness, fainting;
- interruptions in the heart area;
- left arm weakness, numbness or tingling.
Watch the video about myocardial infarction, its manifestations and treatment:
Classification of myocardial damage
Small-focal infarctions are most often located near the inner lining of the heart - subendocardial, less often they are inside the wall (intramural) or under the outer layer (subepicardial). The transmural variant is almost never found. They are not accompanied by the appearance of pathological Q on the ECG. By localization they are divided into:
- right ventricle;
- left ventricular (anterior, lateral and posterior);
- septal
They can appear both initially and against the background of an existing large-focal infarction.
Acute infarction and other stages on the ECG
The only sign of a small-focal lesion may be the appearance of a negative (negative) T wave and a slight decrease in the amplitude of the ventricular complex. At the earliest stages of development, an increase in ST above the isoline is detected for a short time (at the moment of intensification of pain). Such changes occur in only one or 2 - 3 leads.
With this type of disease, there is no clear focus of necrosis and pathological Q wave, so it is not always possible to judge its location from the ECG.
Since a similar ECG picture occurs with focal dystrophy of the heart muscle, to clarify the diagnosis, a study of cardiac-specific blood enzymes and indicators of acute inflammation is required.
Additional diagnostic methods
In addition to the ECG, patients are shown a laboratory blood test. The following increasing signs are typical for myocardial infarction:
- leukocytes, ESR;
- myoglobin in the first 4 hours;
- CPK-MB activity after 8 hours (analysis is carried out every 8 hours; with 3 negative results, the diagnosis of infarction is removed);
- lactate dehydrogenase on the second day and return to normal after a week;
- troponin from 4 hours to 1 - 2 weeks;
- aminotransferases (ALT and AST).
With coronary angiography, it is possible to detect blockage of the coronary artery and the degree of development of collateral blood flow pathways, and determine indications for stenting.
It must be taken into account that none of the criteria individually - typical heart pain or its analogues, changes in ECG and enzyme activity - can confirm myocardial infarction.
The diagnosis is made only on the basis of the presence of all these parameters, while normal enzyme values and ECG changes are regarded as unstable angina, and the appearance of laboratory signs in a typical or atypical clinic is considered a heart attack.
Consequences for the patient
In most cases, small-focal infarction occurs in an uncomplicated form - disturbances in the rhythm and conduction of cardiac impulses, pericarditis, pleurisy, and a less pronounced increase in temperature occur less frequently. Such damage to the heart muscle does not lead to the formation of an aneurysm or myocardial rupture, or heart failure.
However, in the absence of adequate treatment, the patients' condition worsens, the area around the source of destruction becomes electrically unstable and becomes a source of arrhythmia.
Treatment of small focal infarction
The key to a successful outcome is the earliest possible call for emergency medical care in case of a prolonged attack of angina and hospitalization of the patient if a heart attack is suspected.
First aid
At the initial stage of treatment, the patient is recommended to take sublingual Nitroglycerin (no more than 3 - 4 tablets) and 300 mg of Aspirin. If this combination is not enough to relieve an attack of pain, then Morphine or its combination with Droperidol is additionally administered intravenously.
Drug therapy in the department
After hospitalization, patients are prescribed complex treatment:
- oxygen inhalation;
- anticoagulants – Heparin, Clexane;
- nitrates – Nitroglycerin, Cardiket;
- antiplatelet agents - Aspirin, Dipyridamole, Xarelto;
- beta blockers – Egilok, Metoprolol;
- ACE inhibitors – Lisinopril, Capoten.
Diagnostics and ECG signs
Primary diagnosis is usually carried out by emergency physicians, for which an anamnesis is collected. Next, the patient is given an ECG. It clearly shows changes in heart rhythm. With a large-focal infarction, a deep Q scar appears and the R scar disappears - a pathological QS scar appears.
During the first month, the ECG chart will indicate a negative T-scar and an enlarged Q-scar . Then scar T becomes in the form of an isosceles triangle, Q is preserved.
Treatment tactics
In the most acute and acute periods, the patient is sent to intensive care . Before the ambulance arrives, the person is placed with his head on a pillow and the window is opened. A nitroglycerin tablet is placed under the tongue and he chews aspirin. Anti-anxiety medications are also given to reduce fear and panic, painkillers, Panangin, and a beta blocker (for example, metaprolol).
In the hospital, the patient is given blood thinning drugs to prevent the formation of blood clots (aspirin). Beta blockers (metaprolol, atenolol) are also prescribed, which reduce the oxygen demand of the heart muscles.
If drug therapy does not help, the patient is prescribed coronary balloon angioplasty (vasodilation) or coronary artery bypass grafting. These are two methods of surgical intervention that will save a person’s life.
Classification
The type of myocardial infarction depends on the depth of the lesion:
| Subendocardial | Damage occurs to the endocardium, that is, the inner lining of the heart muscle. |
| Subepicardial | This infarction affects the epicardium |
| Intramural | This type of myocardial infarction affects the middle ball of the heart muscle |
| Transmural | This type is considered the most severe, as it affects all three balls of the heart |
Prevention
For prevention it is necessary:
- Quit smoking and alcohol.
- Stay outdoors more. If possible, move to a suburb or city with an unpolluted environment.
- It is necessary to monitor your weight, nutrition, and blood sugar levels.
- Normalize blood pressure.
- Engage in sports, physical education, therapeutic exercises.
- Stay outdoors more.
Damage to the middle heart muscle is a dangerous disease, because slightly less than half of patients die in the first day .
This video explains first aid rules:
After rehabilitation, the patient may experience complications with the heart or any other internal organ . A heart attack can affect anyone, but to protect yourself and stay healthy for many years, you should follow preventive measures and lead a healthy lifestyle.
Source: oserdce.com
Rehabilitation after myocardial infarction
Today I want to talk to readers about such a serious complication of coronary heart disease as myocardial infarction, or rather about rehabilitation after it. This is very important, since many in our country suffer from hypertension, coronary heart disease, and cases of myocardial infarction as a result of these diseases are quite frequent.
