How to deal with deviations
Both prolonged deficiency and excess of insulin are pathological conditions that require correction.
Raising insulin levels
Hormone levels can be increased using replacement therapy. It consists of the therapeutic administration of insulin analogues. There are several groups of such drugs that are combined into certain regimens:
- short-acting drugs (Actrapid NM, Humalog, Novorapid);
- medium-duration medicine (Protafan NM);
- long-acting insulin (Lantus, Levemir).
A synthetic analogue of the hormone is used to restore insulin levels in the body
A low-carb diet is another way to increase your blood insulin levels. This is a method of nutrition correction in which the patient’s body receives a small amount of carbohydrates. The principles of the diet are to avoid sugar, alcoholic beverages, and eat small, frequent meals. The patient should eat at approximately the same time. This stimulates the pancreas to work “on schedule.”
You should avoid fried, smoked and salty foods. Preference is given to steamed, boiled, stewed and baked dishes.
Important! The work of the gland is stimulated by blueberries, greens, apples, kefir, cabbage, and lean meats. They definitely need to be included in the daily menu. . We reduce the indicators
We reduce the indicators
To reduce insulin levels, it is necessary to get rid of the cause of the pathological condition. If hyperinsulinism causes a tumor, it must be removed followed by chemotherapy. Extrapancreatic causes must also be eliminated.
Drug treatment is used only during periods of hypoglycemic attacks. At an early stage, the patient is given something sweet, and later glucose is injected into a vein. At the coma stage, injections of glucagon, adrenaline, and tranquilizers are used.
The rest of the time, insulin levels are kept within acceptable limits by diet. It is important that the body receives up to 150 g of carbohydrates per day, meals are frequent and fractional. It is better to avoid foods that are too sweet.
Any changes in the body should be discussed with a qualified specialist. This will help avoid the development of complications and speed up the recovery process.
How to take and pass the analysis
The insulin content is determined in plasma (blood is taken into a tube with heparin) or in serum (blood taken without an anticoagulant is centrifuged). Work with biological material begins immediately (maximum after a quarter of an hour), since this medium does not tolerate long “downtime” without treatment.
Before the study, the patient is explained the significance of the analysis and its features. The reaction of the pancreas to food, drinks, medications, and physical activity is such that the patient should fast for 12 hours before the study, not engage in heavy physical work, and avoid taking hormonal medications. If the latter is impossible, that is, the medications cannot be ignored, then an entry is made on the analysis form that the test is being carried out against the background of hormone therapy.
Half an hour before venipuncture (blood is taken from a vein), the person waiting in line for the test is asked to lie down on the couch and relax as much as possible. The patient should be warned that failure to comply with the rules may affect the results and then a return to the laboratory, and, therefore, repeated restrictions will be inevitable.
What influences the result
There are four important factors that can lead to a false result:
- Eating immediately before blood sampling - insulin synthesis automatically increases when food enters the body. Accordingly, the blood after a hearty breakfast will be oversaturated with sugars and insulin, which strives to normalize carbohydrate metabolism.
- Eating fatty, sweet, spicy foods the day before, as well as strong alcoholic drinks - holiday feasts provoke overeating, which in turn entails an increased load on the liver and pancreas, forcing these organs to work incorrectly.
- Stress and intense physical activity - insulin release increases when the body experiences stress, so you should rest well and get enough sleep the night before.
- Errors on the part of the laboratory when blood is examined not immediately, but after a certain time. It has been found that the results obtained are more accurate if fresh blood is used for the study. 15 minutes after collection, its chemical parameters, even under the influence of anticoagulants, sharply decrease and it ceases to be “alive.”
These factors should be taken into account, since their neutralization will allow obtaining more reliable results.
The effect of insulin on the body
The influence of the hormone extends to all cells, but insulin primarily acts on the liver, muscles and adipose tissue. The main functions of this protein in relation to glucose:
- seizure from blood;
- movement across the cell membrane;
- absorption by tissues to produce energy.
In addition, with its help, glycogen is formed from glucose molecules and its breakdown is stopped, the rate of synthesis of new glucose from proteins and fats decreases.
Additional processes in which insulin takes part include:
- inhibition of the breakdown of fat to acids;
- preventing the growth of ketone bodies in the blood (they appear in excess when fats rather than glucose become the source of energy);
- removal of fats from the body;
- ensuring the movement of amino acids across the cell membrane;
- activation of protein formation and slowdown of its breakdown.
