0
Author of the article: Marina Dmitrievna
2017.09.29
1 659
Blood analysis
Biochemical analysis is an informative method of laboratory diagnostics. Helps to comprehensively develop the clinical picture and identify serious pathologies and disorders in the functioning of internal organs. After receiving the results, doctors draw a conclusion about what exactly the body needs, what vitamins and microelements it lacks, and what metabolic disorders exist.
The analysis is necessary to prescribe subsequent effective treatment. But to get true results, patients should undergo preliminary preparation. And laboratory assistants must follow the rules that the technique of taking blood for biochemical analysis requires, taking into account the algorithm and instructions for sequential actions.
What does detailed analysis determine?
A detailed blood test is similar to a general blood test, but it is based on determining a larger number of indicators.
A more in-depth study or general detailed analysis of plasma and formed elements of the body's liquid connective tissue studies a large number of elements, and also determines the erythrocyte sedimentation rate and calculates the detailed leukocyte formula.
All determined indicators in the schematic recording of blood test results (hemogram) have Latin designations.
To understand quantitative and qualitative indicators, you need to find out what these unfamiliar Latin letters mean.
Here is their transcript:
- HGB is the Latin abbreviation for hemoglobin, a complex protein that saturates tissues with oxygen;
- WBC is the designation for white blood cells (leukocytes) that produce antibodies to protect the body from infections;
- RBC is the Latin name for erythrocytes, the red blood cells that distribute oxygen throughout the body;
- HCT is a designation for hematocrit, which measures the ability of blood to deliver oxygen to tissues;
- MCV is a Latin term that refers to the average volume of red blood cells in the body's fluid connective tissue;
- MCH is a designation for the average amount and concentration of hemoglobin in one red blood cell (erythrocyte);
- RDW-CV is the red blood cell distribution scale;
- PLT is a Latin term that refers to the number of spherical, colorless cells without a nucleus (platelets) responsible for blocking vascular damage and blood clotting;
- PCT is the Latin name for thrombocrit, or the volume of blood carried by platelets;
- MPV is the average quantitative indicator of spherical, colorless cells without a nucleus (platelet);
- PDW – scale of distribution of platelets in the blood;
- NEUT is the Latin name for neutrophilic leukocytes that protect against bacteria and fungi;
- LYMPH – designation of the number of lymphocytes (cells of the immune system) in the blood;
- MONO – designation of monocytes or active phagocytes of peripheral blood;
- EO – designation of the number of eosinophils (cells of the immune system);
- BASO is a quantitative indicator of basophils (large granular leukocytes).
To obtain an extended hemogram, blood is drawn not from a finger, but from a vein in the crook of the arm. A general analysis in detailed form is also given in the morning, always on an empty stomach.
Red blood cell indicators
By considering the parameters of red blood cells, one or another type of anemia in a person or other abnormalities can be diagnosed.
- Red blood cells (RBCs) are red blood cells that contain a special protein called hemoglobin. The latter ensures the delivery of oxygen to the tissues of human organs, as well as the removal of carbon dioxide from them. The number of red blood cells is measured in cells per liter of blood, and the number of cells should be multiplied by 1012. The normal number of red blood cells in adult men ranges from 4.0 to 5.0, in women - 3.9–4.7. Reduced red blood cells are characteristic of anemia, pregnancy, blood loss and vitamin deficiency. An increased content of red blood cells is often observed during dehydration.
- Hemoglobin (HGB): when deciphering a complete general blood test, this indicator is measured in grams per liter of blood. The normal hemoglobin level for men is considered to be 130–160 g/l, for women – 120–140 g/l. Low hemoglobin indicates anemia, leukemia or a deficiency of B vitamins. If the indicator is elevated, the patient may have certain diseases of the lungs, heart, kidneys and liver that cause increased production of red blood cells.