The goal of informing patients about myocardial infarction is to reduce the incidence of complications.
Speaking about myocardial infarction, it is important to remember that in the presence of high blood pressure, constant use of antihypertensive therapy is necessary. Following this simple rule is very likely to protect you from myocardial infarction and stroke.
Rehabilitation after myocardial infarction: exercise therapy and psychologist
Exercise therapy plays a great role in the rehabilitation of the patient. If the condition is moderately severe, the patient can begin exercise therapy with the permission of the doctor and together with the instructor 2-3 days after the heart attack. And if the condition is serious, you have to wait a week.
Most often, the patient is allowed to sit on the bed on days 4-5; on day 7, you can walk a little near the bed. And only after 2-3 weeks the patient can walk from the bed to the stairs.
After some time, the distance that the patient walks increases to 500 - 1000 m with an instructor. In this case, it is necessary to carefully monitor the patient’s heart rate, blood pressure and ECG.
If there are deviations, then it is necessary to reduce the load.
If everything goes well, the patient is transferred to a special cardiological sanatorium, where he does exercise therapy, walks 5-7 km every day, receives a diet and takes medications. Also in the sanatorium there are psychologists and psychotherapists who set the patient up for a successful outcome. After hospitalization, the patient either returns to work or goes on disability.
In order to calculate training for a patient who has suffered a heart attack, it is necessary not only to take into account the severity of the condition, but also to introduce the concept of functional class for clarity.
- The first functional class is patients who have suffered a small focal myocardial infarction with minor damage
- The second functional class also includes patients who have suffered a small-focal myocardial infarction, but with complications, as well as patients who have suffered a large-focal myocardial infarction, but with minimal complications.
- The third FC is patients who have undergone small-focal MI without complications and with frequent attacks of angina (4 - 6 times a day)
- Fourth FC
- Patients with small focal infarction and serious consequences (clinical death, AV block, cardiogenic shock)
- Patients who have had transmural MI
- Patients who have undergone transmural myocardial infarction, with any complications
After conducting a velgoergometric test, patients with functional classes 1 and 2 are prescribed special training. Also, when prescribing training, the severity of the patient’s condition and the severity of coronary insufficiency are taken into account. Contraindications to training include cardiac aneurysm, arrhythmias that worsen with physical activity, and severe heart failure.
It must be remembered that during training, pain in the heart, shortness of breath, wheezing, an increase in heart size, and anxiety and depressive disorders may occur. It is necessary to monitor the patient’s heart rate, blood pressure, and ECG to prevent a recurrent heart attack.
In order for a patient to be rehabilitated in a clinic, it is necessary that the patient be of 1-2 functional class. The rehabilitation program at the clinic also includes physical therapy exercises 3 times a week, drug therapy, classes with a psychologist or psychotherapist, and the fight against bad habits. It is important to remember about walking!
Patients in the group of increased medical control are patients of FC 3-4. They need to learn how to serve themselves and move around the apartment. They have their own program at home under the supervision of a general practitioner and cardiologist. The patient does work at home, if possible, does exercise therapy from the third week and walks in the yard for an hour.
The work of a psychologist with a patient should not be underestimated, because many patients are sure that life after a heart attack is incomplete. Patients may have fears, anxiety and depressive disorders. And such beliefs have a very negative impact on the patient’s prognosis and treatment. It has been proven that a positive attitude gives hope even to hopelessly ill patients, and the capabilities of the human body are colossal!
The role of diet in rehabilitation after a heart attack
Diet therapy begins in the hospital, continues in the sanatorium and at home. It is necessary to convince the patient to quit smoking and drinking alcohol if he does so. And also normalize body weight so that cholesterol decreases and the lipid profile normalizes. And constantly, for life, use drugs that normalize blood pressure, as well as antithrombotic therapy.
Speaking about diet, it is worth noting that it is necessary to give up fried, spicy, fatty foods, limit the amount of table salt, and, when drinking liquid, give preference to clean drinking water rather than tea, coffee and soda. And, of course, do not overuse liquids so that your legs do not swell. Forget about sauces, unfortunately! Of course, limit the cakes. Try to eat small meals without overloading the body.
The main emphasis in diet therapy is the fight against excess weight, hypercholesterolemia and arterial hypertension. It is necessary to reduce body weight by no more than 3–5 kg per month. In any diet you need to adopt several principles:
- Reduce caloric intake
- Eliminate or minimize the consumption of “fast carbohydrates”, i.e. sweet
- Limit fatty foods
- The amount of table salt should be no more than 5 g per day
- Drink no more than 1.5 liters of fluid per day
- Eat little and little
This diet must be followed for life.
Sample one-day menu:
- First breakfast: boiled meat 50 g, vinaigrette with vegetable oil, tea with skim milk 200 ml
- Second breakfast: salad with seaweed 150 g
- Lunch: vegetable soup 250 ml, boiled meat with potatoes 55/150
- Afternoon snack: rose hip decoction 200, apple 100
- Dinner: baked fish with vegetable side dish 130/250 g
- At night kefir 200 ml.
Employment and disability
Patients with functional class 3-4 receive a disability group with complete exclusion of physical activity. Patients with FC 1-2 are usually transferred to light labor.
Patients after myocardial infarction are contraindicated in heavy physical labor, daily and 12-hour shifts.
Patients after a heart attack are observed in the clinic with a diagnosis of post-infarction cardiosclerosis. He can receive sanatorium-resort treatment only after a year.
Summarize. It is important for the patient and loved ones caring for him to distribute their attention to 8 points of rehabilitation after myocardial infarction. Firstly, it is moderate physical activity. You shouldn’t feel sorry for yourself, but it’s also dangerous to overdo physical labor (in the garden beds, for example).
Secondly, special attention to diet, this will become your eating style for life and will prevent other heart attacks. The third point is to avoid overwork and stress. Surround the patient with attention and positivity.
