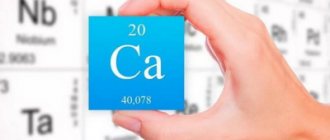
Parathyroid hormone (parathyroid hormone, parathyrin, PTH, in English literature PTH) is a product of synthesis of the parathyroid glands. It is the most powerful of the 3 factors that regulate Ca and P in the blood. Two other factors are also hormones - calcitonin and vit. D3. Yes, vit. D3 is such a powerful metabolism that it is also called a hormone.
The main work of parathyroid hormone is to increase Ca in the blood serum and decrease the concentration of phosphorus. Ca increases due to increased absorption by the intestines and reabsorption in the kidneys. Parathyroid hormone is not considered a mandatory element for determining it in the blood, except in cases of special direction. The reason for this may be an imbalance in the balance between P and Ca in the blood.
Why is Ca so important?
It not only forms part of teeth and bones, but also transmits impulses along nerve fibers and affects the contractile activity of all muscles, incl. and heartfelt. The parathyroid glands are located on the posterior surface or inside the thyroid gland symmetrically, usually there are 4 of them - 2 above and 2 below.
This is a rare case when the number does not necessarily end at 4. There can be 3 (in 3% of cases). In this case, most scientists consider one gland simply not identified).
The parathyroid glands, thyroid gland and thymus have a common origin - they are formed from the same type of endoderm already at 5-6 weeks of fetal development. Then they migrate according to their anatomy. With negative effects on the fetus, the localization of these organs, especially the parathyroid glands, may change and become atypical.
What does parathyroid hormone do?
Bone tissue - its dual action was noticed back in the 30s of the last century. What does it mean? This refers to its restorative anabolic effect under normal conditions and its destructive effect when increased.
If PTH remains elevated for a long time, bone density decreases and osteoporosis occurs, especially in menopausal women. The concentration of parathyroid hormone may decrease under the influence of propranolol and cimetidine.
Normal parathyroid hormone
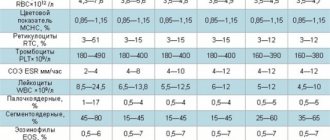
There are intervals of parathyroid hormone levels, the values within which are considered normal. They vary depending on age, but gender does not affect the level of this hormone. Sometimes the norms differ from one laboratory to another, so you need to rely on the form issued by a specialist. To complete the picture, the patient’s blood is additionally examined for phosphorus and calcium content. In addition, the level of these indicators is determined in the patient’s urine. The norm of parathyroid hormone for women and men is presented in the table:
| Age | Norm of parathyrin in men, pg/ml | Norm of parathyrin in women, pg/ml | Norm of parathyrin for pregnant women, pg/ml |
| Up to 20-22 years old | 12-95 | 12-95 | 9,5-75 |
| 23-70 years | 9,5-75 | 9,5-75 | |
| From 71 years old | 4,7-117 | 4,7-117 |
Features of PTG
Parathyrin exists in its intact form in the blood for a very short time - about 4-5 minutes, then it disintegrates. And in this minimum time, it must have time to perform all its functions. PTH is very sensitive even to room temperature and requires cooling.
If this is not the case, the analysis results will not be correct. Therefore, when taking PTG, some rules must be followed:
- the analysis is carried out only in a vacuum tube, not in an open one;
- You cannot leave the test tube at room temperature even for 5 minutes, you need to cool it immediately;
- Only use a refrigerated centrifuge.
If even 1 condition is not met, the result will be falsely low.
Functions of parathyroid hormone:
- reduces Ca in excreted urine and increases P;
- increases D3 to increase the absorption of Ca into the blood;
- in case of Ca deficiency in the blood, it helps Ca and P molecules leave the bones;
- if there is a lot of Ca in the blood, parathyrin stimulates its concentration in the bones;
- enhances the absorption of Ca in the intestine;
PTH also affects lipid metabolism, glycolysis in the liver, and the ANS. If the synthesis of parathyroid hormone does not occur for a long time, osteoarthritis develops.