- Color index: indicates the degree of saturation of red blood cells with red pigment. Its norm ranges from 0.8 to 1.1. An increase in the color index is observed in cancer and vitamin B12 deficiency. Lack of pigment indicates anemia.
- Hematocrit (HCT): Expressed as a percentage. This indicator determines the percentage of red blood cells to plasma. For men, the norm is 40–48%, for women – 36–42%. An elevated hematocrit may indicate dehydration and heart failure, while a low hematocrit may indicate renal failure and anemia. Also, a hematocrit deficiency can be detected when deciphering a detailed blood test of a woman experiencing the last months of pregnancy.
- Mean erythrocyte volume (MCV): This indicator is assessed if you need to determine the type of anemia, but MCV will not be informative if a person has many red blood cells of an abnormal shape, for example, sickle-shaped, in his blood. MCV is measured when deciphering the detailed general analysis in femtoliters. The normal volume of 1 corpuscle ranges from 80 to 100 femtoliters. Too large red blood cells are characteristic of some liver diseases, and small ones are characteristic of hemolytic and aplastic anemia.
- Mean hemoglobin content per erythrocyte (MCH): expresses the absolute hemoglobin content in 1 red blood cell. Measured in picograms. The norm ranges from 27 to 35 picograms. A decrease in the indicator may indicate the development of cancer and iron deficiency anemia.
- Red blood cell distribution width (RDW): the coefficient is expressed as a percentage. Within normal limits, the value ranges from 11.5 to 14.5%. An elevated value often indicates thalassemia, folic acid deficiency, cancer metastases to the bone marrow, or liver damage.
- Erythrocyte sedimentation rate: reflects the ratio of plasma protein fractions. ESR shows how quickly red blood cells settle in 1 hour. For women, the norm for ESR is considered to be a number ranging from 2 to 15 mm/h, for men - from 2 to 10 mm/h. If a person has an elevated ESR, this may indicate foci of inflammation in the body, as well as cancer.
- Reticulocytes (RTC): These are immature red blood cells and are calculated as a percentage of the total red blood cells. They should be no more than 12% in human blood.
Blood indicators for coronavirus
A number of blood indicators for coronavirus help not so much in making a diagnosis, but in determining the stage, severity of the disease, prognosis, and according to them, the doctor can make changes in the treatment of the infection.
Leukocytes
84% of patients had low lymphocytes and eosinophils in the blood, and a general drop in the number of leukocytes (leukopenia) was observed in a third of those infected. This means that when the coronavirus multiplies inside the body, it suppresses the activity of the immune system.
In extremely severe cases of the disease, massive inflammation develops in the lung tissue, which means the influx of immune cells into this area accelerates. At this stage, increased neutrophils (neutrophilia) are found in the leukocyte formula of a general blood test. This is regarded as an unfavorable sign - a “cytokine storm”. Due to an overly active reaction, pulmonary edema occurs, that is, acute respiratory failure.
It is the “cytokine storm” that causes death in elderly patients in 57% of cases. It was noted that at the same time during this period the level of ferritin in the blood increases rapidly, its increase is interconnected with the degree of damage to the lung tissue.
Antibodies
In the acute stage of the disease, immunoglobulin M is found; it reaches its maximum value by 10-14 days. Detection of this protein in the blood is necessary to distinguish coronavirus from other diseases with similar symptoms. The second group of antibodies is IgG, they are produced at a late stage and remain in the blood of recovered people.
So far, there is conflicting information about what proportion of those who have recovered from the disease are immune. Doctors give figures from 29 to 80%. It is also unknown how long it will protect against re-infection (from 3 months to 1-1.5 years). All this conflicting information is explained by the fact that the pandemic is not over yet, and it is too early to draw final conclusions.
ESR
ESR (erythrocyte sedimentation rate) increases in most patients with coronavirus. Its growth may be the first, and sometimes the only change in the general blood test. Since this is one of the indicators of inflammation, the increase in the indicator is especially pronounced with the development of pneumonia.