Negative effects of increased insulin
If insulin is elevated, disorders affect all body systems:
- Glucose regulation becomes spasmodic: at first its level is too high, but after the release of insulin it decreases excessively. A person feels mild hypoglycemia: nervousness, hunger, cravings for sweets. Carbohydrate intake automatically increases, the patient is one step closer to diabetes.
- High insulin promotes the synthesis of fats and prevents their breakdown. The person is gaining more and more weight.
- Simultaneously with the growth of fatty tissue, blood lipids also increase. Adipose tissue located in the abdominal cavity is especially dangerous: triglycerides from it penetrate into the blood more actively.
- Cholesterol synthesis increases in the liver, and the risk of atherosclerosis increases.
- Excess insulin affects blood clotting factors, which, in combination with atherosclerosis, provokes thrombosis.
- Long-term elevated insulin increases the tone of the nervous system, constricts blood vessels, which causes an increase in blood pressure.
Additionally: Tables with norms and deviations of cholesterol in the blood
Insulin deficiency
Insufficient insulin production leads to an increase in plasma glucose levels. This circumstance leads to the development of such a pathological condition as diabetes. Insulin deficiency can be caused by various reasons, and its deficiency can be determined by some specific symptoms.
Symptoms of insulin deficiency
The following symptoms may indicate insufficient levels of the hormone:
- constant feeling of thirst;
- dry mouth;
- increased frequency of urination;
- hunger;
- A blood test shows elevated glucose levels (hyperglycemia).
If the above symptoms are present, a person should immediately contact an endocrinologist. Diabetes mellitus is a complex pathological condition that requires immediate treatment.
If the disease is detected in a timely manner, therapy can be limited to tablet drugs, and the sugar level can be maintained with proper nutrition.
The main symptom of diabetes is a constant feeling of thirst.
Attention. Without proper treatment, insulin deficiency begins to progress and acquire increasingly serious forms that threaten the patient’s life.
Causes of hormone deficiency
Insulin deficiency can occur for a number of reasons. This:
- Eating “junk” food, frequent overeating.
- The diet consists of a large amount of sugar and white flour. To convert this amount of sugar, the pancreas is required to produce large volumes of insulin. Sometimes the organ is not able to cope with such a task, and dysfunction of the gland occurs.
- The presence of chronic and severe infectious diseases. They weaken immune function and increase the risk of associated pathologies.
- Severe stress, nervous shock. The level of glucose is directly proportional to the psychological state of a person; with nervous excitement, the level of sugar in the blood rises to critical levels.
- High physical activity or complete passivity.
- Inflammatory processes in the pancreas.
- Complications after surgery.
- Hereditary predisposition.
- Lack of protein and zinc, as well as elevated iron levels.
What to do if your blood insulin is low?
Insulin is involved in the metabolism of glucose, fats and amino acids. Insulin also has an anabolic effect on the body and prevents lipolysis.
Insulin is released into the blood by beta cells of the pancreas. Insulin synthesis begins when glucose levels are above 100 mg/decilitre. This happens every time after eating.
That is, the main function of insulin is to get rid of excess glucose in the blood.
If insulin exceeds normal levels, heart disease, clogged arteries, obesity and loss of muscle fibers can develop. If the level of insulin in the blood is very high, death can occur.
Lack of insulin leads to the development of diabetes, kidney failure, and various nervous system disorders.
Properties of insulin
Insulin has the following effects on the body:
- stimulates protein synthesis (insulin activates protein production by ribosomes; if there is little insulin in the blood, ribosomes do not work);
- prevents the destruction of proteins;
- stimulates the formation of glycogen (promoting the formation of glucose reserves);
- participates in the delivery of certain amino acids to cells;
- prevents the breakdown of fat (instead of fat, insulin promotes the breakdown of carbohydrates) and blocks hormone receptor lipase, which is responsible for the breakdown of adipose tissue;
- increases fatty acid production in the liver and stimulates cholesterol production.
Symptoms of insulin deficiency
Low insulin levels may present with the following symptoms:
- hypergycemia;
- polyuria;
- polydipsia.