Functions in the body
The hormonal background is proportional to the level of calcium - the lower the level of calcium ions, the more active the parathyroid glands that secrete this hormone work. PTH performs the following functions in the body:
- Prevents calcium from being washed out in urine;
- Monitors the complete absorption of Ca ions in the small intestine;
- Strong bones are also the responsibility of this hormone;
- If Ca in the blood is less than normal, PTH removes a certain part of calcium from bone tissue and improves its absorption by the intestines, then Ca enters the blood.
- Is there a lot of calcium detected? parathyrin promotes its accumulation in bones;
- The hormone promotes recovery after fractures.
How does the gland work?
The parathyroid glands have cell receptors that are hypersensitive to the level of Ca ions in the blood. They send a signal to the gland, stimulating it to synthesize PTH. Daily fluctuation of PTH - maximum concentration at 15:00; minimum (lowest level) - at 7 am.
PTH has its own antagonist, calcitonin. PTH is more active.
Reasons for decreased PTH:
- development of sarcoidosis – a systemic lung disease;
- magnesium deficiency;
- thyroid surgery;
- osteolysis – resorption of bone tissue.
- The following drugs can also affect PTH levels: COCs, drugs with vitamin D, magnesium sulfate, famotidine, prednisolone.
The PTH hormone can be produced in 2 ways: continuously and pulsed. Ca oscillations are caused by its pulsed production.
Why do parathyroid hormone levels increase?
The reasons why parathyroid hormones enter the blood in large quantities are different. The development of the primary form of the disease is influenced by tumors (malignant and benign). Primary hyperparathyroidism can also be caused by renal failure.
Article on the topic:
Oxalates in urine - what does it mean?
Parathyroid hormone is elevated due to:
- Calcium deficiency.
- Vitamin D deficiency.
- Pathologies of the renal apparatus and gastrointestinal tract.
- Thyrotoxicosis.
- Rakhita.
These etiological factors are characteristic of the secondary form of the disease.
Parathyroid hormones increase due to lung and kidney cancer. In this case, the production of hormonal substances is carried out by the inactive tissue structures of the glandular organ. These processes occur in tertiary hyperparathyroidism.
For each form of pathology, its own amount of parathyroid hormone is determined:
- For primary – 2-4 times higher than standard indicators.
- For secondary - 5-10 times more than normal.
- For tertiary - 11 times more.
Indications for taking a PTH test
Indications for testing may include:
- abnormalities of Ca and P;
- bone resorption status;
- pseudofractures of large bones;
- increased density of spinal bone tissue (osteosclerosis);
- stones in the kidneys;
- presence of neurofibromatosis;
- neoplasia of the endocrine glands;
- parathyroid adenoma.
What can affect the test result:
- Drinking milk the day before, diuretics, OK, gentamicin and excess vitamin D can lower the levels.
- During pregnancy and pregnancy, taking corticosteroids, estrogens, rifampicin, lithium, anticonvulsants and laxatives, PTH increases.
- Conducting studies with radioisotopes prior to analysis.
Symptoms of decreased hormone secretion (hypoparathyroidism)
Hypateriosis is characterized by the following symptoms:
- muscle activity is impaired;
- problems appear with the cardiovascular system, autonomic nervous system, psyche, and intestines.
Also, with insufficiency, visual and trophic disturbances occur.
Muscle disorders:
- convulsions, involuntary twitching, spasms in the bronchi, intestines, trachea;
- changes in thermoregulation - from chills to hot flashes;
- CVS – tachycardia;
- cardialgia;
- arrhythmias.
Psyche:
- symptoms and changes appear with a long process - insomnia;
- depression;
- feeling tired;
- decreased memory and intelligence.