Biochemical indicators
With coronavirus infection in the active stage, the following signs are found:
- renal dysfunction: high creatinine, urea;
- liver: increased levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST);
- damage to the heart muscle: increase in creatine kinase (CPK), lactate dehydrogenase (LDH);
- coagulation disorders: prolonged prothrombin time, increased D-dimer;
- inflammation: C-reactive protein and interleukins increase;
- addition of a bacterial infection: procalcitonin increases;
- blood poisoning (sepsis): lactic acid is sharply increased, blood PCR test is positive, lymphocytes are falling.
At what age is blood taken from a patient for research?
The composition of a person's blood changes throughout life. In a child, this process is more dynamic, since he is in the stage of growth and active development. Doctors distinguish several age groups:
- Newborns (one day);
- 1 month;
- 6 months;
- 1 year;
- 1-6 years;
- 7-12 years (inclusive);
- 13-15 years old.
Indicators that are normal for one age category are considered deviations for another. When conducting research, doctors take this factor into account. However, in some cases this is not the only influence. For example, a decrease in hemoglobin is observed with increased physical activity or dehydration.
What does a clinical blood test show?
Typically, a visit to a therapist for various reasons is accompanied by a referral to donate blood to a laboratory. Therefore, most patients wonder why a clinical blood test is needed - what this study shows, what diseases can be identified with its help, how informative it is.
What does a clinical test of blood from a finger and vein show?
As a rule, for a general study of biological fluid, it is taken from a finger (capillary). For biochemical analysis, venous blood is required.
Modern laboratories conduct clinical research only on biological fluid from a vein. The fact is that capillary blood contains a fairly large amount of intercellular component, due to which microscopic clots from damaged cells can form during the sampling process. This significantly reduces the information content of the analysis; there will be a need to take it again. Venous biological fluid does not contain an intercellular component, so the blood components are not destroyed.
Clinical analysis is usually prescribed to confirm the following pathologies:
- anemia;
- infectious lesions;
- inflammatory processes;
- allergy;
- bleeding disorders;
- internal bleeding;
- dehydration of the body;
- hemoglobinopathies;
- erythrocytosis;
- thrombocytopenia;
- poisoning;
- liver diseases;
- increased radioactive background;
- parasitic infestations;
- radiation sickness;
- tuberculosis.
Also, the study in question can be informative for some “childhood” diseases, so many parents are interested in whether a clinical blood test will show whooping cough. Pediatricians give a negative answer to this question. In most cases, a clinical study is not informative enough when diagnosing whooping cough; it is better to donate blood for specific antibodies (immunoglobulins) and do a bacterial culture of material from under the tongue and from the mucous membranes of the nasopharynx.
Can a clinical blood test show cancer?
With malignant tumors of various organs, changes in such indicators as the amount of hemoglobin, red blood cells, platelets and leukocytes are observed. But it is impossible to make a diagnosis based solely on fluctuations in these values, since they are also characteristic of many other pathologies.
Therefore, you should not wonder whether a clinical blood test will show cancer; it is better to follow other, more informative, diagnostic instructions from your doctor.
| Carcinoembryonic antigen If you have been prescribed a test for CEA or CEA, but you have no idea what these indicators are, what they are used for and what they show, read this article. Our latest material clearly explains the meaning of this tumor marker, indicating its normal values and the reasons for its increase. | Alkaline phosphatase is normal. A significant indicator in a biochemical blood test is the activity of various enzymes in the body. Alkaline phosphatase is a key substance in metabolism. Find out what the normal level of alkaline phosphatase is and what factors can affect the level of the enzyme in the blood. |
| Increased alkaline phosphatase - causes Results of a biochemical blood test may indicate an increase in alkaline phosphatase. Find out in which diseases the level of alkaline phosphatase is elevated, and whether changes in the amount of the enzyme are always pathological. | Alkaline phosphatase is reduced Alkaline phosphatase is a substance whose concentration in the blood is used to assess the condition of the body. Often, the analysis reveals a change in alkaline phosphatase. Find out why enzyme levels are low? How to bring alkaline phosphatase levels back to normal. |
Decoding the analysis result
Depending on the degree of deviation of the test results from the norm, one can judge whether the child has a disease. The table shows the most significant indicators for diagnosis and possible reasons for their changes.