Hyperglycemia (high blood sugar) occurs because glucose accumulates in the blood and, due to the absence or low levels of insulin in the blood, is not transported into cells. Lack of insulin over a long period of time can mean the development of type 1 diabetes (in this case, treatment is with daily insulin injections).
At night, glucose levels in the body rise. If there is not enough insulin in the body, then glucose is excreted in the urine, which provokes polyuria (increased urine volume). At the same time, the body's need for fluid increases. Constant strong thirst appears (polydipsia).
Also signs of low insulin levels in the blood are poor wound healing, itchy skin, increased fatigue and lethargy. Symptoms of insulin deficiency increase rapidly. Therefore, when the first mild symptoms appear, you need to consult a doctor and start treatment.
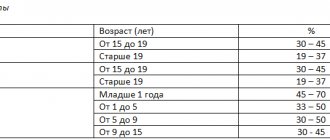
For an adult, insulin is normally 3-25 µU/ml, and in children 3-20 µU/ml. If a child has low insulin, this may indicate the development of type 1 diabetes. The pancreas is finally formed by the 5th year of child development.
From 5 to 11 years of age, children are especially vulnerable to diabetes. At this age, children need a daily intake of 10 g of carbohydrates per kg of weight, which increases the need for insulin.
In addition, the human nervous system in childhood is not yet fully formed, which can also cause disruptions in insulin synthesis.
Damage to the pancreatic cells that synthesize insulin can cause childhood infectious diseases such as measles, mumps and rubella. In this case, timely vaccination can protect a child from developing type 1 diabetes.
Low insulin in very young children can be suspected if the child suckles very greedily or drinks water. Since excess glucose is excreted in urine, diapers become stiff from such urine.
Causes of insulin deficiency
The most common reasons for low insulin levels in the blood include:
- poor nutrition (frequent overeating, consumption of large amounts of refined carbohydrates);
- stressful situations;
- overwork and intense physical exertion;
- chronic diseases and infectious diseases.
Treatment
To restore the functioning of pancreatic cells that produce insulin, the drug Civilin is used.
Livicin (a drug that promotes vasodilation) and medzivin (a drug that restores hormonal levels) are also used in treatment.
If the pancreas is no longer able to produce insulin at all, the patient is prescribed insulin injections, which he can do with outside help or on his own.
How to increase insulin in the blood without drugs: if the pathological processes that led to a decrease in insulin production have not gone far, you can help stimulate the pancreas by eating cabbage, apples, blueberries, kefir and lean meat. You should avoid eating potatoes, rice, semolina, and honey.
Low insulin in the blood should be a reason to reconsider the principles of nutrition (it should be complete and balanced). You need to eat small meals often.
Source: https://saharnyydiabet.ru/chto-delat-pri-nizkom-insuline-v-krovi/
How to determine indicators
The level of insulin in a woman’s blood on an empty stomach, namely 3.0 to 25.0 µU/ml, is the most indicative when it is necessary to determine the hormone ratio. This is explained by the fact that after eating food, the concentration of the component increases, being a response to the penetration of carbohydrates into the body.
Please note that:
- It is strongly recommended not to use any medications 24 hours before donating blood. At the same time, the patient should discuss this possibility with a specialist in advance;
- the most accurate information will be obtained by combining two types of hormone analysis: in the morning the blood is examined on an empty stomach, after which the woman is given a glucose solution to drink, and the material is removed again two hours later;
- Based on this, one can draw any conclusions about an increase or decrease in the ratio of the hormone present in the bloodstream.
Only using similar techniques can we talk about a complete picture of the activity of the pancreas not only in women, but also in males, as well as in children.
Each type of examination will require the use of venous blood.
It is important to understand that the level of insulin in a woman’s blood, namely 3.0 to 25.0 µU/ml, is direct evidence of how normal her health is and what kind of treatment is necessary in this particular case.
udiabeta.ru
Insulin
- a hormone produced by the pancreas. Its main function is to transport glucose, fats, amino acids and potassium to cells. In addition, the substance controls blood sugar levels and is responsible for regulating carbohydrate balance. All this happens when women have normal amounts of insulin in their blood. But for various reasons, the amount of the hormone may change. And this definitely affects your well-being and health.
What is the norm of insulin in the blood of women on an empty stomach?
To obtain reliable data, it is necessary to measure insulin levels on an empty stomach. If you conduct the analysis after eating, the data will be distorted. This happens because after eating, the pancreas begins to function and very actively produce the hormone. As a result, the content of the substance in the blood will be overestimated.
