Disease verification and treatment
Diagnosis of pulmonary edema must be made quickly. It determines further tactics. A set of examinations to verify the diagnosis includes:
- collection of patient complaints,
- history of life and illness,
- general examination,
- additional research methods.
During a general examination, the doctor pays attention to the color of the skin, the involvement of additional muscle groups in the breathing process, the position of the patient, changes in the fingers, and the frequency of respiratory movements.
Auscultation of the lungs reveals a weakening of vesicular breathing in the lower parts, and isolated dry or moist rales are possible. This picture is typical for cardiac asthma. With alveolar pulmonary edema against the background of weakened breathing, moist rales of various types (small and large bubbles) are heard throughout all pulmonary fields. Their tonality is different. In the lower sections, with a severe course of the process, breathing cannot be heard.
Additional examinations for pulmonary edema and diagnosis of underlying disorders are of an auxiliary nature. They confirm decompensation of a chronic disease. The mandatory minimum includes:
plain X-ray of the chest organs in a direct projection,- ECG in 12 standard leads,
- general blood and urine tests,
- determination of renal and hepatic parameters during biochemical studies,
- an analysis for troponins, CPK and CPK-MB (markers of myocardial necrosis) is mandatory, since infarction is the most common cause of pulmonary edema,
- pulse oximetry (determining blood oxygen saturation).
Establishing the cause of the development of a critical condition and the underlying disease determines how to treat pulmonary edema in the future and prevent its occurrence.
First aid
A sudden deterioration in health does not always occur within walking distance of medical facilities. First aid is provided by strangers who do not have special education. What can and should be done in case of pulmonary edema is an algorithm of actions that can temporarily ease the patient’s well-being:
call an ambulance,- unbutton your shirt collar or remove clothing that restricts your breathing,
- provide a flow of fresh air,
- ensure a semi-sitting position,
- If your health deteriorates after inhaling toxic fumes at work, take the victim outside.
Help from medical personnel
The doctors who arrived at the scene will continue to stop the attack if this could not be done before they arrived. Emergency care for cardiac asthma consists of administering medications:
- A solution of strophanthin or korglykon is administered intravenously;
- Eufillin should be injected slowly into a vein, but only if there are no contraindications: low blood pressure, rapid pulse, paroxysmal tachycardia;
- Oxygen inhalations, which are done for a long time and repeated if necessary;
- The administration of morphine is indicated for pronounced excitation of the respiratory center;
- When congestion is detected in the lungs, a bolus solution of furosemide is injected into a vein.
The rest of the treatment is prescribed after a study has been carried out, which will identify the disease and its place in the classification of the occurrence of cardiac asthma.
Diagnostic techniques
Diagnostic methods for making a correct diagnosis are very important so as not to confuse cardiac asthma with equally dangerous, but other pathologies. To confirm the diagnosis, the following diagnostic techniques are used:
- Measuring blood pressure indicators;
- Tapping the chest in the area above the lungs;
- Listening to the lungs, which allows you to detect the presence of wheezing, indicating the onset of swelling of the lung tissue;
- Listening to heart sounds, which in the presence of pulmonary wheezing will be barely audible;
- The appearance of additional heart sounds that are absent in a healthy person;
- Counting the number of heart beats per minute.
The doctor needs to conduct hardware tests that will confirm or refute the preliminary diagnosis:
- ECG;
- Echocardiography;
- Ultrasound duplex scanning;
- X-ray in 3 projections.
Based on the examination, adequate treatment will be prescribed, after which you need to consult a cardiologist. He will supervise the main therapeutic course and make intermediate prescriptions of medications so that the attack does not recur.
Specifics of preventive measures
It is difficult to predict how an attack of cardiac asthma will end, since its outcome will depend entirely on the pathology that caused it. In the case of a “cardiac” factor, the prognosis is often unfavorable. However, strict adherence to medical prescriptions, properly selected drug therapy, daily routine and nutrition allow patients after an attack not only to avoid the manifestation of new serious conditions, but also to achieve lasting satisfactory well-being.
Prevention of attacks of cardiac asthma is timely seeking medical help in the presence of cardiovascular diseases, as well as strict adherence to medical instructions in the form of regular taking of prescribed medications.
It is important to take walks in the fresh air every day, correctly distributing hours of rest and work. And gentle physical activity will help improve blood circulation, well-being and mood.
Source
Technique for applying tourniquets
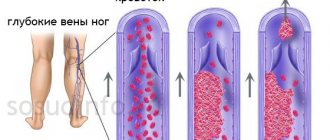
Tourniquets, or tourniquets, are applied to the lower extremities in order to deposit part of the venous blood in them. It is temporarily excluded from the bloodstream to relieve the heart until alveolar and interstitial edema are removed with special diuretics. The prolonged presence of tied tourniquets on the legs can lead to vein thrombosis, so the condition requires urgent hospitalization and treatment. It should also be remembered that the method is contraindicated in case of exacerbation of thrombophlebitis.
The application of tourniquets to the legs can retain 600-800 ml in each limb.