The psychologist took fourth place. If a psychologist is needed at the beginning of rehabilitation, then at home the role of a psychologist can be taken on by relatives of the patient who has suffered a heart attack. Create a collection of happy examples of life after a heart attack, stories of how the disease transformed a person’s life. Help yourself or your loved ones get the maximum benefit for the soul and self-development in the current circumstances.
If smoking and alcohol abuse were present before the heart attack, then in order to avoid repeated myocardial infarctions, it is vital to free yourself from the burden of addictions. This also includes dependence on harmful foods that lead to obesity.
I have seen how loved ones lovingly help put this into practice. A relative helped one patient quit smoking with the words: “If you smoke anyway, you won’t be able to stand it.
“This phrase hurt the man so much that for 10 years now he has not touched cigarettes, refreshing his memory of that statement. This is private, of course.
Today there is so much literature to help you get rid of addictions! It is important to understand why this is needed and go towards the goal.
The last two points are taking medications regularly and visiting a doctor for routine tests. This is something to which the patient, caring for himself and his loved ones, must strictly devote his time.
Many patients who have had a heart attack consider this event a second birth. Changing the quality of life and rethinking values made their lives better, cleaner and more conscious.
Therapist E.A. Kuznetsova
Source: https://azbyka.ru/zdorovie/reabilitaciya-posle-infarkta-miokarda
Why does heart muscle damage occur?
All pathologies of the circulatory system have several provoking factors. Against the background of a genetic predisposition and a weakened state of the body, they lead to the occurrence of necrotic processes in the myocardium.
Main risk factors:
- old age (men over 45 years old, women over 55 years old)
- bad habits (smoking, alcohol, coffee abuse, which leads to increased blood pressure)
- history of cardiovascular diseases (atherosclerosis, venous thrombosis, hypertension)
- disorders of the endocrine system (diabetes mellitus, obesity, thyroid disease)
- sedentary work, physical inactivity followed by sudden physical activity.
To make a timely diagnosis, it would be appropriate to take a general blood test to determine leukocytosis. It may be absent if a small area of the myocardium is affected, so it is worth additionally determining the level of troponin T, lactate dehydrogenase, creatine phosphokinase and myoglobin. For atherosclerosis, coronary angiography may be useful to help detect the coronary artery containing the plaque.
Reasons for appearance
The main reason for the development of the pathological process is considered to be ischemia. It occurs when the lumen of the blood vessels is blocked by a blood clot.
The risk of a heart attack increases due to the following factors:
- age-related changes in the body. The problem is diagnosed in people over 55 years of age;
- genetic predisposition;
- presence of type 1 diabetes mellitus;
- increased blood cholesterol levels;
- arterial hypertension;
- smoking;
- overweight;
- sedentary lifestyle.
People who are at risk should pay more attention to their health.
Pathological changes
Small focal myocardial infarction goes through the following stages of development:
- The sharpest. Occurs when coronary circulation ceases. It is characterized by sharp chest pain, which can radiate to the left shoulder, shoulder blade, or arm. It can last from a few minutes to a day, depending on the complexity of the lesion.
- Spicy. Passes within a week. There is a gradual death (necrosis) of a small section of the myocardium. The pain decreases. Due to the development of inflammation of the cardiac tissue, a short-term increase in temperature, leukocytosis, and an increase in ESR may be observed.
- Subacute. The inflammatory process subsides over time, and the patient's condition improves significantly. Appetite increases, and the desire for physical activity arises. The area of necrosis is replaced by connective tissue (cardiosclerosis).
- Post-infarction. Small focal myocardial infarction carries much less pathological changes. Laboratory and clinical parameters are close to normal. A number of unpleasant complications are possible, such as arrhythmias, blockades, and the development of heart failure.
Small foci of necrosis do not pose a great danger to the conduction system of the heart. Excitation spreads in the normal sequence: from the atria to the ventricles. Unlike large-focal myocardial infarction, no new elements appear on the ECG (pathological Q wave, QRS complex).
The following manifestations of cardiac muscle ischemia can be seen on the ECG:
- migration of the RST segment along the vertical axis (above or below the isoline);
- changes in the trophic T wave during ventricular repolarization (it becomes negative and pointed);
- persistence of signs of small focal infarction on the electrocardiogram for 2–4 weeks.
To avoid repeated attacks of heart attack or angina, you should adhere to preventive measures.
What happens during a small focal infarction?
The process of myocardial infarction formation
Small-focal infarction has some features in its development that distinguish it from other forms, in particular, from large-focal infarction:
- Incomplete closure of the vessel lumen
- Presence of bypass blood flow paths in the damaged area
- Blockage of small branches of the arteries that supply the heart muscle
Non-transmural infarction often develops against the background of spontaneous or drug-induced destruction of a blood clot located in the vessel. Therefore, this type is characterized by the presence in the heart muscle of damage zones of different “ages” - old and fresh. When a blood clot enters the lumen of a vessel, blood flow in this place is disrupted.
An area of the heart muscle begins to starve from lack of oxygen and “turns on” a protective mechanism - anaerobic glycolysis, in order to somehow obtain energy. However, under such conditions, acidic compounds accumulate in the myocardium (heart muscle), which “acidify” the damaged area and thereby disrupt the contractility of muscle cells. In the absence of restoration of blood flow, such an area begins to die with the formation of a necrosis zone.
Symptoms of the disease
The signs of small-focal myocardial infarction largely coincide with its large-focal form. They may be less pronounced, depending on the degree of damage to the heart muscle. Patients complain of discomfort in the heart area. Since pressing, stabbing or aching pain tends to radiate, patients in the cardiology department complain of pain in the left arm, neck or spine. Manifestations of angina pectoris may resemble intercostal neuralgia or exacerbation of osteochondrosis. A hallmark of myocardial infarction is the ineffectiveness of nitroglycerin in controlling pain. In advanced cases, unexpected cardiac arrest is possible.