The normal level of the hormone insulin in women is from 3 to 20 µU/ml. A slight increase in indicators during pregnancy is allowed - as a rule, they vary from 6 to 27 µU/ml. The amount of the substance also changes upward in older people. After 60 years, it is considered normal if 6 to 35 µU/ml of the hormone is detected in the blood.
Insulin in the blood of women in normal quantities ensures the performance of vital processes:
- Due to the substance, muscles are built. It promotes the activation of ribosomes that synthesize protein, which, in turn, takes part in the construction of muscle tissue.
- Thanks to insulin, muscle cells can function correctly.
- The substance prevents the breakdown of muscle fibers.
- In normal amounts, insulin in women's bodies increases the activity of enzymes responsible for the production of glycogen. The latter, in turn, is the main form of glucose storage.
womanadvice.ru
Pathological changes in the norm
Insulin contained in the blood of women often deviates from the norm, which is a reason to sound the alarm. This may be due to the following reasons:
- Excessive physical activity.
- Frequent stress.
- Overweight.
- Taking hormonal drugs.
- Liver pathology.
All these problems are considered to be a consequence of an incorrect lifestyle, which, by correcting it, can normalize insulin levels. But this is not always enough; in such cases, the presence of deviations may be a sign of dangerous diseases.
The accuracy of the analysis is justified.
Hormone production always increases during meals, so blood sampling is performed only on an empty stomach.
This helps avoid false elevated readings. More accurate is to carry out the analysis in 2 stages. In this case, the first time the biomaterial is taken from the patient on an empty stomach, then she drinks a glucose solution and repeats the analysis after 2 hours.
How to raise and lower insulin
Knowing what the normal insulin level should be, many patients wonder: how to increase or decrease insulin in the blood? This can be done most effectively by using special medications that help fight diabetes.
So, drugs to lower sugar also help reduce the secretion of the hormone insulin and lower its concentration in the body in type 2 diabetes. Insulin-lowering medications should be taken daily to reduce the load on the pancreas and prevent it from becoming depleted.
But it is important to choose medications that increase tissue sensitivity to insulin and thereby reduce glucose concentrations. Under no circumstances should you use drugs that result in increased insulin production.
Treatment
If, in parallel with low insulin levels, a patient has high blood sugar, he may need constant injections of this hormone using an insulin syringe or a special pen. With type 1 diabetes, it is unfortunately impossible to force the body to produce this hormone on its own in the required quantity. Insulin replacement therapy in injections is the only way out in this case. But along with this, it is necessary to follow a low-carbohydrate diet (especially at first) and eat small portions at strictly defined hours.
A low-carbohydrate diet is prescribed to patients in order to relieve the pancreas and give it the opportunity to at least slightly increase its functional activity.
The rules of such nutrition imply a temporary refusal of the following foods:
- sweets and sugar;
- fruits;
- cereals (even unpolished);
- bread;
- berries;
- pasta.
What can people on a low-carb diet eat? The basis of the diet should be white and green vegetables (except potatoes and Jerusalem artichoke), meat, lean fish, cheese, eggs and seafood. A small amount of butter is allowed. At first glance, it may seem that such restrictions are too strict, but you need to understand that this is a temporary and necessary measure necessary to improve the general condition.
You can lower blood sugar with insulin injections. But without following a diet, treatment will not be effective, and the patient may develop complications of the disease.
In addition to diet and insulin injections, the patient may be prescribed drugs to improve blood microcirculation, and, if necessary, drugs to get rid of edema and maintain the heart. All additional medications are selected individually, taking into account the patient’s age and the presence of concomitant diseases. Sometimes the doctor may recommend that the patient take dietary supplements such as Civilin, Medcivin and Livicin. These are preparations based on medicinal plant extracts that improve blood circulation, calm the nervous system and help the body improve immunity. But not all patients need them, so under no circumstances should they be taken without an endocrinologist’s prescription.
A little about insulin therapy
The selection of insulin therapy for each patient is carried out individually. The patient, together with the doctor, should achieve maximum compensation for carbohydrate metabolism.
