A blood test for allergens is one of the most reliable diagnostic methods for testing a patient with suspected allergies.
It is difficult to establish an accurate diagnosis even in the presence of many symptoms, since allergies are skillfully disguised as intestinal, dermatological or bronchopulmonary diseases.
The success of allergy treatment depends entirely on the complete isolation of the patient and provoking factors. A blood test allows you to determine the presence of an allergic reaction and identify the allergen or a whole group of them.
How to take a blood test for allergens?
The easiest way to get rid of allergies is to eliminate the allergen from a person’s life. If this concerns a food allergy to a certain product, then it is enough for a person to simply not eat it. But what should people who suffer from allergies to dust or pollen do? First you need to identify the allergen itself , which causes such a reaction.
Children suffering from allergies are prescribed a course of research.
Very young children have an insufficiently developed immune system and when conducting research, the results may not be informative enough, so it is advisable to conduct research only for children after 3 years of age .
Expert opinion
Kovaleva Elena Anatolyevna
Doctor-Laboratory Assistant. 14 years of experience in clinical diagnostic services.
Laboratory tests for susceptibility to allergens in children are often based on blood tests. When conducting research, a specific allergen is determined.
When it comes into contact with human blood, the appearance of special antibodies can be noted.
This type of research is safe for the baby’s well-being and does not cause him serious discomfort.
There are only a few types of allergy tests that use biological material (blood):
- RAST;
- test for immunoglobulin type E.
The first test makes it possible to identify a specific type of allergen and the direction of subsequent research. If a positive result is obtained, it is necessary to conduct allergy tests of a more narrow focus.
The RAST test requires a blood test .
The resulting biomaterial is divided into test tubes. A certain amount of a special solution is added to each, obtained by concentrating one of the allergens. When a large number of antibodies are formed in the blood, the doctor can judge which substances can cause allergies in a person.
Expert opinion
Kovaleva Elena Anatolyevna
Doctor-Laboratory Assistant.
14 years of experience in clinical diagnostic services.
A second allergic reaction study, or immunoglobulin E test, makes it possible to identify a more precise allergen.
A small volume of blood is taken from a person, which is mixed with a small amount of specific allergens belonging to one of the groups:
- inhalation;
- contact;
- food.
For children under the age of 1 month , if severe allergies occur, a venous blood test can be prescribed to determine the reaction to allergens.
For this procedure, a specific or general IG E study is used. However, it is more advisable to wait 6 months .
A blood test for allergens can be performed in the following cases:
- with prolonged runny nose without signs of a cold or fever;
- for sore throat and coughing that lasts more than 3 weeks;
- when itching or skin rashes occur;
- with itching in the eyes, throat, nose;
- when the child has difficulty breathing or begins to choke;
- when the above symptoms decrease after using antihistamines.
Pathogenesis of the development of an allergic reaction in infants
In response to the entry of an allergen into the baby’s body, the synthesis of specific immunoglobulins E occurs, which activate a chain of reactions with the formation of inflammatory mediators (histamine, serotonin and other factors), leading to the development of allergy symptoms - skin rash, rhinitis or conjunctivitis.
Clinical manifestations of allergies in infants
Increased sensitivity to allergens in infants can manifest itself in the form of:
1) allergic skin lesions:
- allergic diathesis (peeling of the skin of the cheeks, forehead, buttock area, intense itching and redness of the skin;
- gneiss, urticaria, local swelling of the skin;
- manifestations of prickly heat and/or persistent diaper rash of unknown etiology (with a comfortable microclimate and good care of the baby’s skin folds);
2) lesions of the digestive tract:
- frequent regurgitation;
- loose stools or constipation;
- flatulence and persistent colic;
- vomit;
3) respiratory disorders:
- allergic rhinitis;
- bronchospasm (frequent dry cough, difficulty breathing, frequent respiratory infections with laryngitis, alveolitis or obstructive bronchitis);
4) combined lesions of organs of various systems
Often there are combined skin and respiratory system (rhinitis or bronchospasm), allergic skin reactions and intestinal lesions.