Bone tissue:
- lack of calcium in the blood can cause bone pain and bone deformities;
- improper walking;
- children are lagging behind their peers in growth;
- Their skeleton is also formed incorrectly.
Signs of gastrointestinal disorders:
- intestinal colic;
- disruption of the pancreas;
- vomiting and nausea.
Autonomic disorders - symptoms can be in the form of:
- profuse sweating, fainting or dizziness;
- increased sensitivity to sounds, bitter and sweet tastes;
- hearing loss and ringing in the ears;
- algomenorrhea.
Trophic disorders:
- skin moisture disappears;
- spots and peeling appear on it;
- candidiasis is often associated;
- baldness develops, gray hair appears early;
- hair growth noticeably slows down.
The condition of tooth enamel deteriorates - it becomes susceptible to caries.
Visual impairment:
- night vision deteriorates;
- accommodation is impaired;
- Cataracts develop up to blindness.
Despite such complex disorders, many symptoms are reversible when calcium levels in the blood are normalized. But with severe disease or improper treatment, consequences may remain. Often, a complication in the form of acute renal failure may immediately appear.
When parathyroid hormone decreases, P increases. In this case, neuromuscular activity becomes abnormally high and a tendency to seizures appears. Ca begins to be deposited in internal organs and tissues and thickens them, because Ca is washed out of the bones to increase it in the blood.
Methods for treating elevated parathyroid hormone
Treatment tactics largely depend on the diagnosis made by the doctor. If primary hyperparathyroidism has been detected, then surgical intervention cannot be avoided in this situation. The tumor that stimulates the production of the hormone is removed, or part of the gland itself is cut out.
Patients with hypercalcemic crisis are admitted to intensive care. Endocrinologists take care of their health. During a crisis, diuresis is indicated. During the procedure, sodium chloride or Furasemide is administered intravenously. Additionally, Complexon is prescribed (binds free calcium in the bloodstream) and Calcitrin (promotes the deposition of calcium in bone structures).
Patients who have been treated for hyperparathyroidism are regularly monitored by an endocrinologist, and once every 6 months they are required to:
Article on the topic:
What is thyroxine (free t4)? Normal in the female body
- Donate blood to determine calcium levels.
- Undergo instrumental studies that document the health of the kidneys.
- Attend an ultrasound.
- Undergo bone densitometry.
Secondary hyperparathyroidism is eliminated with drug therapy. Calcium-based drugs are used, as well as vitamin D. If conservative treatment does not have the desired therapeutic effect, the patient is referred for surgery. Surgical intervention is appropriate when the amount of parathyroid hormone is 3 times higher than normal.
Tertiary hyperthyroidism occurs in patients who have had a kidney transplant. To alleviate the patient's condition, he undergoes a subtotal parathyroidectomy.
Attention! Treating hyperparathyroidism with folk remedies without resorting to traditional medicine is extremely dangerous in any form.
Low PTH or hypoparathyroidism
It can be primary and secondary. In primary, the parenchyma of the gland suffers; in secondary, external factors act.
The primary ones include:
- Congenital - the anlage of an organ is disrupted during intrauterine development. The glands may be underdeveloped or completely absent.
- Postoperative – damage during strumectomy or resection of the parathyroid glands themselves or the vessels feeding them. If the vessels are damaged reversibly, then a transient form of hypoparathyroidism develops - this phenomenon is restored and goes away after a month.
- Post-traumatic - a consequence of radiation or radiation therapy, injury to the glands with subsequent hemorrhage or inflammation.
- Autoimmune – antibodies against the parathyroid glands are formed in the blood and destroy them. Such hypoparathyroidism is often combined with damage to the adrenal glands or mycosis of the skin and mucous membranes.
- Idiopathic hypoparathyroidism is a genetic disorder of unknown etiology.
Secondary hypoparathyroidism develops outside the glands, but leads to impaired Ca metabolism. This is possible with hypothyroidism and oncology.