Discuss this with your doctor
In general, insulin therapy should mimic physiological insulin secretion:
- Basal, which provides normoglycemia during the interdigestive period and during night rest. Its average rate is 0.5-1 units/hour, or 12-24 units per day;
- Stimulated (food), corresponding to the level of proprandial glycemia. When calculating the required dosage, it is necessary to take into account that 1-1.5 units of insulin are produced per 1 XE (bread unit).
The main principles of insulin therapy include:
- administration of the hormone in maximum accordance with physiological secretion;
- correct distribution of insulin throughout the day (2/3 in the evening, 1/3 in the late evening and at night);
- a combination of long-acting and ultra-short-acting insulin injections.
The advantages of intensified therapy are:
- imitation of physiological processes in the body;
- higher quality of life for the patient and minimization of complications;
- ease of understanding of the general principles of treatment by the patient and his relatives.
But there are also disadvantages:
- the need for frequent self-monitoring of glycemia up to 5-6 times a day;
- the need to educate the patient and his relatives;
- possible tendency to hypoglycemia.
Diabetes school operates at clinics
Normalization of insulin levels
Regardless of whether the level of insulin in the blood is increased or decreased, it must be normalized to prevent the development of pathologies in the body.
A decrease in the hormone is corrected by administering its injections. Third-party insulin comes in several types, which differ from each other in the speed of action and duration of action.
The type, dosage, injection site and hours of taking hormone injections are prescribed only by the attending physician. In addition, the doctor indicates the necessary diet that is recommended to be followed.
To reduce the amount of insulin in the blood, diet and physical therapy are mainly used. The diet is based on eliminating foods containing large amounts of sugar from the diet. The basis consists of dishes from vegetables, lean meat, seafood and dairy products
In addition to diet, it is important to constantly load the body with moderate exercise, which helps convert sugar in the body into energy, and, consequently, reduce insulin levels.
If diet and exercise do not help, then medications are prescribed that restore the response of the pancreas to the amount of sugar in the body, which leads to normalization of insulin levels.
Fasting insulin blood test
You can have your insulin levels checked at the clinic. For this purpose, two methods are used: on an empty stomach and after a carbohydrate load. To establish an adequate diagnosis, both tests are required.
Fasting insulin testing is performed only on an empty stomach. There should be at least 8 hours between blood collection and the last meal, ideally 12–14 hours. Therefore, the best time for diagnosis is the morning after a night's rest. This will allow the patient to easily endure the forced refusal to eat. 24 hours before the test, you need to exclude sweet and fatty foods from your diet. You should also refrain from drinking alcoholic beverages and smoking.
To correctly determine the level of insulin in the blood, you should avoid strong emotional disorders and heavy physical activity. On the morning of the study, any drinks are prohibited (except for pure water without carbon), and food must not be eaten.
Blood for analysis is taken from a finger. In exceptional cases, a venous blood sample is used for the test. Often, the endocrinologist additionally prescribes diagnostics of the pancreas. This helps to identify lesions and inflammatory processes in the organ that cause the death of β-cells.
Insulinedit edit code
Historical reference
The discovery of insulin is one of the most exciting in medicine. The honor of the discovery belongs to Banting and Best, but without the previous work of many researchers it would have been unthinkable. In 1869
German medical student Paul Langerhans noticed that the pancreas consists of two groups of cells - acinous cells that secrete digestive enzymes, and others collected in the so-called islets. Langerhans suggested that islet cells perform some special function
What this function was was only discovered in 1889, when Oskar Minkowski and Joseph von Mehring described a syndrome similar to diabetes mellitus in pancreatectomized dogs (Minkowski, 1989).
This was followed by many attempts to isolate a substance from the pancreas that regulates blood glucose levels. In the early 1900s. German physician Georg Ludwig Zülzer decided to inject an extract from the pancreas into a patient dying of diabetes. The patient felt better, but not for long: when the supply of the extract ran out, he fell into a coma and died. Another attempt to find an antidiabetic factor was made in 1911 by E. L. Scott, a student at the University of Chicago. He treated dogs with experimental diabetes mellitus using an alcoholic extract of the pancreas (by the way, almost the same as that later used by Banting and Best). However, Scott's supervisor found these experiments inconclusive because he did not measure blood glucose levels. From 1916 to 1920, the Romanian physiologist Nicolae Paulescu conducted a series of experiments in which he showed that administering an extract from the pancreas to dogs with experimental diabetes mellitus reduced the content of glucose and ketone bodies in the urine. Despite the fact that these results were published, Paulescu's work was only appreciated many years later.
