Developed thrombosis of the internal jugular vein is caused by damage to the vascular wall and activation of the blood coagulation system. Cervical osteochondrosis and other somatic pathologies can contribute to this process. In this case, the patient develops severe headache and neurological disorders. Treatment of thromboembolism consists of the use of blood thinning drugs, and if this technique is ineffective, surgery is performed.
Blood blockage in the neck area causes mental and physical discomfort for the patient.
Features of the pathology
Jugular vein thrombosis requires timely diagnosis and treatment
Compared with lesions of the lower extremities, jugular vein thrombosis is considered less life-threatening. The most common trigger for the disease is infection. If a person has problems with blood clotting, the risk of developing thrombosis increases.
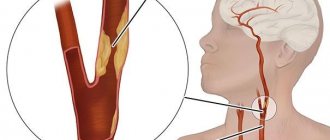
The jugular venous system includes vessels that drain blood from the head and neck. There are three pairs of veins, differing in anatomical location. The internal vein begins at the sigmoid sinus and goes to the subclavian artery.
The external vein runs along the front of the neck. It can be seen during singing, coughing and raising the tone of the voice. Its function is to collect and drain blood from the superficial part of the neck, face and head.
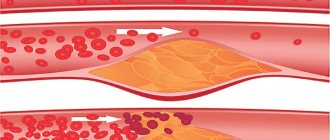
Thrombosis can affect any type of jugular vein, but most often it develops on the external one. Due to increased blood clotting and other pathological processes, fibrin is produced in the body.
As a result, a blood clot forms in the vascular cavity. It can form even in the absence of mechanical damage to the vascular walls.
Etiology and pathogenesis
Thrombosis of the jugular vein can be provoked by the following factors on the human body:
- burdened heredity;
- obesity;
- inactive lifestyle;
- consumption of foods rich in cholesterol;
- smoking;
- alcohol consumption;
- diabetes;
- atherosclerosis;
- atrial fibrillation;
- hypertension;
- entry into the body of an infectious agent;
- Varicose veins;
- increase in platelet count;
- vascular injury;
- neoplasms;
- hormonal imbalance;
- influence of medications.
Osteochondrosis of the cervical vertebrae can provoke thrombosis of the jugular vein
Pathology arises as a result of the presence of diseases, injuries, bad habits, and infections.
As a result of damage to blood vessels under the influence of various factors, most often somatic diseases or injury, the blood coagulation system is activated. This provokes the formation of a blood clot at the site of damage, which over time becomes large and can completely fill the entire vein. In this case, venous blood flow is disrupted and blood stagnates in the structures of the brain.
Possible reasons
A number of different pathological processes can provoke the occurrence of thrombosis. These include the following:
- Damage to endothelial cells. It is provoked by surgery, infectious diseases and various injuries.
- Changes in blood composition. Increased blood clotting can be congenital or acquired. The composition of the blood changes due to the progression of cancer, autoimmune disorders, etc.
- Stagnation of blood. A change in the direction of blood flow provokes diseases of the circulatory system and abnormalities in the functioning of the heart. Varicose veins can also be a provoking factor.
On a note! Drinking regime plays an important role in the effectiveness of therapeutic therapy. Pure water, supplied to the body in the required quantity, has a thinning effect on the blood.
How does pathology manifest itself?
There may be limited movement
To ensure the effectiveness of treatment, it is necessary to diagnose jugular vein thrombosis in a timely manner. Symptoms become more severe as the clot grows. The following signs help to suspect the presence of a blood clot:
- cyanosis of the skin surface in the area of the collarbones and neck;
- swelling of the affected vein;
- painful sensations that increase with palpation of the problem area;
- migraine;
- sharp pain when turning the head (in some cases radiates to the arm);
- redness of the skin in the area where the blood clot is located.
If there are clots in the jugular vein, signs of neurological diseases occur. In some cases, there is limited movement due to muscle hypotonia. Marked swelling may be present.
Causes of varicose veins on the face, under the tongue and under the eyes: treatment of veins of the neck and head, photo
Have all your attempts to cure varicose veins been unsuccessful?
Have you already thought about radical measures? This is understandable, because healthy legs are an indicator of health and a reason for pride. In addition, this is at least human longevity. And the fact that a person protected from vein diseases looks younger is an axiom that does not require proof.
The materials presented are general information and cannot replace medical advice.
The jugular vein is a significant paired vessel of the circulatory system, passing through the human neck.
Divided into internal, external and anterior. The main functions are to collect blood from the soft parts of the head and neck. Each of the jugular veins has a different location, structure and diameter. However, they all belong to the circulatory system of the superior vena cava. Let's take a closer look at the anatomy of each of these venous vessels.