| Index | Level up | Level reduction |
| Protein |
|
|
| Albumen |
|
|
| ALaT and ASaT |
| |
| Cholesterol |
|
|
| Glucose |
|
|
| Bilirubin |
| |
| GGT |
| |
| C-reactive protein |
| |
| Urea |
| |
| Creatinine |
| |
| Lipase |
| |
| Amylase |
|
|
| Uric acid |
| |
| Alkaline phosphatase |
| |
| Creatine kinase |
|
- Biochemistry results taken from different laboratories may vary significantly. In this regard, when deciphering the analysis, it is necessary to build on the standards indicated on the form of a particular laboratory.
- A week before the test, it is advisable to avoid taking medications that affect metabolic processes. If this is not possible, be sure to tell your doctor what medications you are giving your child.
Only an experienced specialist can decipher blood biochemistry. It is impossible to judge the child’s condition from just one analysis. For a correct diagnosis, other studies are necessary, such as a clinical blood test, computed tomography, ultrasound and others.
Why donate blood for a general test?
Human blood is made up of many different components. If a bacterial or viral infection enters the body, the amount of substances may change. To confirm or refute the initial diagnosis, the doctor takes the material for a general analysis (GA). The behavior of hormones and enzymes is also revealed, on the basis of which the doctor diagnoses any disease.
Indications for donating blood in children are:
- complaints about symptoms that the child had not previously shown;
- complications of diseases that last a long time;
- determination of the activity of drugs previously prescribed for treatment;
- handing over material before vaccination or entering kindergarten.
The reasons why a child undergoes a general test includes disease prevention. This check is done once a year.
In adults, such a study is not necessary, since a person’s immunity and protective forces are already formed by this age. The exception is patients with reduced immunity. More often, testing is carried out when applying for a new job, passing a medical examination and pregnancy.
Before donating biomaterial, the patient needs to prepare:
- 12 (at most)
 hours before visiting the clinic, refuse to eat. Tea, coffee and juices are considered food. Drinking water is not prohibited. In exceptional cases, you can eat an apple or drink unsweetened tea 60 minutes before donating blood.
hours before visiting the clinic, refuse to eat. Tea, coffee and juices are considered food. Drinking water is not prohibited. In exceptional cases, you can eat an apple or drink unsweetened tea 60 minutes before donating blood. - Stop taking antibiotics and other medications 2 weeks before the test.
- Before the procedure (30 minutes before), avoid hot baths, psychological stress and physical exercise.
- Do not smoke on the day of submitting your biomaterial.
- If you have an ultrasound, x-ray, physiotherapy, rectal examination or reflexology scheduled on the day of your blood draw, donate blood first. The listed procedures may distort the initial indicators.
The ideal time to visit a laboratory technician is from 7 to 12 am. This is the period immediately after sleep, when hunger is not yet so noticeable. In addition, indicators can vary significantly throughout the day.
Blood test for group and Rh factor: how to take it, where does the biomaterial come from, how much does it cost?
A blood test can tell you almost everything about the human body.
In addition to identifying hidden inflammatory processes, assessing hormonal levels and the functioning of various organs, blood can be used to determine whether its owner belongs to a certain group and Rh factor.
When and in what cases may such a determination be required? What can a person's blood type tell us? Can this indicator change throughout life?
Blood type and Rh factor: what is it and why determine them?
Blood is a mobile connective tissue of the internal environment of the body, consisting of a liquid component (plasma) and cellular material (erythrocytes, leukocytes, platelets). There are specific proteins (antigens) on the surface of red blood cells.