The combination of allergic reactions with damage to several systems in infants is considered a high predisposition to the occurrence of dangerous allergic diseases: bronchial asthma, eczema, atopic dermatitis or the development of complex inflammatory-allergic pathologies of the kidneys, heart, blood vessels, musculoskeletal system;
5) other dangerous conditions
- Quincke's edema;
- anaphylactic shock.
Types of allergy tests
Types of allergy diagnostics are divided into:
- Blood analysis.
It is widely used for different types of allergies. Its task is to determine the presence of antibodies to allergens in the blood and the level of immunoglobulin E. Using this method, the general group of allergens is first determined, in order to then establish a narrow group. The results are deciphered by a doctor; not only the level of indicators is important, but also their ratio.
Skin tests are also divided into 4 types:
Depending on the method of implementation, allergy diagnostics is divided into:
- nasal – used for allergic rhinitis. To do this, a potential allergen is injected into the nose and the reaction is monitored (sneezing, itching, runny nose, swelling);
What results can you get?
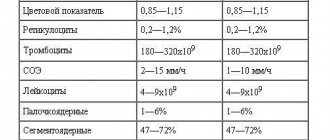
Blood tests are performed over several days. At the same time, the level of immunoglobulins in plasma is determined. Immunoglobulin E is normally present in human blood only in small quantities. An increase in its concentration is observed during allergic reactions. At the same time, there is a dependence of the IgE level on the severity of the pathological process. Normal levels of this protein may vary depending on age:
- in the first two years of life, its concentration should not exceed 64 mIU/ml;
- in older children – 150 mIU/ml;
- in adults – 110-120 mIU/ml.
This indicator is not specific and allows you to judge whether the patient has a tendency to allergies or whether it is necessary to look for another reason for the change in health status.
The analysis is deciphered based on the obtained immunoglobulin values, which are specific for each specific substance. For this purpose, the immunoblotting technique is used, which, using serological reactions, allows one to detect antibodies formed upon contact with a specific antigen. In this case, nitrocellulose membranes are used, on which individual proteins are applied.
To identify the allergen, various panels are used, among which the most popular are:
- pediatric;
- inhalation;
- food;
- mixed.
The determined antibody titer can have different values, allowing the doctor to diagnose the disease:
- absence of antibodies (less than 0.35);
- very low titer (0.35-0.7);
- low titer, but the result is close to the upper limit (0.7-3.5);
- a pronounced titer, at which clinical symptoms most often occur (3.5-17.5);
- high titer (17.5-50);
- very high titer (50-100).
Since the titer indicator does not always directly depend on the degree of change in immune reactivity, the results obtained should be compared with the clinical course of the allergy.
Features of testing for allergies in a child
In general, a child, upon referral from a pediatrician and an allergist, undergoes the same allergy tests as an adult.
Therefore, both a blood test, which is considered a safer method, and skin tests are used. Since the reaction of the child’s body can be very strong, all procedures are carried out only under the constant supervision of a specialist.
Typically, a child’s reaction to a skin test appears within 15 minutes. As a rule, the child’s body tolerates such manipulations well.
If an allergy appears in a breastfed baby, then there is no point in conducting a blood test, since his blood contains the mother’s antibodies obtained with milk.
Advantages and disadvantages of in vitro samples (blood tests)
Advantages of the method:
- There are practically no contraindications, the method is safe;
- The method allows you to weed out false-positive and false-negative results of skin prick tests;
- Less invasive compared to skin prick tests - a single injection is performed to collect blood.
Disadvantages of the method:
- More expensive than skin prick test;
- Less sensitive;
- Not all laboratories have mastered the technique;
- There may be cross-reactions between food and inhalant allergens;
- Not sensitive to non-protein antigens.
Patients for whom the test is indicated should undergo a blood allergy test.
Indications for determining specific IgE in the blood:
- There are contraindications to skin prick tests;
- The performed prick tests did not give a clear result and contradict the medical history;
- Pronounced dermographism;
- Patients with common skin diseases;
- Availability of indications for the test in patients with a history of anaphylaxis, especially in the first 1.5 months after the reaction);
- Infancy or severe discomfort in the patient when performing skin tests.
