Shape of red blood cells - norm and deviations
80-90% of red blood cells are round cells. They have a specific shape - the shape of a biconcave disk.
But there are also cells of other shapes: flat, spiky, dome-shaped, spherical. These unusual shapes are characteristic of aging cells.
In some diseases, red blood cells of a very unusual shape may appear in a person’s blood. Such cells can be seen, for example, in sickle cell anemia. As the name suggests, the red blood cells in this disease are sickle-shaped.
Shape and structure of red blood cells
The population of red blood cells is heterogeneous in shape and size. In normal human blood, the bulk are biconcave erythrocytes - discocytes (80-90%). In addition, there are planocytes (with a flat surface) and aging forms of erythrocytes - spiny erythrocytes, or echinocytes , dome-shaped, or stomatocytes , and spherical, or spherocytes . The aging process of erythrocytes occurs in two ways - by heeling (i.e. the formation of teeth on the plasmalemma) or by invagination of areas of the plasmalemma.
During creening, echinocytes are formed with varying degrees of formation of plasma membrane outgrowths, which subsequently disappear. In this case, an erythrocyte is formed in the form of a microspherocyte. When the plasma membrane of an erythrocyte invaginates, stomatocytes are formed, the final stage of which is also a microspherocyte.
One of the manifestations of the aging process of red blood cells is their hemolysis , accompanied by the release of hemoglobin; at the same time, the so-called “shadows” of red blood cells – their membranes.
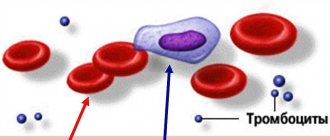
An obligatory component of the erythrocyte population are their young forms, called reticulocytes or polychromatophilic erythrocytes. Normally, they range from 1 to 5% of the total number of red blood cells. They retain ribosomes and the endoplasmic reticulum, forming granular and reticular structures that are revealed by special supravital staining. With conventional hematological staining (azur II - eosin), they show polychromatophily and are stained blue-gray.
In diseases, abnormal forms of red blood cells may appear, which is most often due to changes in the structure of hemoglobin (Hb). Replacing even one amino acid in the Hb molecule can cause a change in the shape of red blood cells. An example is the appearance of sickle-shaped red blood cells in sickle cell anemia, when the patient has genetic damage in the hemoglobin beta chain. The process of disruption of the shape of red blood cells in diseases is called poikilocytosis .
As mentioned above, normally the number of red blood cells of altered shape can be about 15% - this is the so-called. physiological poikilocytosis .
The size of red blood cells in normal blood also varies. Most red blood cells have a diameter of about 7.5 microns and are called normocytes. The rest of the red blood cells are represented by microcytes and macrocytes. Microcytes have a diameter <7, and macrocytes >8 μm. The change in red blood cell size is called anisocytosis .
The erythrocyte plasmalemma consists of a bilayer of lipids and proteins, presented in approximately equal quantities, as well as a small amount of carbohydrates that form the glycocalyx. The outer surface of the red blood cell membrane carries a negative charge.
15 main proteins have been identified in the erythrocyte plasmalemma. More than 60% of all proteins are: the near-membrane protein spectrin and membrane proteins - glycophorin , etc. lane 3 .
Spectrin is a cytoskeletal protein associated with the inner side of the plasma membrane and is involved in maintaining the biconcave shape of the erythrocyte. Spectrin molecules have the form of rods, the ends of which are connected to short actin filaments of the cytoplasm, forming the so-called. "nodal complex". The cytoskeletal protein that binds spectrin and actin simultaneously binds to the protein glycophorin.
On the inner cytoplasmic surface of the plasmalemma, a flexible network-like structure is formed that maintains the shape of the red blood cell and resists pressure as it passes through a thin capillary.
With a hereditary spectrin abnormality, red blood cells have a spherical shape. With spectrin deficiency in anemia, red blood cells also take on a spherical shape.