The manipulation technique is as follows: the patient must be placed in a semi-sitting or sitting position so that the legs are down, that is, hanging or standing on the floor. Before applying tourniquets, the patient's blood pressure must be measured. The patient must sit in this position for 10 minutes, after which tourniquets are applied. You can use nylon stockings or elastic bandages as tourniquets.
The place where the tourniquets are applied is on the hips, about 15 cm below the inguinal fold, and on the arm at the top of the shoulder (about 10 cm below the head of the humerus). Venous tourniquets are tied over a napkin or linen on both legs at the same time. It is necessary to ensure that the limbs do not turn pale under the tourniquet, and also change the application site every 20 minutes.
When tourniquets are applied correctly, the limbs become bluish-purple due to venous congestion. It is also necessary to check the pulsation of the arteries - it should not be below the tourniquet. To relieve an attack when the upper pressure is at least 100 mm Hg, use the Nitromint inhaler or give the patient Nitroglycerin. These drugs dilate blood vessels and help reduce preload on the heart.
While the tourniquets are tied on the legs, decongestant therapy is carried out in a hospital setting. To eliminate edema, the diuretic Lasix (Furosemide) is used.
Under pressure, oxygen mixed with alcohol vapor is injected into the lungs using an artificial respiration apparatus. Oxygen inhibits the respiratory center in the brain, eliminating shortness of breath and hypoxia. Alcohol prevents mucus from foaming. Antifomsilan can be used for this purpose. Sputum aspiration is carried out.
Narcotic analgesics also eliminate the excitability of the respiratory center caused by plasma sweating and alveolar pulmonary edema. The opioid painkiller Talamonal is used in a solution of glucose or sodium chloride. In some cases, neuroleptanalgesia is performed using Droperidol with Fentanyl. Morphine is sometimes used. The use of analgesics, especially in the elderly, is carried out with caution to avoid respiratory arrest.
Antihistamines are also used to relieve pulmonary edema during anaphylactoid reactions and intoxications: Suprastin, Diphenhydramine. If possible, block the stellate ganglion using novocaine. Spinal anesthesia is also effective for pulmonary edema. After removing the alveolar edema, it is necessary to gradually loosen and remove the tourniquets.
Diseases
Treatment.
The success of therapy for pulmonary edema depends primarily on the urgency of the measures taken. Treatment should begin immediately, be intensive, comprehensive, rational, with the obligatory implementation of general measures, namely:
- give the patient a semi-sitting or sitting position in the
arteries was preserved. After the swelling is relieved, tourniquets
PULMONARY EDEMA
493
they are allowed in slowly due to the danger of a sharp increase in the mass of circulating blood. In case of thrombophlebitis, the application of tourniquets is contraindicated. Hot foot baths may be used;
the patient must be provided with fresh air;
if edema develops against the background of elevated or normal blood pressure, bloodletting from the cubital vein can be performed. After bloodletting, the volume of circulating blood decreases by 200-400 ml, which reduces blood flow into the lesser circle and reduces the pressure in the pulmonary capillaries;
organize immediate aspiration of foam from the upper respiratory tract, then inhalation of an air-oxygen-alcohol mixture, if possible, under high pressure (96% alcohol is added to the humidifier for adults and 30% alcohol solution for children), or inhalation of a defoamer with antifungal silane - 1 ml of 10% alcohol solution. Inhalations of alcohol vapor are carried out for 10-15 minutes, alternating them with inhalations of pure oxygen or an oxygen-air mixture. Foamy fluid from the upper respiratory tract is aspirated through a nasal catheter using an electric suction device.
Treatment measures should be carried out taking into account the premorbid state and be aimed at eliminating or at least reducing the effect of the main causes that led to this complication. Further treatment tactics are determined by: the underlying disease, the effectiveness of primary treatment measures, and the peculiarities of circulatory compensation processes in each individual case. Therefore, further therapy includes measures aimed at restoring airway patency, compacting alveolar-capillary membranes, reducing hydrostatic pressure in the vessels of the pulmonary circulation, reducing blood volume, dehydration of the lungs, reducing the effect of biologically active substances, improving myocardial contractility, eliminating hypoxia, normalizing tissue metabolism.
In all cases, drug treatment for conscious patients with pulmonary edema should begin with the normalization of their emotional background, often with the elimination of pain or the removal of the reaction to a stressful situation, which are often the trigger for the development of pulmonary edema. For this purpose, it is advisable to administer slow intravenous morphine - 0.5-1 ml of 1% solution per 10-15 ml of isotonic sodium chloride solution or 5% glucose solution in combination with antihistamines (1-2 ml of 1% diphenhydramine solution, 2% suprasti solution - or 2.5% pipolfen solution). Morphine in small doses reduces
^ CRITICAL CONDITIONS IN THE CLINIC OF INFECTIOUS DISEASES
494
excitability of the respiratory center, causing a slowdown and increase in the depth of respiratory movements, and also reduces feelings of fear and anxiety. At the same time, morphine, by dilating the veins and arterioles, reduces the return of venous blood to the heart, reduces pressure in the pulmonary artery, peripheral vascular resistance and blood pressure. The side effects of morphine - activation of the vomiting center and increased bronchospasm - are eliminated to some extent by combination with 2 ml of a 0.25% solution of droperidol, which is slightly different in action. It reduces peripheral resistance by blocking α-receptors, moderately increasing minute blood volume. When signs of depression of the respiratory center appear, which is sometimes observed when morphine is prescribed, 0.4-0.8 mg (1-2 ml) of naloxone, an opiate antagonist, is administered. You can prescribe 2-4 ml of a 0.5% solution of seduxen (Relanium) or 2 ml of a 2.5% solution of diprazine. Administration of morphine is contraindicated in case of bronchospasm and in patients with low breathing volume (hypoventilation). For patients with low blood pressure, it is preferable to prescribe sodium hydroxybutyrate intravenously, 20-30 ml of a 20% solution (4-5 g of the drug) very slowly - over 8-10 minutes. Sodium hydroxybutyrate stabilizes blood pressure and helps normalize it. To normalize the emotional background, hexenal is sometimes used - 1-2 ml of a 1-2% solution intravenously or sodium thiopental - 20 ml of a 2% solution intravenously under blood pressure control.