Contraindications and restrictions for blood tests:
- Newborns (has no diagnostic value);
- No analysis is carried out to assess the likelihood of anaphylactic manifestations due to penicillins and insect venom.
Preparing for an allergy blood test:
- You should not eat food later than 2 hours before the test (blood must be donated on an empty stomach);
- Avoid drinking alcohol the day before;
- Do not smoke for 2 hours before the blood test.
In modern specialized clinics there are a huge number of tests for screening antibodies. (IgE)
The set of tests for determining inhalant allergens includes the following:
- allergens of grasses (early and late flowering - timothy, orchard grass, fragrant spikelet and many others);
- A set of tests for determining antibodies to pet allergens (cat and dog epithelium, dog hair, parrot and canary plumage, guinea pig hair and many others);
- A set of tests for determining food allergens (meat, seafood, fruits, nuts, cheeses, vegetables).
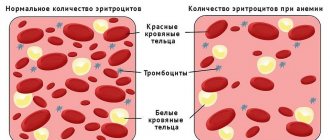
A complete blood test for allergies can reveal eosinophilia. Eosinophils are a type of granulocyte leukocytes, the number of which increases during allergic reactions and helminthic infestation. A general blood test allows you to determine the level of cellular elements of the blood and a number of its parameters: red blood cells, white blood cells with a leukocyte formula, platelets, ESR (erythrocyte sedimentation rate). The leukocyte formula is a determination of the number of different leukocytes as a percentage (monocytes, neutrophils, basophils, eosinophils, lymphocytes).
A complete blood count (CBC) is a simple but very valuable diagnostic examination for determining blood diseases and inflammatory processes. But a clinical blood test for allergies (general blood test) is not decisive in the diagnosis of pathology.
allergoportal.ru
Provocative methods
Provocative tests are carried out in cases where skin tests for allergies and immunoglobulin studies have not identified the cause of the allergy. This test should only be performed by an experienced physician. But tests of this kind are rarely prescribed for allergies in children due to the risk of developing anaphylactic shock.
The essence of the research is that the allergen is applied directly to the mucous membrane of the selected target organ. Provocative tests can be inhalational, nasal or conjunctival. Inhalation ones are performed exclusively in a hospital setting, while others can be performed on an outpatient basis. After some time, the immune reaction is studied.
Why is a blood test better than a skin test?
In some cases, doctors prefer to limit themselves to prescribing those examinations that can be done using blood serum. This diagnosis has several advantages:
- Contact of the skin with a possible allergen is completely excluded. This eliminates the development of an acute allergic reaction.
- It is possible to determine an irritant substance in the blood at any time and for almost everyone. Skin tests are carried out only if several conditions are met.
- To identify different allergens, blood is taken once.
- Blood can be used to determine both objective and quantitative indicators, this makes it possible to determine the degree of sensitivity to various allergens.
Skin tests are not always prescribed, since not everyone is suitable for them.
They are not used if most of the skin is changed due to allergies or skin diseases.
This examination is contraindicated for those who have a history of anaphylaxis.
The results of skin tests will not be reliable in cases where the patient has been taking medications for a long time that inhibit the body’s sensitivity to possible allergens.
Due to the low information content, skin tests are not prescribed for children and the elderly.
Skin tests
Skin tests for allergens are carried out in several ways, these are:
- Scarification test. A few drops of a solution containing allergens are applied to clean, antiseptic-treated skin, then the top layer of skin is scratched using a scarifier.
- Peak test. Drops with allergens are also applied to the skin, then superficial injections are made through these drops with a disposable needle.
- The application test (patch test) involves attaching a patch with applied allergens to the skin.
The patch test is considered the least invasive examination method. They usually walk with the patch glued on for two days, after which the doctor evaluates all changes.
The application method of examination is most often used for allergic dermatitis.
Peak test and skin scarification allow you to obtain examination results within 15-20 minutes; if during this time skin changes appear in the form of swelling, redness, itching, it means that the human body is sensitive to these substances.
These tests can identify up to 15 possible allergens at one time.
The scratch test and peak test are not always prescribed, since there is a possibility of allergens entering the body, which can result in anaphylactic shock.