Unaware of the work of his predecessors, a young Canadian surgeon from Toronto, Frederick G. Banting, in 1921, begged professor of physiology John J. R. McLeod to let him into the laboratory to isolate antidiabetic factor from the pancreas. Banting hypothesized that the hormone (insulin) secreted by islet cells was rapidly destroyed by proteases during or before extraction. Together with Charles G. Best, a fourth-year medical student, he began ligating the pancreatic ducts to avoid proteolysis. After ligation, the acinar cells underwent degeneration, but the islets remained intact, and the antidiabetic factor was extracted from them using ethanol and acid. The resulting extract reduced blood glucose levels in dogs with experimental diabetes mellitus.
The first patient to receive Banting and Best's extract was fourteen-year-old Leonard Thompson (Banting et al., 1922), admitted to Toronto City Hospital with a blood glucose level of 500 mg% (28 mmol/l) and a daily urine output of 3-5 l. Despite a strict diet (450 kcal/day), glucosuria increased, and without insulin the boy would have died in a few months. A trial administration of pancreatic extract resulted in a reduction in blood and urine glucose levels. Then the researchers began to inject the boy with Zxtracg daily, which was followed by immediate improvement. Daily glucose excretion decreased from 100 to 7.5 g. In addition, “the boy became cheerful, stronger and said that he felt much better.” Thus, replacement therapy with a new hormone, insulin, prevented inevitable death from diabetes (Banting et al., 1922). In the following year, Banting and Best were plagued by failure. They were unable to achieve reproducibility of results, that is, to obtain active extracts of the pancreas from time to time. McLeod got involved in solving this problem, and, in addition, Banting turned for help to James B. Collip, a chemist famous for the isolation and purification of adrenaline. Soon the extraction technique was fine-tuned, and patients in North America were able to be treated with insulin isolated from the pancreas of pigs and cattle. Currently, diabetes mellitus is treated with human insulin obtained using genetic engineering methods.
Symptoms and signs of low insulin levels
A symptom of diabetes is thirst.
Diabetes was first described by the ancient Roman physician Aretaeus, who drew attention to the pathological loss of fluid in a patient. He noted in his observations that the incoming fluid flows out of the body unchanged. This is where the name of the disease comes from: “diabetes” comes from the Greek “flowing through.” Increased urination is one of the first signs of insufficient functionality or synthesis of insulin. Excessive amounts of glucose in the blood are dangerous for the body, so it tries to get rid of it by excreting the excess in the urine. Increased fluid loss provokes the next symptom of insulin deficiency - constant thirst and dry mouth, the skin also becomes dry and flaky.
The lack of energy in tissues and organs due to glucose not reaching them causes the brain to give the command about hunger. Low insulin levels provoke increased appetite; often, despite the fact that the amount of food increases, the feeling of fullness does not occur for a long time. At the same time, body weight often decreases, which is due to general exhaustion of the body, loss of muscle mass, and fatty tissue.
Patients may complain of numbness in the extremities
Numbness of the limbs is another symptom, the cause of which is damage to the nervous tissue. High blood pressure is the result of the negative effects of high glucose levels on the nervous system.
The smell of acetone appears as a result of increased production of ketone bodies, it can be felt when breathing, coming from the body or urine excreted.
Wounds that take a long time to heal are a known symptom of low insulin levels. The cause is microcirculatory disorders, necrotic processes, inhibition of cell proliferation, etc.
Functions and norm
The hormone insulin regulates sugar levels by transporting it into the cells and tissues of the body:
- Carbohydrates enter the gastrointestinal tract with food and are broken down into glucose.
- Blood glucose levels rise, which is a signal for the release of insulin.
- The hormone binds the monosaccharide and transports it to muscle and fat tissue.
- In the muscular system, glucose is broken down into energy, which is needed for the proper functioning of the body, and in the lipid tissue, sugars accumulate (deposit formation).
The hormone is also involved in the “transfer” of fats, proteins and microelements into cells, activates the synthesis of amino acids, which results in increased muscle performance, participates in regeneration processes, and stimulates the work of enzymes necessary for the formation of glycogen.