Sedative therapy leads to normalization of the content of catecholamines in the blood, and consequently, peripheral vascular spasm is significantly reduced, blood flow to the lungs is reduced, the outflow of blood from the pulmonary circulation is stimulated, and thus the filtration of tissue fluid through the alveolar-capillary membrane is reduced. Sedatives also reduce the intensity of metabolic processes, which makes hypoxia easier to tolerate.
Narcotic analgesics are contraindicated in case of cerebral edema, acute obstruction of the respiratory tract, pregnancy, chronic cor pulmonale, and antipsychotics are contraindicated in case of severe organic lesions of the central nervous system.
To dehydrate the pulmonary parenchyma, unload the pulmonary circulation by reducing the volume of blood volume, use the diuretics lasix (furosemide) at a dose of 80-160 mg intravenously in a bolus (better in fractions - 40-80 mg each to avoid necrosis of the renal tubules) or uregit (ethacrynic acid) at a dose of 50 —150 mg. In cases of severe hemodynamic disturbances, diuretics are indicated after normalization of blood pressure. Diuresis should not be very abundant (no more than 2-3 in the first day) due to the possibility of electrolyte disturbances. After intravenous administration of Lasix, the positive effect develops within a few minutes and lasts for 2-3 hours.
PULMONARY EDEMA
Osmotic diuretics (urea, mannitol, mannitol, etc.) are not recommended for use to relieve acute pulmonary edema. In the first phase of their action, these drugs can increase the volume of circulating fluid, and therefore increase pulmonary edema, so they are prescribed for prolonged pulmonary edema, when there is no effect from the administered drugs; urea is administered at the rate of 1 g of dry matter per 1 kg of body weight in a minimum amount of liquid or mannitol at the rate of 1-1.5 g/kg, while the daily dose should not exceed 140-180 g.
Osmotic diuretics are used in combination with Lasix. The diuretic effect when prescribing osmotic diuretics usually occurs within 15-30 minutes, reaches a maximum 1-1.5 hours from the start of the solution and lasts 5-6 hours or more (up to 14 hours).
A significant reduction in blood volume in the pulmonary vessels can be achieved with the help of short- and medium-acting ganglion blockers. However, they are administered only under the control of blood pressure, since, by expanding the veins of the systemic circulation, they deposit part of the circulating blood in them, and therefore reduce systemic blood pressure. This group of drugs includes arfonade and pentamidine. Their administration is stopped at blood pressure 120 mm Hg. Art. Arfonad (hygronium) is administered intravenously at a dose of 250 mg of a 1% solution in 250 ml of isotonic sodium chloride solution or 5% glucose. Initially, the drug is administered at a rate of 80-100 drops per 1 minute, and as blood pressure decreases, the rate of administration is reduced to 10-15 drops per 1 minute. Pentamidine (50-100 mg) is injected into a vein in fractions with a syringe. To do this, 1-2 ml of a 5% solution of the drug is diluted in 20 ml of isotonic sodium chloride solution and administered intravenously in 3-5 ml doses every 5-10 minutes. Benzohexonium (10-40 mg) or nano-fin (50-100 mg) is also prescribed; they are administered slowly intravenously with a syringe in 20 ml of a 40% glucose solution under blood pressure control; administration is stopped at 110-120 mmHg. Art. Reducing pressure in the pulmonary circulation can be achieved using nitroglycerin preparations. Nitroglycerin is administered very slowly intravenously, 1 ml of a 1% alcohol solution diluted in 290-300 ml of a 5% glucose solution, or 1-2 tablets are given under the tongue. Transfusion is carried out under blood pressure control. A similar effect can be achieved by prescribing nitrosorbide at a dose of 20-30 mg (2-3 tablets) every 4-5 hours.
Their action is based on reducing venous tone and venous return to the heart, relieving pulmonary vasospasm and reducing overall pulmonary resistance; they reduce shortness of breath, suffocation, cyanosis. One should keep in mind the possibility of using ganglion blockers and peripheral vasodilators
not only with high, but also with moderately elevated and even normal blood pressure.