Contraindications to these tests:
- The child's age is under 5 years;
- Identification of cases of anaphylaxis during a conversation with a patient;
- Pregnancy and lactation period;
- Hormone treatment period;
- Age over 60 years;
- Exacerbation of cardiac, nervous, allergic, gastrointestinal diseases.
Preparing for analysis
When various allergy symptoms appear, it is necessary to eliminate the allergen itself. This can be done by identifying it using tests that require blood testing. The blood donation procedure must be carried out in the morning, on an empty stomach . When taking antihistamines, it is recommended to stop using them for at least 4 days before taking the test.
If a child is prescribed skin tests , then this procedure should not be done during an exacerbation of allergies, since the results of the study will not be reliable, since the body is overly susceptible at this time. When visiting an allergist, the patient will be given instructions for the correct testing, which must be strictly followed.
How to identify an allergen in a child?
One of the most difficult patients for an immunologist is a child, and the younger he is, the more difficult it is to make a diagnosis. Why? Because the baby’s immune system is not yet fully formed, an allergic reaction is most often associated with a short-term stage of the body’s adaptation to a new thing and can stop on its own as it grows up.
The most common in infants under one year of age, for example, are food allergic reactions associated both with artificial nutrition (many mixtures, unfortunately, are produced in violation of technology and with the use of potentially allergenic components) and with the diet of the nursing mother. Therefore, identifying an allergen in a child is a complex, painstaking task that requires long-term observation.
Many experts generally do not recommend doing an analysis before 3 years of age, since it is not very informative. But overly cautious parents may still try to do something. For example, try the elimination method, when potential allergens are gradually removed through trial and error. In the case of food allergies (and not only with them), it is wise to exclude dangerous foods from the diet. First, of course, the most typical ones. These include: chocolate, cocoa, citrus fruits, pomegranates, melons, black currants, strawberries, raspberries, honey, fish, caviar, nuts, mushrooms. Cow's milk and eggs, semolina, wheat bread, cottage cheese, whole milk, fatty beef and pork, and chicken can also be potentially dangerous. Parents should keep a food diary, which includes all the foods that the baby eats, his reaction to them, and the amount in grams. If after 7-14 days relief occurs and symptoms disappear, then you can try giving the allergen again. The resumption of symptoms will be the final sign that the enemy has been identified, and all that remains is to stop using it for at least 3 years.
Diagnosis of allergies is a complex process that must be carried out under the supervision of a specialist. First, the doctor will study information about the child’s way of life, his diet, the health status of the parents (allergies can also be hereditary), living conditions (are there any pets, what kind of pillows and blankets, what season does the allergy appear). To do this, parents must keep a diary for two weeks, in which they record all the foods that the child ate, write down what clothes he wore, and with whom he came in contact. Once the main “aggressor” has been identified, it is necessary to exclude him from the child’s environment. Then a hypoallergenic diet is created, even if the problem is not food. Remember that self-medicating allergies is strictly prohibited!
All methods of examining an allergic patient can be divided into two categories:
- In vivo - the patient is present during the test (skin tests, provocations).
- In vitro - only blood serum is collected.
Then tests are prescribed, which can be performed using the following methods:
- Scarification skin tests.
- Detection of specific immunoglobulins, Ig E antibodies.
- Provocations, provocative tests.
- Elimination tests.
How are such tests done for allergies in children?
Scarification skin tests
Scarifications (scratches) are made on the forearm, and a drop containing the allergen is applied to them. Peak testing (injection) with a sterile thin needle with injection of the allergen under the skin no more than 1 mm inside is also practiced. The skin area must be treated with an antiseptic. Both methods are absolutely bloodless, as they do not touch the capillary.
Typically, no more than 15 samples can be performed at one time. The body's reaction is visible after 15 or 20 minutes in the form of slight local swelling and redness. The least aggressive method is the application method (patch test), when a special patch with an allergen is glued to the skin. The reaction of the skin in the form of itching, hyperemia, swelling indicates a positive response to the presented allergen. However, these methods have contraindications:
- Age up to 5 years.
- History of anaphylactic shock.
- Exacerbation of diseases - allergic, gastrointestinal, cardiac, nervous and others.