The norm of insulin in women on an empty stomach (in mU/ml) is 3-29. In children under 12 years of age - up to 20. During pregnancy, a slightly increased insulin level is allowed - 6-32. The indicator numbers for older people are 6-35. A condition in which insulin in the blood is high is called hyperinsulinism. It can be primary or secondary, depending on the causes of the pathology.
Primary form
The second name is pancreatic hyperinsulinism, since all the causes of development are associated with disruption of the secretory apparatus of the pancreas:
- Insulinoma is a tumor that autonomously synthesizes the hormone. The result is high levels of insulin in the blood and hypoglycemia. The state of hyperinsulinism usually develops on an empty stomach. Symptoms: increased appetite, obesity, headache, seizures, neurological disorders.
- Reduced glucagon production - a process that leads to slower glycogenolysis and lower blood sugar levels. Accordingly, insulin is increased.
- Diabetes mellitus type 2 - the body's cells stop responding to the hormone, losing sensitivity to it. The body perceives this as if the hormone is not enough, and compensates for the condition with increased synthesis.
Secondary form
Increased insulin in the blood caused by extrapancreatic pathologies develops against the background of the following conditions:
- after removal of part of the stomach;
- prolonged fasting;
- neurotic disorders;
- diarrhea;
- increased body temperature;
- liver pathology;
- congenital metabolic abnormalities;
- tumors of the pituitary gland and adrenal glands.
Hyperinsulinism can develop against the background of increasing doses during therapy with insulin preparations and hypoglycemic agents. Increased insulin in the analysis can be observed as a result of pharmacological interference with certain medications.
About insulin
The pancreas is responsible for the production of insulin, a unique organ that simultaneously performs exocrine (exocrine) and intrasecretory (endocrine) functions.
The main purpose of the hormone is to regulate carbohydrate metabolism and timely delivery of glucose, as an energy source, to the cells and tissues of the body.
To ensure vital functions, insulin is involved in the following processes:
- glycogen production (insulin helps synthesize and maintain glucose reserves to replenish cells with energy in case of energy deficiency);
- inhibition of the breakdown of amino acids into simple sugars;
- regulation of the level of ketones (acetone bodies) in the blood (the hormone controls the amount of ketones, preventing them from accumulating);
- protein synthesis (activates their production and prevents decay);
- the formation of RNA (ribonucleic acid), which encodes and transmits hereditary information.
Without insulin, the body is unable to function fully. Glucose from food is concentrated in the blood, and cells do not receive adequate energy. Type 1 diabetes occurs, otherwise insulin-dependent. For normal human existence, he needs regular replenishment of the body with artificial medical insulin. In the case when insulin production is carried out in full, but due to a violation of carbon metabolism, cells cannot absorb it, insulin resistance develops - type 2 diabetes mellitus.
The effect of insulin on metabolism
The hormone insulin carries glucose into the cells, providing the body with energy, which is released during its breakdown inside the cells. In addition, it delivers amino acids (especially valine and leucine), potassium and magnesium ions, and phosphates to tissues.
Insulin has the properties of activating the main enzymes that are involved in the use of glucose in the processes of glycolysis and glycogen formation, slowing down the formation of glucose in liver cells. Thanks to these effects, the level of glucose in the blood that comes from food decreases.
For the body, insulin is the main anabolic hormone, as it enhances protein synthesis and inhibits its breakdown. The effect of insulin on fat metabolism is in the form of an increase in the synthesis of fatty acids, the conversion of glucose into triglycerides in the liver and a decrease in the flow of lipids into the blood.
The main role of the hormone is hypoglycemic
The action of insulin in the human body (and not only the human body, in this regard, all mammals are similar) lies in its participation in metabolic processes:
- This hormone allows sugar obtained from food to freely penetrate into the cells of muscle and fat tissue, increasing the permeability of their membranes:
- It is an inducer of glucogen production from glucose in liver and muscle cells:
- Insulin promotes the accumulation of proteins, increasing their synthesis and preventing the breakdown, and fatty products (it helps adipose tissue to capture glucose and convert it into fat (this is where excess fat reserves come from and why excessive love of carbohydrates leads to obesity);
- By increasing the activity of enzymes that enhance the breakdown of glucose (anabolic effect), this hormone interferes with the work of other enzymes seeking to break down fats and glycogen (anti-catabolic effect of insulin).