^ CRITICAL CONDITIONS IN THE CLINIC OF INFECTIOUS DISEASES
496
The use of aminophylline for pulmonary edema is advisable only in cases of concomitant bronchospasm, cerebral edema with the development of bradycardia, mitral stenosis, and hypertensive crisis. Eufillin is administered intravenously slowly (10 ml of 2.4% solution). The use of aminophylline is limited by its side effects: it causes tachycardia, increases the myocardial oxygen demand, and activates the respiratory center.
The use of cardiac glycosides as agents that improve myocardial contractility and reduce heart rate in pulmonary edema is limited due to possible toxic effects and increased contractile function of the right ventricle. They are used only for pulmonary edema due to chronic heart failure, cardiogenic shock during myocardial infarction in small doses (strophantine 0.25-0.5 ml of 0.05% solution or cor-glycon 0.5-1 ml 0.06 % solution intravenously slowly under heart rate control).
When pulmonary edema occurs at low blood pressure, attempts to stop it with the help of sedatives, diuretics, and ganglionic locators do not always give a positive result. In these cases, peritoneal dialysis or hemodialysis is used to remove excess fluid from the body.
During intensive care, measures should be taken to ensure the necessary oxygen content in the air inhaled by the patient, as well as to reduce foam formation. Sometimes hyperbaric oxygen therapy is performed.
An important component of intensive care for pulmonary edema is to counteract filtration in the alveoli and impede the passage of blood transudate from the pulmonary capillaries into them, which is achieved by spontaneous breathing with expiratory resistance (5-10 mm H2O) with positive end-expiratory pressure ( use devices RO-2, RO-4, AND-2, “Engstrem”, etc.).
In case of pulmonary edema due to anaphylactic shock, severe intoxication with medicinal and industrial poisons, acute hemolytic crisis, transfusion of incompatible blood, malaria, and some blood diseases, it is necessary to prescribe prednisolone in a dose of 100-150 mg or more or hydrocortisone in a dose of 200-350 mg intravenously. isotonic sodium chloride solution or 5% glucose solution. Glucocorticoid drugs are also prescribed to reduce swelling of the mucous membrane of the respiratory tract (prednisolone 40-60 mg or more or hydrocortisone 125 mg intravenously).
In the complex treatment of pulmonary edema in infectious diseases, the etiological factor of the underlying disease should be taken into account and adequate etiotropic therapy should be continued.
PULMONARY EDEMA
497
To cleanse the respiratory tract of viscous sputum (viscosity is caused by acid glycoprotein fibers), trypsin, chymotrypsin or their combination - chymopsin - are indicated. When the secretion is purulent (containing ribonucleide fibers), ribonuclease and deoxyribonuclease have a more pronounced liquefying effect. Mucolytic agents are administered directly into the respiratory tract in the form of an aerosol or through a tracheal tube (single dose 25-50 mg, dissolved in 3 ml of isotonic sodium chloride solution or 4% sodium bicarbonate solution). The administration of proteolytic enzymes for hemoptysis is contraindicated. The aerosol contains antihistamines (suprastin, diphenhydramine), purine derivatives (aminophylline), bronchodilators (ephedrine hydrochloride, naphthyzine, isadrin), anticholinergics (atropine sulfate), as well as officinal mixtures (solutan or efatin, etc.) . If necessary, antibiotics, glucocorticoids or other chemotherapy drugs are included in the mixture. Inhalations are carried out using inhalers that provide the formation of fine aerosols that easily penetrate not only into the upper, but also into the lower parts of the respiratory tract, up to the bronchioles and alveoli.
An effective cough is essential to maintain tracheobronchial patency. Cough stimulation is facilitated by changing the position of the patient's body in bed, percussion-vibration massage of the chest, pressing on pain points along the trachea, and using the IKAR-2 artificial cough apparatus. In these cases, narcotic analgesics (morphine, promedol, tecodin, fentanyl, etc.) that suppress cough are prescribed with great caution.
The development of pulmonary edema against the background of laryngospasm, stenotic edema of the larynx requires catheterization of the trachea and bronchi and therapeutic laryngotracheobronchoscopy. Medicines are administered endotracheally after preliminary washing of the tracheobronchial tree with isotonic sodium chloride solution heated to 38 °C or 4% sodium bicarbonate solution (3-5 ml each), which helps thin the sputum. If necessary, repeat therapeutic laryngotracheobronchoscopy is performed. In the complex treatment of laryngospasm, anticonvulsant therapy, which consists of prescribing seduxen (2 ml 0.5 %
solution) with sodium hydroxybutyrate (20 ml of 20% solution, administered intravenously slowly over 6-10 minutes), as well as lytic mixtures of different compositions (aminazine 2.5% solution 2 ml, promedol 2% solution 2 ml , diphenhydramine 2% solution 2 ml).
Thus, taking into account the above, the provision of emergency
32 — 2-3077
^ CRITICAL CONDITIONS IN THE CLINIC OF INFECTIOUS DISEASES
help with pulmonary edema can be recommended in the following order:
giving the patient a semi-sitting or sitting position in bed;
conclusions
With the correct technique, applying tourniquets to the lower limbs and one of the arms is a simple and effective method for reducing hydrodynamic pressure in the pulmonary circulation. Reducing venous return by tying tourniquets relieves the heart, but is a temporary measure. A patient with alveolar pulmonary edema requires urgent hospitalization and treatment in a hospital. This condition is life-threatening and is fraught with complications, such as fibrosis and the development of infection! The hospital is treating edema with diuretics. After the swelling is removed, the tourniquets are first loosened and then slowly removed.