In order to suspect the disease in time, you should pay attention to the following signs of small focal myocardial infarction:
- first, symptoms of general malaise occur (excessive sweating, dizziness, migraine, nausea, lack of appetite);
- the development of the inflammatory process is accompanied by leukocytosis, increased body temperature, tachycardia, and possible loss of consciousness;
- signs common to diseases of the cardiovascular system are expressed (shortness of breath after physical exertion, hypoxia of the body, fluctuations in blood pressure);
- with the development of myocardial necrosis, severe pressing pain appears behind the sternum, which can radiate to the left arm, shoulder, or under the scapula.
Since this form of myocardial infarction involves only a small area of damage, the severity of clinical symptoms can vary from minor discomfort to severe chest pain with loss of consciousness. Sometimes the patient may not experience any characteristic symptoms. In the latent form of the disease, necrosis of the heart muscle occurs unnoticed and makes itself felt when the infarction affects a large area of the myocardium. Laboratory tests for marker enzymes of damage to the heart muscle will help make a timely diagnosis.
Treatment, rehabilitation
Therapy for small focal myocardial infarction is aimed at restoring damaged tissue, eliminating the cause, preventing the development of complications and neutralizing symptoms.
What should you do during an attack?
If a person develops symptoms of a small-focal myocardial infarction, you need to immediately call an ambulance, and until it arrives, provide the patient with rest.
If possible, measure your blood pressure. If it is elevated, you can give the patient Nitroglycerin. But if you have low blood pressure, drinking this drug is strictly prohibited. To thin the blood you need to take a tablet of acetylsalicylic acid.
A patient in this condition is usually visited by fears and anxiety. In this case, give a sedative. This could be valerian tincture, hawthorn, motherwort.
Be sure to unbutton the buttons to the middle of your chest and remove any tight clothing. During a heart attack, a person needs a flow of fresh air, so open the vents and windows.
Drug therapy
After the ambulance arrives, doctors will take all necessary measures and send the patient to the hospital (cardiology department). Further treatment is carried out in a hospital setting.
After a full examination, the doctor may prescribe the following medications:
- Painkillers are selected on an individual level, depending on the pain threshold, characteristics of the patient’s body and other factors. These are mainly non-narcotic analgesics.
- In some cases, tranquilizers are used, which are aimed at eliminating nervous excitability. These are drugs such as Phenazepam or Diazepam.
- To thin the blood, accelerate blood circulation and prevent the development of thrombosis, Cardiomagnyl or Aspirin is prescribed.
- In order to quickly expand the blood vessels, which will increase the lumen in the arteries, the patient is given Tenecteplase or Alteplazau.
- Additionally, anticoagulant therapy is prescribed. These are mainly heparin drugs.
- Statins are used to remove cholesterol deposits from the body.
- To improve the functioning of the cardiovascular system, the doctor prescribes beta-blockers, antiarrhythmic drugs, ACE inhibitors and calcium antagonists.
Rehabilitation
During the recovery period, the following is recommended to speed up the healing process:
- The patient must remain in bed for some time.
- The diet is changed - the patient is prescribed a special diet that reduces the amount of salt intake. Animal fats, smoked sausages, fried and fatty foods are excluded. During this period, it is important to consume plenty of vitamins, fiber and minerals.
- The patient should do therapeutic exercises. First, under the strict supervision of a specialist, and then independently at home. The doctor will introduce you to the set of exercises.
- You will have to completely give up smoking and drinking alcoholic beverages. It is necessary to significantly reduce the consumption of coffee and strong tea. It is advisable to drink medicinal decoctions of herbs, hawthorn and rose hips.
- Throughout your life you need to avoid stressful situations and monitor your blood cholesterol levels.
After a small-focal myocardial infarction, it is important to undergo a rehabilitation course in a medical institution. The recovery period will continue at home. The duration of rehabilitation depends on the form of the pathology, the course of the disease and the severity.
To learn how rehabilitation after a heart attack is carried out and why it is needed, watch our video:
How to avoid negative consequences
Actually, small-focal myocardial necrosis rarely causes serious complications in the functioning of the cardiovascular system. Much more dangerous is its transition to a large-focal form of the disease. To avoid the development of further necrosis, it is necessary to reduce the load on the heart muscle with the help of cardiotonic medications. They lower blood pressure, reduce heart rate, and protect against oxidative processes.
Common cardiotonics include:
- cardiac glycosides (“Strophanthin K”, “Korglikon”, “Digoxin”);
- non-glycoside cardiotonic drugs (“Dobutamine”, “Dopamine”, “Milrinone”).
Primary small-focal infarction in most cases proceeds favorably. For some time after the attack, negative consequences in the form of heart rhythm disturbances (for example, ventricular fibrillation) are possible. Sometimes they persist, requiring additional treatment with antiarrhythmic drugs.
Heart rate stabilizers are divided into:
- membrane-stabilizing drugs (“Quinidine”, “Novocainamide”, “Aymalin”, “Ritmonorm”);
- beta-blockers (“Anaprilin”, “Metproprolol”, “Atenolol”);
- potassium channel blockers ("Amiodarone");
- calcium channel blockers (Verapamil, Diltiazem);
- potassium preparations (potassium chloride, Panangin).
Treatment methods aimed at keeping the heart muscle healthy consist of stopping necrotic processes, eliminating negative consequences and preventing further development of necrosis. Small-focal myocardial infarction, if preventive measures are not followed, can develop into a large-focal form of the disease. Other complications include: cardiac aneurysm, thromboembolism, cardiac arrhythmia, cardiogenic shock, heart failure.
Source: sosudoff.ru
Prognosis and rehabilitation
Life after suffering a large-focal heart attack may never return to normal. Recovery after an illness should be long-term and gradual. Preventive measures can extend a person’s life for many more years.
Recovery lasts throughout the post-infarction period. At this time, emotional peace and adherence to preventive measures against complications are recommended.
Quality of life depends on the area of tissue necrosis, complications encountered and the response of medical workers.