Determination of IgE and IgG4 antibodies or quantification of specific immunoglobulins
This method (in vitro) is considered highly sensitive, since it can be used to determine the entire group of true provoking allergens. After all, initially our blood contains a small amount of IgE, and after the introduction of an allergen, its amount significantly exceeds normal limits.
This method is most often used as an analysis for food allergens, thereby complementing the diagnostic information obtained by provocative or skin methods or being the only possible method when it is impossible to use others for various reasons. It is very convenient because you can get tested for allergies at any time. The analysis will require blood from a vein, taken 3 hours after eating, which is very convenient in the case of a small child.
RIST (radioimmunosorbent paper tracer) method
This method is effective in cases of suspected allergic rhinitis, bronchial asthma, sinusitis and bronchitis. RIST gives a fairly informative and accurate picture of the level of IgE and IgG antibodies.
Provocative methods
They are rarely prescribed to children due to the risk of anaphylactic shock. Provocative tests are necessary in cases where skin tests and IgE level studies are not sufficient for an accurate diagnosis, and the doctor has doubts about the true causative agent of the disease. They are carried out only under strict medical supervision.
A small amount of the allergen is placed under the tongue, injected into the nose, or less often directly into the bronchi. After a certain amount of time, the body’s reaction is studied, which can be very acute. For this purpose, the patient must be in the hospital.
What are prick and provocative tests?
Currently, there are several laboratory tests that can be used to determine which products and substances provoke an allergic reaction. There are prick tests, scarification, and patch tests.
Each examination method is carried out in a certain way and has its own advantages. But most specialists prefer to find out what causes allergies in a child using a general blood test for antibodies.
In professional language, such an analysis is called an allergy test or allergy diagnosis.
Depending on the clinic, testing may be carried out in one way or another.
Doctors claim that determining allergies using a general analysis of blood fluid is the most advantageous, since the biomaterial is taken only once. Further, it can be used to determine the reaction to many allergens.
The undoubted advantage of diagnostics is that there is no negative effect on the body; blood testing is carried out exclusively in a laboratory.
Rashes, itching and runny nose occur as a response of the immune system to contact with a specific irritant. Having encountered pathogenic factors, the immune system triggers many responses, one of which is increased production of immunoglobulin. The essence of this analysis is precisely to determine these antibodies in the blood.
Indications for examination
Many parents doubt whether their child needs such tests. Experts assure that if a child periodically develops a rash and redness on the skin, allergy testing is mandatory.
With the help of testing, you can determine the risk of developing allergic diseases and identify what is an irritant for the body.
It is recommended to carry out diagnostics if there is:
- eczema, skin dermatitis;
- bronchial asthma;
- suspected allergies due to taking certain medications;
- reaction to certain foods;
- helminthiasis;
- inflammatory diseases of the respiratory system.
Most doctors are of the opinion that such a test should be done in any case, since testing will help identify what the irritant is and it will be possible to prevent further contact with it.
Allergy indicator in a general blood test
Taking blood for a clinical blood test from a finger is quite simple if there is any suspicion of an allergic reaction.
- Most often, this test is performed when a child is suspected of having an allergy.
- A typical change and indicator of allergies in a general blood test is an increased level of eosinophils - this is a type of white blood cell that is responsible for the formation of certain types of allergic reactions.
- Normally, their number does not exceed 5% of the total number of leukocytes.
- Exceeding this value indicates an active allergic reaction.
How is the analysis carried out?
How to donate blood for analysis in order to get reliable results? Preparation is described above. The material is taken exclusively from a vein located in the elbow area. Before inserting the needle, the doctor tightens the baby’s arm just above this place with a tourniquet, so the procedure will go faster.
Usually a fairly large amount of biomaterial is taken - at least 7 ml. After the puncture, the blood is poured into a test tube, then the flask is sent to the laboratory. A form with a transcript of the analysis is issued within 7 days.
Parents often ask where to donate blood in order to get reliable information. The best option is to visit a special diagnostic center. Such laboratories are equipped with the maximum number of reagents, which makes it possible to obtain the most accurate results.
For infants, blood tests are done in the same way as for older children. The only difference is that a smaller amount of blood is taken from infants (usually up to 5 ml).