The connection between the spectrin cytoskeleton and the plasmalemma is provided by the intracellular protein ankerin . Ankyrin binds spectrin to the plasmalemma transmembrane protein (lane 3).
Glycophorin is a transmembrane protein that penetrates the plasmalemma in the form of a single helix, and most of it protrudes on the outer surface of the erythrocyte, where 15 separate chains of oligosaccharides that carry negative charges are attached to it. Glycophorins belong to a class of membrane glycoproteins that perform receptor functions. Glycophorins are found only in red blood cells .
Band 3 is a transmembrane glycoprotein, the polypeptide chain of which crosses the lipid bilayer many times. This glycoprotein is involved in the exchange of oxygen and carbon dioxide, which are bound by hemoglobin, the main protein of the erythrocyte cytoplasm.
Oligosaccharides of glycolipids and glycoproteins form the glycocalyx. They determine the antigenic composition of red blood cells . When these antigens bind with the corresponding antibodies, red blood cells stick together - agglutination . Antigens of erythrocytes are called agglutinogens , and the corresponding blood plasma antibodies are called agglutinins . Normally, blood plasma does not contain agglutinins to its own red blood cells, otherwise autoimmune destruction of red blood cells occurs.
Currently, more than 20 blood group systems are distinguished based on the antigenic properties of erythrocytes, i.e. by the presence or absence of agglutinogens on their surface. The AB0 system identifies agglutinogens A and B. These erythrocyte antigens correspond to α - and β -agglutinins in blood plasma.
Agglutination of red blood cells is also characteristic of normal fresh blood, and so-called “coin columns” or sludge are formed. This phenomenon is associated with the loss of charge in the erythrocyte plasmalemma. The rate of erythrocyte sedimentation (agglutination) in 1 hour in a healthy person is 4-8 mm in men and 7-10 mm in women. ESR can change significantly during diseases, for example during inflammatory processes, and therefore serves as an important diagnostic sign. In moving blood, red blood cells are repelled due to the presence of the same negative charges on their plasmalemma.
The cytoplasm of an erythrocyte consists of water (60%) and dry residue (40%), containing mainly hemoglobin.
The amount of hemoglobin in one red blood cell is called the color index. By electron microscopy, hemoglobin is detected in the hyaloplasm of the erythrocyte in the form of numerous dense granules with a diameter of 4-5 nm.
Hemoglobin is a complex pigment consisting of 4 polypeptide chains of globin and heme (iron-containing porphyrin), which has a high ability to bind oxygen (O2), carbon dioxide (CO2), carbon monoxide (CO).
Hemoglobin is able to bind oxygen in the lungs, and oxyhemoglobin . In tissues, carbon dioxide released (the end product of tissue respiration) enters red blood cells and combines with hemoglobin to form carboxyhemoglobin .
The destruction of red blood cells with the release of hemoglobin from the cells is called hemolysis . The disposal of old or damaged red blood cells is carried out by macrophages mainly in the spleen, but also in the liver and bone marrow, while hemoglobin breaks down and the iron released from the heme is used to form new red blood cells.
The cytoplasm of erythrocytes contains enzymes of anaerobic glycolysis , with the help of which ATP and NADH are synthesized, providing energy for the main processes associated with the transfer of O2 and CO2, as well as maintaining osmotic pressure and transport of ions through the plasmalemma of the erythrocyte. The energy of glycolysis ensures the active transport of cations through the plasmalemma, maintaining the optimal ratio of K+ and Na+ concentrations in erythrocytes and blood plasma, maintaining the shape and integrity of the erythrocyte membrane. NADH is involved in the metabolism of Hb, preventing its oxidation into methemoglobin.
Red blood cells participate in the transport of amino acids and polypeptides, regulate their concentration in the blood plasma, i.e. act as a buffer system. The constancy of the concentration of amino acids and polypeptides in the blood plasma is maintained with the help of red blood cells, which adsorb their excess from the plasma and then distribute it to various tissues and organs. Thus, red blood cells are a mobile depot of amino acids and polypeptides.