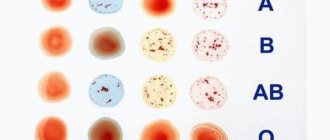
Plasma contains certain antibodies that bind to a specific antigen on the surface of the red blood cell. This combination forms agglutinogens, which are used to determine the blood type.
There are 2 options for the formation of agglutinogens - type A and type B.
In medical practice, blood type is determined using the ABO system. In accordance with this system, a person inherits from his parents genetic material corresponding to one of four groups:
- group 0 (I) – agglutinogens of types A and B are absent;
- group A (II) – red blood cells contain only agglutinogen A;
- group B (III) – red blood cells contain only agglutinogen B;
- group AB (IV) - agglutinogens of types A and B are present on red blood cells.
Rhesus is also inherited at the genetic level. On the surface of red blood cells in most people (85% of cases) there is a specific Ph antigen. Such a person is called Rh positive. The remaining 15% of people whose red blood cells do not have the Ph antigen are called Rh negative.
A test for Rh factor and blood group is required in the following cases:
- before performing surgical operations;
- before hemotransfusion (blood transfusion);
- during pregnancy planning.
Why do you need to know your group and Rh? During pregnancy, the Rh factor plays an important role. If one of the spouses is Rh negative, there may be a conflict between the blood of the mother and the child.
As a result, the pregnant woman’s body produces protective antibodies against the fetus, which are extremely dangerous for the unborn child.
An expectant mother with a negative Rh factor needs to donate blood every month for alloimmune antibodies in order to control the process of bearing a child and in time to prevent the threat of miscarriage in the event of a Rh conflict.
During blood transfusion, the group and rhesus play a particularly important role. If the recipient is transfused with donor blood of a different type, his immune system will begin to reject foreign blood cells, which can be fatal. Group I donors are considered universal - their blood does not contain antigens A and B, therefore it is suitable for absolutely everyone.
Can a child’s blood type differ from that of its parents (for more details, see the article: What blood type can a child have: determination using a special table)? Yes. For example, a mother with group A (II) and a father with group B (III) have a 50% chance of having a child with group AB (IV). The child's Rh factor can be any, even if both parents have the Ph+ antigen in their blood.
How is the group and Rh factor analyzed?
Where is the best place to get tested? No difference. The donation of biomaterial can take place either in a clinic at your place of residence or in any paid clinic where laboratory services are provided.
Preparing to donate blood
No special preparation is required before donating blood. The biomaterial is taken from a vein, the manipulation is performed quickly and painlessly. You can donate blood at any time of the day, not necessarily on an empty stomach. Drinking water before the test is allowed. Taking medications does not affect the results. The exact preparation rules can be found at the clinic.
Collection of biomaterial and its examination
The study requires the patient's venous blood. The material is taken into a test tube with ethylenediaminetetraacetic acid (EDTA). Blood sampling time is a few seconds.
Before drawing, the health care provider may ask the patient to pump his fist a little so that blood quickly gets into the tube.
After the puncture, the venipuncture site is treated with sterile gauze; at the patient’s request, a bactericidal patch can be applied.
When is the result known and are errors possible?
How long does the research take to complete? Typically, a blood test for Rh factor is completed within 1 working day, not counting the day of blood collection. The exact time for performing the analysis depends on the distance and workload of the laboratory. Some medical centers provide a service for express delivery of results - within 2 hours from the moment of blood collection.
Modern medical equipment using robotic technology in most medical laboratories eliminates the possibility of error. A unique barcode is attached to each tube, from which the analyzer reads the information before performing the analysis.
In rare cases, the result may be given in the format “a weakened variant A2 has been identified”, or “a weak Rh antigen has been identified”. This is not an error and is due to the individual characteristics of the body. In this case, it is recommended to donate blood again and seek advice from your doctor.
What indicators correspond to the norm?