First aid for pulmonary edema: how to apply a tourniquet
Timely and professional first aid for acute heart pathology helped save the lives of a large number of patients. The list of necessary techniques necessarily includes the technique of applying venous tourniquets for pulmonary edema. Quite often, pathology develops in patients with heart disease in places where it takes a certain amount of time to provide specialized care to the patient. If among the people around him there is a person who has resuscitation skills, then this will give a certain chance of saving the life of the victim.
Complications in the absence of proper assistance
Pulmonary edema is always considered a serious and dangerous condition that requires urgent care and professional therapy.
Consequences and complications of failure to provide first aid for pulmonary edema:
- Edema can develop into a fulminant form , which most often occurs in the presence of decompensated heart disease. In this case, all manifestations of the disorder begin to develop very quickly, and it is extremely rare to save a person’s life.
- Respiratory depression . In most cases, this condition appears due to pathology of a toxic nature, which occurs during poisoning with drugs, gases, and poisons. Quite often, such manifestations are observed when using narcotic painkillers when the dosage is exceeded, but other drugs, for example, barbiturates, can also cause a similar phenomenon.
- Asystole . This is what is called in medicine when the heart stops working. If assistance is not provided against the background of severe diseases of the cardiovascular system, a person may completely stop cardiac activity.
- Hemodynamic instability , expressed in a decrease or sharp increase in pressure. Such changes can be alternating in nature, but this condition has a very unfavorable effect on the condition of the walls of blood vessels, and greatly complicates the implementation of therapeutic measures.
- Blockage of the respiratory tract . This condition can occur due to the discharge of a large amount of sputum in the form of foam, which significantly impairs breathing and gas exchange.
- Cardiogenic shock . This condition is characterized by severe failure of the heart, or more precisely, the left ventricle. In this case, the level of blood supply to organs and tissues is greatly reduced, which creates a real threat to the patient’s life. The pressure in this state drops below 90 mm Hg, the skin turns blue due to excess carbon dioxide in the tissues, and a significant decrease in the number of urinations occurs.
Causes and clinical picture of pulmonary edema
The main reason for the development of pulmonary edema is the sweating of the liquid part of the blood from the pulmonary vessels into the alveoli. Typically, such a pathology is caused by congestion in the pulmonary circulation.
The etiology of this acute process divides its causes into two large groups:
- Heart disease that can cause pulmonary edema. These include acute myocardial infarction, aortic aneurysm, heart defects and hypertension.
- If the pathological process is caused by non-cardiac causes, then we can talk about the non-cardiogenic nature of the problem. Pulmonary edema can be a consequence of pneumothorax, acute respiratory failure, severe pneumonia, allergic reactions, etc. Regardless of the reasons for the development of this formidable pathology, the clinical manifestations will almost always be the same.
The feeling of suffocation forces the patient to take a forced position in bed - sitting and with his legs down. The respiratory rate can reach 35 - 40 per minute.
When the clinical picture of pulmonary edema develops, the patient’s cough is initially dry, but after 10-15 minutes the production of foamy sputum mixed with blood begins. At the beginning of the process, moist rales in the lungs can only be heard with the help of a phonendoscope; as conditions worsen, wheezing breathing can be heard at a distance of 3 - 5 meters.
Blood oxygen saturation sharply decreases, which leads to the development of cyanosis of the mucous membranes and skin. Brain cells also suffer from hypoxia, which is characterized by agitation, a feeling of fear of death and a lack of criticism of the patient’s condition.
Cause-and-effect relationships
Cardiac asthma refers to functional changes in the functioning of the left ventricular myocardium. These deviations are associated with stagnant blood in the pulmonary circulation. Pathology can develop into pulmonary edema. Moreover, its occurrence can be almost instantaneous, which is always a consequence of a rapid fatal outcome.
An attack is always accompanied by suffocation. The heart works in an increased mode, which is why tachycardia develops and diastolic blood pressure increases significantly. Due to acute lack of air, the patient panics and fears possible death. Panic attacks make the situation even worse: a strong dry cough increases the feeling of suffocation, the person’s skin turns blue, and he begins to choke.
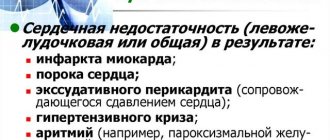
Factors that cause cardiac asthma can be divided into 2 groups:
- Related to cardiac activity;
- Not related to cardiac activity.
The main reasons that cause a dangerous cardiac condition are cardiac pathologies caused by a violation of the left side of the heart. These include the following pathologies:
- Acute form of left ventricular heart failure;
- Chronic form of left ventricular heart failure;
- Consistently high blood pressure;
- Myocardial infarction;
- Heart defects capable of decompensation;
- Atrial fibrillation;
- Intracavitary cardiac tumor.