Large focal necrotic changes in the heart muscles lead to death in half of all cases. However, with a timely visit to the clinic, adequate treatment and the patient completing all rehabilitation measures, the prognosis can be favorable.
After a large-focal myocardial infarction, complications may occur, conditionally divided into two groups:
- Early manifestation of consequences: acute heart failure, cardiogenic shock, arrhythmia, tachycardia, ruptures of the heart walls.
- Late manifestation of complications: chronic heart failure, aneurysms in the myocardial cardiac muscles, thromboembolism.
Large-focal myocardial infarction is a dangerous disease that in many cases leads to death. To prevent it, it is very important to lead a healthy lifestyle, get rid of chronic pathologies in a timely manner, pay attention to the slightest symptoms of cardiovascular system disorders and undergo annual preventive examinations with a doctor.
Blood pressure in a person having a heart attack
Heart disease is one of the main problems of our time. Blood pressure changes radically during myocardial infarction, which leads to the need for medical intervention to prevent harmful consequences. During normal functioning, the myocardial muscle transports the required amount of blood to the organs, but before the attack there is a state of oxygen starvation. To prevent an attack and return to a normal way of life, you need to understand the origins and follow preventive measures.
Causes of the disease
Myocardial infarction is a pathological disorder of the heart muscle caused by a discrepancy between the organ’s need for oxygen and the rate of its delivery. Necrosis of muscle tissue subsequently develops. In men, the development of heart attacks is observed more often; in women, the tendency appears after the onset of menopause. The most common factors leading to a heart attack include:
- Gender specificity. Men are more prone to heart attacks.
- Climax. During the period of restructuring of the body, a failure in blood pressure and weight gain occur. A combination of factors can cause a heart attack.
- Hereditary predisposition.
- Excess cholesterol.
- Use of tobacco products.
- Overweight.
- Psycho-emotional stress.
- Frequent increases in blood pressure above 145/90.
- Diabetes.
Return to contents
Symptoms of pathology
Myocardial infarction leads to disturbances in the functioning of the entire cardiovascular system and threatens the life of the patient.
Myocardial infarction is characterized by a sharp, prolonged pain that does not go away even after the use of heart medications, increased excitability, and fear of dying. Pain can be felt in the arms, in the neck, lower jaw, it can also be bursting, squeezing, burning, squeezing. Under certain circumstances, myocardial infarction can be painless. Characteristic symptoms are: shortness of breath, lightheadedness, abdominal pain, periodic loss of consciousness, decreased blood pressure. There are these types of heart attack depending on the symptoms:
on
| Name | Description |
| Typical | All the above mentioned signs are characteristic. The most commonly reported type of heart attack. |
| Gastralgic | The first symptom is abdominal pain. |
| Asthmatic | It manifests itself as a feeling of suffocation, masking pain in the posterior chest. |
| Arrhythmic | Caused by a severe heart rhythm disorder that can be fatal. |
| Cerebral | The symptoms inherent in a stroke are concerning; in severe cases, there is a high risk of developing cardiogenic shock. |
| Asymptomatic | There are no characteristic signs. |
Return to contents
Why is high blood pressure one of the signs of the disease?
High blood pressure negatively affects a person's cardiovascular system.
With hypertension, blood pressure often rises above 140/90 for a long period of time, which leads to the risk of developing cardiovascular diseases, which are the causes of heart attacks. High blood pressure increases the load on the heart, which has to pump blood under increased pressure. This causes an increase in cardiac muscle mass, which leads to an increased need for oxygen. The consequences are ischemic pathology, which, together with other unfavorable factors, leads to myocardial infarction. Increased cardiac pressure during myocardial infarction leads to complex consequences.
Return to contents
Low pressure
Elevated blood pressure is recorded only on the first day; then the person’s blood pressure decreases. The pulse during myocardial infarction is recorded within 55-60 beats. If it is clearly visible that the pulse rate begins to increase, then these are signs of disease progression. Cardiogenic shock often becomes a complication of the disease; its characteristic signs are:
- acute lack of blood supply;
- decreased blood pressure;
- decreased heart rate;
- numbness of the limbs.
Heart pain is a consequence of myocardial infarction.
Often, blood pressure drops and no longer rises to the previous level. This is associated with cardiac and vascular disorders. It happens that after a stroke in hypertensive patients, blood pressure normalizes; this is considered a positive consequence after the disease. Low blood pressure after myocardial infarction causes the following consequences:
- weather dependence (well-being depends on weather changes);
- fatigue (in the evening energy drops);
- lack of air (cause of yawning);
- throbbing pain in the temporal lobes and the back of the head (similar to migraine pain, causing nausea and vomiting);
- coldness of the extremities (numbness and increased sensitivity to temperature changes);
- dizziness (disturbs in the morning when getting out of bed);
- painful discomfort in the heart or in the back of the chest (caused by decreased vascular tone);
- memory impairment (depressive state, psycho-emotional instability).
Return to contents
First aid
An important step is to call emergency services. If there are symptoms of disease development or acute pain, you must immediately take a Nitroglycerin tablet; if necessary, the tablet is taken again. It is forbidden to reduce the pressure; in case of a heart attack, sharply reduced pressure will lead to harmful consequences. In an acute attack, loss of consciousness, respiratory arrest, loss of heart rate are observed, and emergency assistance is required.
Return to contents
What to do when treating the disease?
At the first symptoms of a heart attack, you must urgently call an ambulance.
At the first symptomatic manifestations, the patient must be sent to the hospital. Timely provision of medication can help the blood clot dissolve and restore blood flow. After this, preventive treatment is carried out to prevent thrombosis formation. However, more often the patient will need to undergo surgery. First, after an attack, treatment should be carried out under the supervision of specialists, strict bed rest is prescribed, since even minimal stress can be dangerous.
The recovery period lasts several months. As a result of a heart attack, heart failure and a number of other complications may occur. The consequences of the attack and the return to normal levels depend on the speed of medical care. The physical activity of the body increases gradually; patients are advised to reconsider their rhythm of life. The pills prescribed by your doctor must be taken throughout your life to maintain cardiac activity.