First of all, the analysis determines the amount of a complex protein - hemoglobin, contained inside red blood cells. A woman’s blood should contain 120–140 g/l of hemoglobin.
In males, this figure is normally higher - it is 130 - 160 g/l. The amount of hemoglobin in the blood of infants ranges between 90 and 140 g/l.
But in a preschool child, the complex protein that transports oxygen to tissues increases - from 105 to 150 g/l.
The norms for the content of red blood cells in the blood reflect the following figures: in the hemogram of men - 4.2 - 6 * 1012/l, and in women - 3.7 - 5.5 * 1012/l.
Quantitative indicators of red blood cells in children depend on age. For a newborn child, they should fit within the range of 2.6 to 4.6 * 1012/l. In the blood of preschoolers and schoolchildren, 4 – 5.2 * 1012/l of red blood cells are normally determined.
The hematocrit level is measured as a percentage. In children within a year after birth it should be at least 29%, but over 40.
In the blood of healthy preschool children, 35 (+/- 5)% hematocrit is usually observed. The norms for the percentage of red blood cells in the blood for men and women are 39–49% and 35–45%, respectively.
The blood of men and women can contain 4 – 9 * 109/L white blood cells. The norms for this indicator for children differ from the norms for adults.
The allowed content of leukocytes in the blood of infants is 5.5 - 12 * 109/l. In one-year-old children and even older children, white blood cells cannot be less than 5*109/l.
Granular leukocytes (granulocytes) should be present in the blood in an amount of 47–70 percent (of the total number of different leukocytes).
Photo:
A positive reading of a complete blood test includes a certain percentage of lymphocytes: in children from one to 6 years old - 42%, infants - 61%, adults - at least 34% of all blood elements. The normal level of monocytes in the blood is from 0.1 to 0.8 * 109/l.
Indicators such as the scale of distribution of red blood cells, their sedimentation rate and the average volume of one red blood cell must also meet the standards. 11.5 – 14.5% is the normal value for the spread of red blood cells in children and adults. 80 – 100 fl is an acceptable figure for the average volume of a red blood cell.
The ESR indicator depends on gender and age: in babies under one year old it is 4 – 10 mm/h, in preschool children – 4 – 12 mm/h, in women – no more than 20 mm/h, in men – maximum 15 mm /h.
Where is blood taken for blood type and Rh factor - rules for collecting material, preparation
Blood is a liquid that circulates throughout the human body. Currently classified according to the presence or absence of antigens that are contained on the surface of red blood cells.
In 1900, the scientist Landsteiner discovered four blood groups. Currently, there are many classifications, but the most commonly used division is by groups and Rh. The group is inherited from parent to child and does not change throughout life.
In addition to differences in groups, blood is divided into two types based on the Rh factor. 85% of the total population of the Earth is positive and only 15% is negative.
But where is blood taken to determine blood type and Rh factor? Why does an ordinary person need knowledge of these characteristics? The answers to these questions are simple.
The meaning of the group and Rh factor
Knowledge of the characteristics is necessary if there is a risk of blood loss. In case of such a problem, only donor material can replenish the body's reserves.
And in this case, both the group and the Rh factor are important, because:
- If the characteristics of the patient’s blood and the donor’s blood do not match, rejection and death occur.
- Incompatibility of Rh factors is deadly, even if transfusion occurs from group to group.
Doctors can determine these indicators in extreme conditions, but this will be a waste of time.
Knowing the characteristics is important for transfusions, for preparing for organ transplants, for operations, and for pregnant women.
Patients ask: where do they get blood for blood type and Rh factor? The answer is simple: if the person is an adult, the sample is taken from a vein, since the venous one carries more information and contributes to the accuracy of the results.
Before taking the fence, it is important to follow the rules:
- You should not eat before the test.
- Carry out the procedure in the morning.
- Stop taking medications several weeks before the procedure. If discontinuation of drug therapy is not recommended, inform the doctor who is taking the sample which substances you are taking, in what dosage and for how long.