The internal jugular vein originates at the opening of the skull, expanding in the shape of a bulb and descending to the sternoclavicular joint. It is covered in front by the mastoid muscle. In the area of the lower neck, it, together with the vagus nerve and the common carotid artery, is located in the common connective tissue sheath.
The external jugular vein is formed by two large venous trunks. The first of these is an anastomosis of the external jugular and mandibular veins, and the second is the posterior auricular vessel passing behind the concha.
The posterior auricle receives blood from the superficial plexus, which is located behind the auricle. This vessel also has a connection with the emissary and mastoid veins.
The occipital branch receives blood from the venous plexus of the head. Below the posterior auricular vein it enters the external jugular vein. In rare cases, the occipital vein accompanies the arterial canal and continues into the internal jugular vein.
The suprascapular venous vessel consists of two trunks, which unite and flow into the subclavian vein or into the last section of the external jugular vein.
The transverse canals of the neck accompany the artery of the same name and most often enter the main vein along with the suprascapular trunk and the occipital branch.
The vessel is paired and passes on both sides of the neck, entering the sternal space and connecting there into one blood channel through the jugular venous arch. After the anterior jugular vein passes behind the sternocleidomastoid muscle, it enters the external jugular vein and then the subclavian vein.
The vessel originates in the jugular cranial foramen, filling a significant part of its posterior space. Initially, the vein has a significant diameter - the superior bulbous extension. Then it narrows and moves downward, coming into contact with the posterior surface of the internal carotid artery, and then with the anterior wall of the external carotid artery.
Above the sternoclavicular joint, the vessel expands again. Here, at the level of the edge of the external jugular vein, there is the inferior bulb of the internal jugular vein. In the upper section, the vein has valves, merges with the subclavian, resulting in the formation of the brachiocephalic venous canal.
All about the cardiovascular system
Recent Entries
The information on the site is provided for informational purposes. Do not self-medicate under any circumstances. At the first symptoms of the disease, consult a doctor first.
Buy Generic Viagra in Ukraine at the best price!
Diagnostics
Ultrasound examination is performed
Veins located in the neck lend themselves well to diagnostic procedures. There are no difficulties in making a diagnosis. The main way to identify a pathological process is to conduct an ultrasound examination with Dopplerography.
It shows the speed of blood flow and the condition of the vascular walls at the current moment. Additionally, phlebography is performed using a contrast agent. Laboratory tests help get an overall picture of the state of the body.
The presence of an enzyme in the blood, which is a product of the breakdown of a blood clot, is also detected. Angiography is used to evaluate large vessels.
Important! With age, the risk of thrombosis increases. This is due to changes in lipid metabolism in the body, due to which the structure of the vascular wall is disrupted.
Prevention
To prevent the development of pathology, you first need to be attentive to your own health and undergo regular medical examinations. If a person is at risk, it is necessary to systematically conduct a study such as coagulometry - a blood test for clotting. Thus, it is possible to promptly detect hypercoagulation leading to the formation of blood clots in the vascular system.
Particular attention should be paid to the choice of clothing. It should not hinder movement or squeeze the body. For everyday wear, preference should be given to loose items made from natural fabrics and of appropriate size. We described how to avoid varicose veins on the legs in our article.
Giving up bad habits, adjusting your diet and diet, and daily moderate physical activity have a beneficial effect on the general condition of the body. Excluding fried and fatty foods from the menu reduces the chances of developing thrombosis, both of the superior jugular vein and similar pathologies everywhere.
Drug treatment
Thrombosis of the jugular vein in the neck can be eliminated with both drug therapy and surgery. The method of treatment depends on the severity of the disease.
The treatment course includes the mandatory use of thrombolytic drugs, which include Urokinase, Fibrinolysin and Streptokinase. If there is pain, taking analgesics is indicated.
Preparations from the phlebotonics group help normalize the outflow of venous blood. Antibacterial therapy is also prescribed. The most commonly used drugs are Diclofenac, Ketorolac and Nimesulide.
Medicines intended for local use include troxevasin and heparin ointments. The speed of recovery depends on the initial condition of the patient, the stage of the disease and its rapid development.
Jugular vein thrombosis: symptoms and treatment
The veins of the jugular system are much less likely to be affected by various diseases than those located in the lower extremities.