Return to contents
Measures to prevent blood pressure during a heart attack
Many people wonder why a heart attack occurred after an attack, but it is necessary to take care of their health in advance. To prevent an attack, experts recommend leading a healthy, active lifestyle, eating a healthy diet, and giving up bad habits. Excess weight, diabetes, high blood pressure, and excess cholesterol contribute to the development of pathology. In this case, it is necessary to purchase a tonometer, keep a journal and systematically monitor pressure readings. There is a need for strict adherence to preventive rules:
- It is worth maintaining the pressure level at around 90-140 mm Hg. st;
- if you are overweight, the permissible weight limit is determined and the process of losing weight begins;
- get rid of bad habits;
- increase active lifestyle;
- limit stressful situations;
- normalize your daily routine.
Return to contents
Blood pressure monitoring for preventive purposes
One of the main preventive measures is blood pressure control. If the pressure has dropped, this means unscrupulous implementation of medical recommendations. If your blood pressure is low, it is recommended to drink strong coffee or tea and rest for a while. Ginseng extract increases low blood pressure, but if the measures taken do not help, you need to call a first aid team in order to provide emergency assistance in a timely manner and prevent the development of a heart attack.
In the modern world, due to frequent stress and overexertion, people have problems with the cardiovascular system, a type of which is a heart attack. The causes of the disease have a variety of origins; it may be a genetic predisposition or an unhealthy lifestyle. One of the key roles is played by blood pressure, the indicators of which change during the attack and after it. To prevent the development or recurrence of an attack, you must follow the recommendations prescribed by your doctor, lead a healthy lifestyle and avoid stressful situations.
Rehabilitation after small focal myocardial infarction
Small focal myocardial infarction is characterized by a weak clinical picture.
As a rule, it occurs with coronary heart disease with small foci of muscle necrosis. According to medical statistics, small-focal lesions appear in 20% of patients with myocardial infarction. Sometimes this disease is regarded as a pre-infarction period. It means that a mild form of pathology has developed into a large-focal myocardial infarction.
What kind of disease is this and how does it appear?
All cells of the human body need oxygen, and heart tissue is no exception. It is needed for organs to function properly and receive energy. The heart needs oxygen to contract in order to pump blood well. This supports the functioning of the circulatory system. If a cell does not receive oxygen for certain reasons, it dies.
Small focal myocardial infarction is one area (or several) of necrosis of the heart muscle, for example, in the posterior or lateral wall.
This problem causes disruption of the functioning of the most important organ of the human body.
The area of damage during the development of pathological processes depends on the size of the vessel. Small-focal myocardial infarction causes small areas of cardiac tissue of the lateral or posterior wall to die.
Most often, the provocateur of the disease is fatty plaques. They form in the lumen of blood vessels, block it, which leads to the appearance of atherosclerosis.
Men are more likely to get sick, since as a result of poor nutrition and predisposition, they have a higher risk of developing pathology. Sometimes the cause of the development of the disease can be vascular spasms, but the disturbances quickly pass.
Clinical picture
If a patient develops small-focal vascular lesions, he is primarily concerned about heart pain. It can be different, for example, squeezing or pressing, piercing or cutting. Many patients indicate that the pain is not constantly present, it either becomes weak or worsens again. At the same time, the patient panics and fears that he may die.
Pain with small-focal tissue lesions is not as severe as it happens during extensive or large-focal pathology. Patients complain of pain in the back, left shoulder, arm, teeth or jaw . And a medicine such as nitroglycerin, which is taken for angina or functional disorders, does not help reduce pain.
In addition, there are other signs indicating the occurrence of small focal necrosis:
- increased body temperature;
- cardiopalmus;
- high pulse;
- general weakness;
- headache;
- pale skin;
- frequent sweating.
If these symptoms appear, you should immediately consult a doctor or call an ambulance. The sooner a specialist makes an accurate diagnosis, the sooner effective treatment will be prescribed. The patient will have a greater chance of undergoing therapy without consequences and recovery.
Important! If there is chest pain that is not relieved by nitroglycerin, and at the same time there is a fear of death, a strong heartbeat and an increase in body temperature, you should immediately call an ambulance.
Classification of the disease
The type of small focal cell necrosis is determined by the depth of damage to the heart tissue. Medicine distinguishes 4 types of this disease:
- Subendocardial. Inside the heart there is a connective tissue membrane - the endocardium. If its blood vessels are affected, necrosis occurs.
- Subepicardial. A form of small-focal myocardial infarction, which develops when blood vessels are damaged in the area of the outer serous membrane of the heart.
- Intramural. In this case, the disturbances cause necrosis to affect the middle layer of the heart.
- Transmural. The most severe form of small focal necrosis. As a result of the development of pathological processes, all 3 layers of the heart muscle suffer.
Medicine provides not only a general classification of the disease. There are also stages of pathological processes:
- The sharpest. A heart attack develops as soon as blood flow stops. Against the background of ischemia, necrosis appears. The main symptom of the critical stage of development is severe pain. It disturbs the patient for 30 minutes or a day, and can last for a long time.
- Acute small focal infarction is accompanied by necrosis, tissue softening, and inflammation. As a rule, the pain decreases, since the area affected by the pathology is already lifeless. But the inflammatory process can continue and cause an increase in body temperature. The duration of this state is 10 days.
- Subacute stage of infarction. Most patients have no complaints during this period, their condition is normal. As a rule, at this stage, necrosis is replaced by scar tissue.
- Post-infarction. The patient is completely free of symptoms and complaints. In addition, there are no changes in laboratory tests.
Depending on how often disorders occur, experts distinguish the following forms of small focal infarction:
- Primary. If the patient did not have heart problems before this incident.
- Recurrent. Heart attack occurring during the first attack within 8 months.
- Repeated. When the disease returned after 8 months.
Considering the location of the disease, doctors distinguish infarction of the right and left ventricles, as well as the interventricular septum.