There are factors that cause pathological changes in cardiac and pulmonary activity that are not related to the work of the heart. Among the reasons for its appearance are the following diseases:
- Diseases of an infectious nature;
- Kidney pathologies;
- Acute changes in the blood circulation of the brain.
It is also necessary to note conditions that, without being the cause of the pathology, provoke its appearance:
- Excessive physical activity that does not correspond to the person’s level of training;
- Psychological crisis, severe stress or emotional tension;
- Hypervolemia resulting from excessive amounts of fluid administered intravenously, which appears during a fever or pregnancy;
- Improper diet, which boils down to eating fatty and heavy foods before bedtime;
- Drink plenty of fluids before bed.
Application of venous tourniquets for pulmonary edema: indications
There is an algorithm for the action of medical personnel when diagnosing acute pulmonary edema. Most people would also like to master the simplest techniques of resuscitation in emergency situations.
In addition to providing access to oxygen during respiratory failure caused by pulmonary edema and relieving pain, a significant role in emergency treatment is played by reducing venous blood flow in the heart area. It is required to minimize the volume of circulating blood in the pulmonary circulation, which, in the absence of the necessary medications, can be facilitated by the application of venous tourniquets for pulmonary edema.
The main indication for emergency such manipulation is the development of pulmonary edema. The main trigger for this formidable problem is most often acute left ventricular failure.
To carry out such a manipulation, complex medical equipment is not required. The main thing is that the resuscitator has at hand 3 conventional venous tourniquets used for intravenous injections.
The only contraindication to the application of venous tourniquets is thrombophlebitis of the deep veins of the lower extremities in the acute stage. However, if the question is about life and death, thinking about the possible complications of manipulation does not always seem reasonable.
Applying venous tourniquets for pulmonary edema: how to do it correctly
Before starting the life-saving manipulation, the patient should be seated with his legs down. The patient should remain in this position for 5-10 minutes, which reduces blood flow to the heart and creates excess blood in the lower extremities. In the subsequent procedure, the main factor is the correct technique for applying tourniquets for pulmonary edema.
The action algorithm is as follows:
- Tourniquets are usually applied to the lower extremities simultaneously. The distance from the inguinal fold should be 15-20 cm. Place a towel, napkin or the patient’s clothing under the rubber.
- At the same time, tighten the right arm in the upper third of the shoulder with a rubber band. A fabric spacer between the skin and the tourniquet is mandatory.
- The tension force of the tourniquet should be such that, while preventing blood circulation through the venous bed, the arteries remain free. To do this, you need to constantly monitor the pulsation in the arteries.
- Every twenty minutes, change the position of the tourniquets on the arm and lower extremities clockwise.
The condition of the limbs is constantly monitored. The color of the skin below the site where the tourniquet is applied serves as a guide. Paleness and cyanosis of the skin indicate trophic disorders in the tissues and indicate excessive tension in the rubber product.
Such a procedure can take from 30 minutes to 1.5 hours, it all depends on the severity of the patient’s condition and the success of the manipulation. Venous tourniquets for pulmonary edema are removed gradually. The goal is simple: to avoid as much as possible the release of a large amount of liquid blood into the vascular bed, which can neutralize the entire positive effect of the manipulation and provoke repeated pulmonary edema
Long-term or frequent use of this method of combating pulmonary edema can lead to deep vein thrombosis of the extremities.
For any acute pathologies of the heart, the ability to quickly and skillfully provide first aid before the arrival of a medical team is very important. Mortality from pulmonary edema in the first 10 - 20 minutes of development of the acute process is up to 20%; successful emergency care at home can significantly reduce this figure.
Emergency care for cardiac asthma should be provided to the patient even before the ambulance arrives. How to do it correctly? What will the doctors do?
Characteristic symptoms
Since the attack is a consequence of excessive load on the pulmonary circulation, it manifests itself in the form of a rapid increase in blood pressure. Its consistently high levels influence a significant improvement in the permeability of the vascular walls, so the plasma begins to actively enter the lung tissue. As a result, due to the deterioration of natural gas exchange between the alveoli and the bloodstream, ventilation of the lungs deteriorates. This circumstance provokes the development of their edema.
Symptoms of a cardiac asthma attack begin to signal “problems” in the body 2-3 days before its onset. Here are the signs that you need to pay special attention to:
- Dyspnea;
- Feeling of tightness in the chest;
- The appearance of a dry cough after the slightest physical exertion or trying to lie down.
Note!
The attacks always begin unexpectedly, most often at night when the person is sleeping. This is explained by the fact that in the supine position, adrenergic regulation is weakened, which increases the load on the pulmonary circulation. An attack can occur during the day. In this case, its provocateur will be physical activity or a psycho-emotional unstable state.
A sudden onset attack manifests itself as follows:
- A person wakes up from the fact that he does not have enough air, it is difficult to breathe;
- Shortness of breath increases rapidly;
- A dry, strong cough appears, which after a short time will be accompanied by the discharge of colorless sputum;
- The patient tries to get up or sit down as quickly as possible, because in a lying position he suffocates;
- Respiratory activity occurs through the mouth;
- The victim has difficulty speaking;
- He is excited, anxious, and feels a strong fear of death.