Insulin is everywhere, it is involved in all metabolic processes occurring in the human body, but the main purpose of this substance is to ensure carbohydrate metabolism, since it is the only hypoglycemic hormone, while its “opponents”, hyperglycemic hormones, seeking to increase the sugar content in blood, noticeably more (adrenaline, growth hormone, glucagon).
First of all, the mechanism for the formation of insulin by β-cells of the islets of Langerhans is triggered by an increased concentration of carbohydrates in the blood, but before this the hormone begins to be produced as soon as a person, having chewed a piece of something edible, swallows it and delivers it to the stomach (and it is not at all necessary that the food product was carbohydrate). Thus, food (any) causes an increase in the level of insulin in the blood, and hunger without food, on the contrary, reduces its content.
In addition, the process of insulin formation is stimulated by other hormones, increased concentrations of certain microelements in the blood, for example, potassium and calcium, and increased amounts of fatty acids. The growth hormone somatotropin (GH) inhibits insulin production to the greatest extent. Other hormones also reduce insulin production to some extent, for example, somatostatin, synthesized by the delta cells of the islet apparatus of the pancreas, but its effect still does not have the effect of somatotropin.
It is obvious that fluctuations in the level of insulin in the blood depend on changes in the glucose content in the body, so it is understandable why, when studying insulin using laboratory methods, they also carry out a determination.
What are the dangers of low insulin with normal sugar?
Insulin is a hormone produced in the pancreas. In the body, it controls the amount of glucose in the blood. It also affects metabolism in all tissues and cells. Low insulin with normal sugar leads to serious disturbances in the metabolic function of the human body. In turn, this can cause the development of diabetes, glucosuria and ketosis.
What are the dangers of reducing the amount of hormone?
Low insulin is one of the main causes of diabetes. With a lack of this hormone, insulin dependence can develop - the substance must be periodically introduced into the patient’s body to maintain its normal level in the blood.
The deficiency has a very serious effect on the functioning of the body. Tissue cells, not receiving the required amount of glucose, begin to look for other sources for energy production. In this case, glucose replaces fat.
Over time, its breakdown products accumulate in the body in ever larger quantities and lead to fainting and death from intoxication.
If the level of the hormone is reduced, a disturbance in the water-salt balance of the body occurs, which can lead to a significant decrease in blood pressure. Because of this, the blood supply to all organs, including the brain, is disrupted.
Type 1 diabetes, caused by a lack of insulin due to dysfunction of pancreatic cells, is one of the top 10 leading causes of death in the US population. Without receiving the necessary treatment, the patient can live a maximum of 20 years. If the hormone is injected or taken orally, you can live for about 50 years.
Symptoms of low insulin
When the level of this hormone in the blood is low, the following symptoms may appear:
- Increased blood sugar. If insulin is below normal or not produced at all, glucose stops being transported into cells, remaining in the bloodstream. Cells begin to look for another source of nutrition. This is called type 1 diabetes. Patients must receive regular injections of the hormone. Sometimes the problem is not the lack of insulin itself, but a disruption in its interaction with cell receptors, which prevents it from performing its functions. This leads to type 2 diabetes, the most common form of the disease.
- The amount of urine increases. A rise in glucose levels in the bloodstream causes it to draw water from the body, leading to polyuria - an increased amount of urine.
- Constant feeling of thirst. Due to the increase in water consumption by the body, the patient very often experiences thirst, which is a natural mechanism aimed at replenishing fluid.
Reasons for decreased hormone levels
These include the following:
- Inflammation of the pancreas or bladder.
- This may be a consequence of a congenital pathology of the beta cells of the pancreas, which are responsible for the secretion of the hormone.
- Increased physical activity or a sedentary lifestyle can cause an increase in blood glucose levels.
- Insulin may be below normal during times of stress and emotional stress.
- Any weakening of the immune system - from various infections to chronic diseases - leads to a decrease in the level of the hormone in the blood.
- The cause may be the appearance of tumors in the pancreas.
- Indicators may change after pancreatic surgery.
- Changes in the vessels that supply blood to the gland also lead to a decrease in insulin production.
- Various deviations from the norm in the amount of microelements in the body: excess iron, little protein and zinc.
- Exposure of the body to products containing cyanide.
- Low insulin with normal sugar levels is observed with excessive production of counter-insular hormones (somatotropin, adrenaline, thyroxine, glucagon, etc.).
After partial removal of the pancreas, less insulin is produced.