- A few days before the test, limit your alcohol consumption and stop smoking.
- Two days before the procedure, minimize physical activity and stress.
- The day before the test, you should not eat fatty or fried foods.
To find out your blood type and where the blood is taken from, you should go to a clinic where the test will be performed. But most often an analysis of venous fluid is performed.
You can take blood for a blood group test from a newborn baby from the heel or big toe. To determine Rh and group, plasma, platelets and red blood cells are removed by centrifugation.
Analysis during pregnancy
One of the important indicators that you should pay attention to when planning pregnancy is the compatibility of the characteristics of the parents’ biomaterial, and whether there are any differences in their Rh.
This is important because:
- If the Rh factors of the parents and the child are incompatible, Rh may be opposite to the maternal one, which will cause a Rh conflict.
- Differences in the blood characteristics of spouses will cause infertility in a woman.
Before conception, it is recommended that both parents undergo testing. The Rhesus conflict may not appear, and the newborn will see the world without problems, but it is not recommended to take risks.
But what if the need for analysis arose during pregnancy, where is blood taken for Rh factor and group in pregnant women? The sampling rate is still the same: from a vein.
In this case, it is important to check whether the characteristics of the biomaterial “mother and fetus” match. In the early stages, the protein from the child’s red blood cells strives to enter the mother’s blood and, if they have a discrepancy in Rh indicators, a process occurs that the mother’s body rejects her child – a Rh conflict.
How the research works
In the laboratory, an analysis is carried out using a test reagent - anti-Rhesus serum. The process is simple and consists of several steps:
- The blood is mixed with a polyglucin solution and placed in a test tube.
- After this, blood is dripped into the test tube and mixed carefully.
- The test tube is placed in a centrifuge for some time.
- After centrifugation, a visual assessment of the results is carried out: if a precipitate is observed, saline solution is added to the test tube.
- If flakes form and the liquid turns white, it is Rh positive. If the fluid is pale pink, it is Rh negative.
The process is quick and doesn't take much time, but the benefits are significant.
The analysis procedure is simple, and at the current level of development of medicine, it is safe. The answer to the question: where is blood taken for Rh factor and group, should not be scary. Taking biomaterial from a vein is not dangerous; it is a standard procedure that will serve an important role during transfusion or if you decide to have a child.
Loading…
Source: https://dlja-pohudenija.ru/serdcze/analiz-krovi/otkuda-berut-krov-na-opredelenie-gruppy-krovi-i-rezus-faktora-pravila
How is the analysis carried out?
The test is taken in the morning on an empty stomach. Even if water, food or toothpaste gets into the mucous membrane of the body, this can change the readings and confuse the doctor. Even stress on the way to the hospital can change your blood picture.
First, blood is drawn to determine the erythrocyte sedimentation rate, as well as the level of hemoglobin, then to determine the number of leukocytes and red blood cells. To do this, blood smears are made on slides and a detailed analysis of the blood and its cells is carried out under a microscope.
Different laboratories have their own standards regarding different blood parameters, so only the doctor who is treating you knows how to decipher the blood test that belongs to you.
Where is the best place to get tested?
Taking blood from a vein from a child is certainly an alarming event. There are painful sensations, but they are short-lived. The most important thing for a parent is to remain calm, find a qualified professional and, if necessary, use an anesthetic.
When looking for a good medical facility, it is best to seek advice from other moms and ask for recommendations. The most important thing is to shower the child with warmth and care after the blood test, forgetting the unpleasant but fleeting procedure.
 hours before visiting the clinic, refuse to eat. Tea, coffee and juices are considered food. Drinking water is not prohibited. In exceptional cases, you can eat an apple or drink unsweetened tea 60 minutes before donating blood.
hours before visiting the clinic, refuse to eat. Tea, coffee and juices are considered food. Drinking water is not prohibited. In exceptional cases, you can eat an apple or drink unsweetened tea 60 minutes before donating blood.