Diagnostic methods
During diagnostic procedures, doctors try to detect changes in the T wave and ST segment on the ECG.
With large-focal vascular damage, a large area of the organ dies. In this case, impulses are not conducted, so a pathological Q is formed.
Against the background of a small-focal infarction, small areas of necrosis are formed that do not interfere with the passage of the impulse. Thus, pathological Q is not observed.
- There are no QRS changes.
- R wave height is lower compared to previous study results.
- The ST segment may be located above or below the isoline.
- The T wave may be negative, deep, jagged, or double-humped.
Medicine provides additional methods for diagnosing small focal lesions:
- a general blood test that will show the presence of an inflammatory process;
- determination of the amount of myoglobin;
- measurement of creatine phosphokinase (CPK) level;
- assessment of lactate dehydrogenase activity;
- Troponin T test.
A procedure such as cardiac ECHO allows you to identify areas that contract poorly or do not contract at all. Coronary angiography is performed to determine the artery in which plaque has formed.
Treatment
Therapy is carried out exclusively in inpatient settings, in specialized medical institutions with a cardiology department and intensive care wards.
- Patients are prescribed bed rest, which must be strictly observed.
- The patient's diet during treatment should be fortified and gentle.
- Since the main symptom of a heart attack is pain, doctors prescribe special medications to eliminate it, usually non-narcotic analgesics.
- To prevent serious disorders and consequences, experts prescribe antiarrhythmic drugs, beta receptor blockers, and calcium antagonists to patients.
- Treatment of small focal myocardial infarction helps prevent and eliminate arrhythmia, heart failure, and cardiogenic shock. The patient is prescribed magnesia, nitrates and antispasmodic drugs.
Overweight patients need to lose extra pounds. To do this, you can do walking and exercise . Statins can help reduce cholesterol. In addition, patients should take nitroglycerin.
Prevention and prognosis
Fine-focal vascular lesions are serious disorders that are accompanied by dangerous complications. Most deaths occur within the first 24 hours after the attack.
The work of the heart depends on the location of the foci and the volume of the infarction zone. If there is damage to more than 50% of the tissues, its work is impossible, as a result the patient experiences cardiogenic shock and the patient dies.
Against the background of minor vascular lesions, the heart may also not be able to cope with the load. In such a situation, the patient experiences heart failure. If the acute period passes without complications, doctors give a positive prognosis for the patient’s recovery.
Rehabilitation after a small focal myocardial infarction requires adherence to strict rules:
- Healthy and active lifestyle.
- Give up any bad habits. This primarily applies to tobacco and alcoholic beverages.
- Nutrition should be healthy and balanced.
- Excessive physical and psychological stress is contraindicated.
- In addition, doctors recommend that patients monitor their blood pressure and control their blood cholesterol levels.
Despite the mild clinical picture and minor changes on the ECG, small focal myocardial infarction is a serious disease. Even with mild pain in the heart, you should consult a doctor. Otherwise, small focal vascular lesions may occur.
source
Rehabilitation after myocardial infarction
Today I want to talk to readers about such a serious complication of coronary heart disease as myocardial infarction, or rather about rehabilitation after it. This is very important, since many in our country suffer from hypertension, coronary heart disease, and cases of myocardial infarction as a result of these diseases are quite frequent.
The goal of informing patients about myocardial infarction is to reduce the incidence of complications.
Speaking about myocardial infarction, it is important to remember that in the presence of high blood pressure, constant use of antihypertensive therapy is necessary. Following this simple rule is very likely to protect you from myocardial infarction and stroke.
Forms of heart attack. Something that not everyone knows about
I think everyone knows that it is necessary not only to monitor blood pressure and take medications that lower blood pressure regularly, but also to stop attacks of angina pectoris. The forms of heart attack deserve special attention; this is really worth knowing and remembering.
- B painless form of myocardial infarction. This form of myocardial infarction occurs with severe sclerosis of the coronary arteries. In the absence of obvious burning pain, interruptions in the heart occur, a very strong feeling of lack of air, cardiac asthma, there may even be gastrointestinal disorders, weakness, sweating, and a sharp decrease in blood pressure. A heart attack suffered on the legs leads to consequences, such as a scar that disrupts the normal function of the heart muscle, weakening of the contractile function of the myocardium, chronic heart failure, and thromboembolism.
- An atypical form of myocardial infarction is abdominal. With this form of heart attack, very severe abdominal pain occurs. In this case, the patient is often suspected of having a catastrophe in the abdominal cavity, requiring surgical intervention. It is always worth remembering these forms.
- It is also important to pay attention to headaches, dizziness, movement disorders and thinking disorders. With such symptoms, a stroke cannot be ruled out, but it may also be a cerebral form of myocardial infarction.
- And, of course, we shouldn’t forget the classic myocardial infarction
Source: https://tepcontrol.ru/reabilitatsiya-posle-melkoochagovogo-infarkta-miokarda/
What are the signs and consequences of an infarction of the anterior wall of the heart?
Myocardial infarction is the death of a section of the heart, a process caused by a lack of blood supply. This is the result of blocking blood flow in the coronary vessels. Heart damage is classified based on the location of necrosis. Myocardial infarction of the anterior wall is considered widespread and frequent.
Localization specifics
Anterior myocardial infarction is characterized by significant muscle damage, and the prognosis for recovery is often poor. The reason for this is a decrease in cardiac output and inhibition of contraction function. This form is found in more than 1 million people worldwide every year. This condition is life-threatening because it alters the normal activity of the left ventricle, leading to cardiogenic pulmonary edema.
Fact! According to medical statistics, 10% of patients with extensive anterior wall infarction die within 12 months after an acute heart attack. Those who survive are considered at risk for recurrent attacks throughout their lives.
Provoking factors
Doctors call anterior wall infarction a largely “male” disease, although in older age groups the number of cases of diagnosing this condition in women increases. Often a hereditary factor is clearly visible, and this is associated with disorders of the blood vessels.