Pronounced external symptoms include the following:
- The skin on the face (nasolabial triangle) and phalanges turns blue;
- Palpitations;
- The value of diastolic blood pressure is greatly exceeded, which, without stopping the attack, drops sharply after a short time.
Note!
Cardiac asthmatic manifestations can pass without changes in blood pressure.
The duration of pathological disorders can vary from 15 minutes to 2-3 hours, depending on the disease that caused them.
If the attack goes on without relief for a long time, the symptoms are more pronounced:
- The skin becomes gray;
- Veins swell in the patient’s neck;
- Cold sweat appears on the body and face;
- A thread-like pulse is accompanied by a sharp decrease in blood pressure;
- The person feels unable to make any movement.
Note!
The duration of the transition from the state of cardiac asthma to pulmonary edema depends on the severity of the pathology that provoked the attack. Its development can be lightning fast or gradual.
The following symptoms indicate that the lung tissue has begun to swell:
- The cough becomes wet;
- During it, copious frothy sputum filled with blood begins to come off;
- Clearly audible wheezing appears over the entire pulmonary surface;
- Pupils dilate;
- The patient can only be in a sitting position with his legs down (orthopnea position);
- Severe dizziness;
- Nausea, which may be accompanied by vomiting;
- Loss of consciousness;
- Possible manifestation of convulsive syndrome.
Technique for applying venous tourniquets for pulmonary edema: algorithm
The purpose of this manipulation is to reduce venous blood flow to the heart and the volume of circulating blood. The places where the venous tourniquet is applied are the limbs. But prolonged ligation of the limbs can lead to thrombosis, so the patient must be urgently sent to the hospital to avoid venous stagnation.
Placing tourniquets or tourniquets on the legs results in retention of up to 800 ml of blood in each limb. The technology is like this:
- The patient needs to be seated. Legs should hang down.
- The patient should sit in this position for at least 10 minutes. At this time, his blood pressure is measured.
- Stockings and elastic bandages can be used as a clamp.
- A tourniquet is placed on the thighs and arm at the top of the shoulder.
- Signs of proper application of a venous tourniquet: the legs become bluish-purple as blood stagnates. Changes in the limbs when applying a tourniquet should definitely occur if the procedure is carried out correctly.
- Check the pulse below the tourniquet. It shouldn't exist.
- If the patient has an attack, then with an upper pressure of 100 mm, he can be given nitroglycerin. When the patient is in the hospital, while tourniquets are applied, he is given decongestants such as furosemide.
- To relieve pulmonary edema, oxygen and alcohol vapor are injected using artificial respiration. This eliminates shortness of breath and hypoxia, while preventing the foaming of sputum. Narcotic analgesics may be used. Antihistamines are also prescribed.
A weak alternative is to bathe the patient's feet in a hot bath.
Hot water will dilate the blood vessels, but the return of blood will not decrease as much as when applying tourniquets. This procedure should take an hour on average. The maximum time for applying a venous tourniquet to a limb is 1.5 hours. The turnstiles are removed gradually. This will help avoid the injection of a large amount of liquid blood, which can negate the full benefit of the procedure. Frequent use of this method can lead to thrombosis.
Treatment of pulmonary edema (reduced venous flow to the heart)
Reducing venous flow to the heart can also be achieved by some “mechanical” methods.
One of the simplest and most accessible is the application of tourniquets to the limbs (primarily the lower ones). The tourniquet must be applied with such force that the veins of the limb are compressed, but the arteries are not (the pulse is preserved in the arteries distal to the tourniquet). Otherwise, the blood will not be deposited. With properly applied tourniquets, 600-800 ml of blood or more can be retained in each leg.
After relief of alveolar pulmonary edema, tourniquets should be released gradually to avoid the rapid entry into the general circulation of a significant amount of blood at once. We should not forget about the possibility of developing phlebothrombosis when tourniquets are applied for a long time. In recent years, certain types of artificial and assisted pulmonary ventilation - high-pressure ventilation - have become increasingly widespread for the treatment of pulmonary edema of various etiologies.
One of the mechanisms of action is a decrease in blood supply to the vessels of the pulmonary circulation. So far, the experience of using these methods in patients with acute MI is insufficient. The pathogenesis of pulmonary edema in acute MI cannot be reduced only to pulmonary congestion due to left ventricular failure. The nervous and endocrine systems are directly involved in its development [Popov V. G. Topolyansky V. D. 1975; Sarnoff, 1952].
It is believed that the rapid and significant therapeutic effect of narcotic analgesics is due not only to a decrease in venous flow to the heart, but also to the effect on the 1DNS, including the cerebral cortex and respiratory center. Morphine (1 ml of 1% solution) is administered intravenously slowly. In less emergency cases, it can be used IM or SC. Only rarely are morphine and similar drugs combined with atropine in the treatment of pulmonary edema (as opposed to the treatment of an anginal attack), since this condition is usually accompanied by tachycardia.
The effect of narcotic analgesics on the respiratory center, which is in an overexcited state during pulmonary edema, is beneficial, but even a slight overdose, especially in elderly patients, is fraught with severe breathing problems and even respiratory arrest. Promedol has a similar but weaker effect to morphine.