It's all about the location and characteristics of the blood supply through the jugular veins, but even these blood vessels can be completely or partially blocked by a blood clot. In fact, the reasons that can provoke the appearance of a blood clot in the jugular veins are quite diverse and can be rooted both in various unfavorable environmental factors and in the genetic characteristics of the human body. Common causes of jugular vein thrombosis include the following pathologies:
- anomalies in the structure of veins;
- lack of C,S-protins and antithrombin-3;
- violation of the anticoagulation properties of blood;
- various mutations;
- benign and malignant tumors;
- bad habits;
- injuries and previous neck surgeries;
- a large amount of excess weight;
- diseases of the cardiovascular system;
- kidney damage of any etiology.
Among other things, uncontrolled use of certain types of contraceptives can provoke the appearance of a blood clot in the jugular vein. Along with this, such a pathological condition can develop against the background of a high level of estrogen in the blood of a woman during menopause.
In rare cases, the development of jugular vein thrombosis may be a consequence of damage to the walls of the blood vessel during catheterization. It is extremely rare that the problem of a blood clot in the jugular vein can be rooted in an increased level of homocysteine in the blood. As a rule, such a predisposing factor is a consequence of a sedentary lifestyle.
In some cases, an increased risk of a blood clot in the jugular vein is a consequence of an increase in the blood of a special protein fibrinogen, which is produced by the liver.
Diagnosis and treatment
After the slightest signs of jugular vein thrombosis appear, you should seek advice from a therapist, phlebologist or cardiologist. An external examination is usually not enough to make a diagnosis.
Usually, if jugular vein thrombosis is suspected, an ultrasound with Doppler ultrasound is immediately performed, which allows for a high degree of visualization.
Other commonly used diagnostic methods include the following examinations:
- chest x-ray;
- angiography;
- scintigraphy;
- thromboelastigraphy;
- duplex scanning of veins;
- Magnetic resonance imaging;
- CT scan.
Therapy for jugular vein thrombosis depends on the characteristics of this pathological condition. In most cases, treatment of this pathological condition is carried out using conservative methods.
First of all, patients are advised to take anticoagulants, which help eliminate fibrinogen from the blood plasma, which is an important component that forms a blood clot. The most commonly prescribed anticoagulants include:
- Fibrinolysin.
- Heparin.
- Fraxiparine.
As a rule, these strong drugs are used exclusively during acute thrombosis. The duration of therapy with these drugs is selected individually for each patient.
In the future, weaker indirect anticoagulants can be used, for example, Cardiomagnyl or Aspirin Cardio.
To eliminate a blood clot and prevent its reappearance, the use of venotonic drugs is often required:
- Troxevasin.
- Glivenol.
- Detralex.
- Aescusan.
These drugs also help accelerate metabolism in the walls of the veins, and also have an analgesic effect and relieve inflammation.
In some cases, the use of antispasmodics may be required to eliminate spasm of the jugular vein affected by a thrombus.
To improve nutrition of the tissues of the cheeks, neck and shoulders, a necessary measure is the application of local agents with antiplatelet properties, including heparin or troxevasin ointment.
In particularly severe cases, surgical treatment of existing thrombosis may be performed. As a rule, minimally invasive techniques for removing blood clots are used, including the widespread use of transluminal aspiration thrombectomy and percutaneous endovascular thrombolysis.
If the patient promptly seeks qualified medical care and carries out adequate conservative therapy, the prognosis for life with a condition such as jugular vein thrombosis is usually favorable.
Surgical intervention
Endovascular thrombolysis and aspiration thrombectomy are in greatest demand.
Most often, minimally invasive surgical methods are used for thrombosis of the internal jugular vein. The following methods of performing the operation are in greatest demand:
- Endovascular thrombolysis. The procedure involves the introduction of a thrombolytic drug into the diseased vessel using a special catheter. This helps restore the patency of the vascular cavity.
- Aspiration thrombectomy. The operation involves removing the blood clot mechanically, through an incision in the skin.
Consequences and complications
Vessel thrombosis rarely provokes the development of thromboembolism, despite this, treatment should be carried out properly. Self-medication and ignoring the pathological process lead to serious health complications. These include:
- Sepsis. It is the process of infection spreading throughout the body.
- Pulmonary embolism. Often leads to death. It develops as a result of a blood clot breaking off and entering the pulmonary artery.
- Papilledema. Pathology leads to impaired vision function or its complete loss.
Forecast
Timely contact with doctors ensures a favorable development of events. The exception is cases when venous thrombus formation is caused by oncology. If the disease is neglected, it can lead to serious health problems. The recovery process after treatment in this case will be long – from 3 to 6 months.
Interesting! Sometimes bleeding disorders occur as a result of long-term use of medications. Medicines that affect the structure of the blood include oral contraceptives.