Risk factors for extensive damage to the anterior wall of the heart include:
- bad habits, in particular smoking;
- increased blood pressure;
- diabetes;
- increased amount of lipids/lipoproteins in the patient’s blood.
Types
Anterior infarction can be small or large focal. It is also divided according to its location on the front wall:
- anterior septal infarction;
- anterolateral;
- lateral myocardial infarction;
- anterior-apical;
- isolated-lateral;
- transmural.
Reasons for the development of the disease
The reasons for the development of myocardial infarction of the anterior wall of the left ventricle cause a lot of controversy among doctors. Some believe that this is an isolated ailment, others consider its reaction of the body to pathological processes. Regardless of the reasons, a heart attack is a violation of blood flow to an organ, which leads to a lack of oxygen. All this leads to the death of heart cells.
That is, it makes sense to consider not the factors that lead to the occurrence of the condition, but precisely the causes of impaired blood supply.
Impaired blood circulation
It occurs due to a decrease in the lumen of the heart vessels, which are responsible for supplying the heart with blood, and therefore oxygen. If they narrow (for any reason), oxygen starvation of the organ tissues occurs and coronary disease develops. Sometimes the cause of this condition is muscle spasm, the fight against it will be successful. If one reason is thickening of the walls of blood vessels, then treatment will not help, the process is irreversible.
But a more common cause is blood clots. Their occurrence in the coronary vessels is very dangerous. Sometimes blood clots enter the coronary arteries from other vessels or form in them. Regardless of this, they affect blood circulation - blockage with a blood clot is one of the common causes of myocardial infarction of the upper, anterior walls.
A less common, but also probable reason is the need for increased amounts of oxygen. The coronary vessels provide oxygen to the heart in normal mode, but during intense physical activity, more oxygen is consumed. If severe oxygen deprivation occurs, a massive heart attack is likely.
Why do problems with blood circulation occur?
The reasons for this are different. In particular, pathologies of blood vessels - atherosclerosis. In this case, plaques form, which narrow and, over time, block the lumen of the vessel. The causes of atherosclerosis are smoking, obesity, high blood pressure, and a passive lifestyle. Often – problems with metabolic processes in the body.
Sometimes circulation problems occur when the main heart arteries become inflamed. In this case, arteritis develops. The disease is rare, but possible with a heart attack. It can be infectious or non-infectious in nature.
Bruises can also lead to myocardial infarction, especially penetrating ones. Closed injuries are considered dangerous in terms of the occurrence of a heart attack, since they lead to serious damage, contusion of the heart, which provokes a blood clotting disorder. In addition, after bruises, blood clots form, which often cause acute myocardial infarction.
Thickening of the walls of blood vessels due to metabolic disorders - this process develops slowly, but it is irreversible. In this case, extensive anteroseptal myocardial infarction occurs very often.
Important! Congenital pathologies of coronary vessels are distinguished separately. Patients who have been diagnosed with such a defect need to be extremely careful, because they are at risk of developing a major myocardial infarction.
It is rare, but it happens that myocardial infarction of the anterior wall is the result of heart surgery. Doctors are not always to blame, because it is almost impossible to predict complications.
Symptoms of anterior infarction
The first and main sign of extensive myocardial infarction of the anterior wall is pain. It is felt behind the sternum. It may be pulling or aching. Patients often complain of pain in the left side of the body – jaw, shoulder blade, shoulder. The attack begins during the day, but the pain syndrome can come at night. The duration of the attack is no less than half an hour.
There are a number of possible symptoms for anterior wall myocardial infarction:
- coldness in the fingers of the extremities;
- breathing problems;
- general weakness;
- heartbeat instability;
- bluish skin;
- anxiety and panic;
- fainting state.
With an atypical course of a heart attack, there may be a sharp burning pain in the stomach, the urge to vomit, memory problems, and inability to concentrate.
This is how an extensive, that is, large-focal, infarction will manifest itself. As for the small-focal form, its symptoms are sometimes blurred and unclearly expressed. The only sign that will definitely be present is chest pain and anxiety.
With a big defeat
Extensive focal infarction is considered an acute disease when large foci of necrosis occur in the heart muscle due to atherosclerotic changes in the coronary arteries or their blockage with plaque.
Narrowing of the artery can be caused by:
- intravascular coagulation;
- atheromatous plaque;
- hemorrhage that occurred in an atherosclerotic plaque;
- thromboembolism.
| The most acute period | It ranges from 30 minutes to 2 hours, which lasts from the moment of the attack and the development of ischemia until the beginning of the death of parts of the heart. |
| Acute period | May last 2–10 days. At this time, areas of necrosis and myomalacia form; the disease can be protracted and recurrent. |
| Subacute period | The body spends 4–5 weeks. It is characterized by the completion of the initial scarring, when the necrotic tissue is replaced by granulation tissue. |
| Post-infarction period | The final formation and compaction of scar tissue occurs, it adapts to the process of functioning in the myocardium. The period can take from 3 to 6 months. |
Large foci of necrosis can form on the anterior, posterior or lateral walls of the heart muscle; their localization depends on the artery that supplies the area of the organ and has been damaged.
Most often, a heart attack occurs when one of the coronary arteries has been completely blocked, resulting in significant disruption of blood flow over a large area.
A large heart attack is difficult for patients to tolerate and leads to serious complications and takes longer to restore health. Its clinical picture has a pronounced pain syndrome, accompanied by weakness and sweating.
A characteristic sign of a large-focal infarction is heart failure, a significant increase in body temperature within 2-3 days. If the feverish state lasts longer, this indicates that complications have begun.
Early complications lead to disturbances in the rhythm and conduction of the heart, muscle rupture, cardiogenic shock, and the development of acute heart failure.
One of the late complications of an acute heart attack may be the development of cardiosclerosis, which appears within 2 months after the illness. Focal or diffuse cardiosclerosis can cause left ventricular aneurysm, chronic heart failure and pulmonary edema. Also, in some cases, this can provoke the formation of a wall thrombus.