Neuroleptanalgesia (thalamonal 2 - 3 ml IV slowly per 10 ml of isotonic sodium chloride or glucose solution or an equivalent amount of fentanyl and droperidol) has a good effect in the treatment of pulmonary edema and cardiac asthma. The effect of narcotic analgesics can be enhanced by neuroleptic and antihistamines (1 - 2 ml of a 2.5% solution of pipolfen, 1 - 2 ml of a 1% solution of diphenhydramine).
Some authors use chlorpromazine in the treatment of pulmonary edema. We avoid this because it can aggravate the tachycardia and cause difficult-to-correct hypotension. In some cases, novocaine blockade of the stellate ganglion and especially spinal anesthesia are highly effective in the treatment of pulmonary edema, but in practice they are rarely used due to technical difficulties.
“Myocardial infarction”, M.Ya.Ruda
Read further:
Treatment of pulmonary edema (decreased circulating blood volume)
The application of venous tourniquets for cardiac asthma should be performed as follows:
- Prepare the limbs. Cardiac asthma is an indication for applying venous tourniquets to three limbs. On the legs they extend 15 cm below the inguinal fold, and on the arm 10 cm below the shoulder joint.
- Every 20 minutes, one tourniquet is removed and applied to the free limb.
- The tourniquet pressure should be greater than arterial pressure, but less than systolic pressure.
Providing first aid for cardiac asthma is extremely important; it can save the patient's life. But you need to know how to behave in case of heart failure. You can read in detail about emergency care for heart failure here.
The importance of pre-medical actions
The essence of first aid for cardiac asthma is to immediately call an emergency medical facility with a preliminary description of the symptoms, as well as to maintain the vital functions of the victim’s body.
Immediately after calling the doctors, it is necessary to measure the patient’s blood pressure, since your further actions will depend on its readings. Next you need to act in the following sequence:
- Ensure free flow of air into the room where the patient is located.
- Remove or unfasten all the pressing elements of his clothing.
- It is recommended that the patient be placed in a sitting position: this is the only way he can breathe.
- If blood pressure readings do not drop below 100 mm Hg. Art., nitroglycerin is indicated. The victim is given a tablet under the tongue or a dose of the medicine is injected if it is in the form of an aerosol. Remember that nitroglycerin can be used no more than 2 times. At the same time, monitor your blood pressure every 5 minutes, as you need to reduce blood pressure slowly.
- If nitroglycerin is not available, you can take validol.
- Usually 10-15 minutes after taking medications is enough for the patient to feel better. Then they begin actions that reduce the volume of circulating blood in the small systemic circulation.
- Application of a tourniquet on 2 legs and one arm. If there is no special rubber band, you can use an elastic bandage or nylon stocking. A tourniquet is made on the arm, 10 cm from the shoulder; on the legs, 15 cm from the groin area. Remember that you cannot tighten the device on a naked body. You definitely need to put some kind of fabric under it. The duration of the tourniquet on the limbs should not exceed 20 minutes. If medical help does not arrive by this time, the devices are removed, the limbs are allowed to rest for 5 minutes, and then they are applied again. In addition, you need to carefully ensure that during its application, stenosis does not form (a condition in which the vessels are compressed). When the tourniquet is applied correctly, a pulsation will be clearly audible just below the place where it is located, and the skin will acquire a purplish-blue color.
- If you are afraid to work with a tourniquet yourself, you can make a warm mustard foot bath. These remedies eliminate the enormous load on the heart and reduce the volume of circulating blood. However, foot baths are considered to be less effective than tourniquets.
Remember that after eliminating an attack of cardiac asthma, you need to find out the reason that caused it. Without proper treatment, it may recur. Therefore, you cannot refuse to go to a medical facility, even if all symptoms have passed by the time the doctors arrive.
Symptoms of cardiac asthma
In order to provide assistance correctly, you need to know the signs of the disease. These include:
- Severe cough that begins spontaneously. Sometimes pink sputum is released.
- The pupils are dilated.
- Facial cyanosis.
- Wheezing in the lower parts of the lungs.
- The pulse is rapid and arrhythmic.
- Pulmonary edema often quickly follows.
- Most often occurs at night.
Knowing the rules for applying unloading venous tourniquets, you can help the patient even before the ambulance arrives. Knowing how to properly provide assistance in any situation saves lives. Therefore, first aid courses have become popular, where knowledge is gained not only theoretical, but also practical. For example, here you can learn about how and what to do in case of venous bleeding.
Symptoms of pulmonary edema
Pulmonary edema is life-threatening. Timely action can save the patient's life. Main symptoms:
- Suffocation. It becomes difficult for the patient to inhale and exhale.
- Shortness of breath occurs. The patient can only be in a sitting position.
- Dry cough.
- Tachycardia.
- Moist rales in the lungs.
- Pressing pain in the chest.
- Paleness of the skin.
- Confusion of the patient, fear of death.
- Usually occurs at night.
Before the ambulance arrives, three venous tourniquets must be applied. This will give the patient time before the doctors arrive. He will then be treated in hospital.