The average lifespan of red blood cells is about 120 days . About 200 million red blood cells are destroyed (and formed) in the body every day. As they age, changes occur in the erythrocyte plasmalemma: in particular, the content of sialic acids, which determine the negative charge of the membrane, decreases in the glycocalyx. Changes in the cytoskeletal protein spectrin are noted, which leads to the transformation of the disc-shaped erythrocyte into a spherical one. In the plasmalemma, specific receptors for autologous antibodies (IgG) appear, which, when interacting with these antibodies, form complexes that ensure “recognition” of them by macrophages and subsequent phagocytosis of such erythrocytes. As red blood cells age, their gas exchange function is impaired.
What does a normal red blood cell consist of?
Red blood cells are cells that, unlike other cells, do not have a nucleus in their structure. And therefore they cannot reproduce by division. This is probably why the name of these cells was born: “red blood cells”. This name seems to emphasize the fact that red blood cells are not exactly cells.
But, nevertheless, they, like ordinary cells, consist of an outer shell - the plasmalemma and an internal content - the cytoplasm.
On the outer membrane of red blood cells in 86% of people there is, among other things, a protein that everyone knows well as the Rh factor. If this protein is present, then they speak of Rh-positive blood. If it is not there, then the blood is Rh negative.
It is red blood cells that color the blood red. And all thanks to the fact that they contain the pigment substance hemoglobin.
Causes and symptoms
There are a number of reasons why a person’s red blood cells die. Hemolysis can occur due to certain pathologies: lupus, acute leukemia, jaundice, autoimmune diseases, myeloma. In addition, the process can begin with a genetic inferiority of the cell, aggression of antibodies against its own cells, or an excess of erythromycin cells.
Destruction begins when heavy metals enter the bloodstream, exposure to arsenic and acetic acid, severe burns, acute sepsis, and protracted chronic diseases. In addition, the phenomenon develops if blood with a different Rh factor was used during transfusion.
In the initial stages there are no manifestations. It is possible to recognize the pathological process by a number of characteristic signs. The appearance of the blood changes: the liquid becomes more red in color and becomes more transparent. The person experiences a constant feeling of nausea, and vomiting is common. There is pain and discomfort in the abdominal area. The color of the skin changes.
In severe cases, shortness of breath and convulsions are added. The skin becomes pale. There is weakness and a general asthenic state. Heart murmurs occur. Using laboratory tests, anemia can be detected. Internal organs increase in size.
Important information: What is platelet aggregation in the blood (analysis transcript)
Kinds
Intravascular hemolysis occurs due to iron deficiency, inhalation of hemolytic gases, and autoimmune pathologies. The process occurs simultaneously with the movement of blood through the vessels.
The intracellular variety is caused due to thalassemia, an autoimmune anemia. Macrophages become the site of red blood cell death.
About hemoglobin
Hemoglobin is a substance that carries oxygen from the lungs to the cells of our body. And, in addition, it ensures the delivery of carbon dioxide from cells to the lungs. That is, in the opposite direction.
The cytoplasm of each red blood cell consists of 60% water, and 40% is dry residue. If you exclude water, then 90% of these cells consist of hemoglobin.
The cytoplasm of these cells is devoid of the usual organelles, the presence of which is characteristic of all other cells. This is another significant difference between red cells and all others.
Between themselves, these blood cells differ in the degree of saturation with hemoglobin. If a cell contains a normal amount of hemoglobin, it is a normochromic cell; if there is too much of it, it is hyperchromic; if there is too little, it is hypochromic.
The overwhelming number of red blood cells in a person’s blood should be normochromic. If there are too many hypo- or hyperchromic cells, this indicates a disease.
Every medical laboratory can determine the amount of hemoglobin in one cell. This indicator is called the color indicator.
Of course, no one counts the amount of hemoglobin in each red blood cell. The average number is taken, which is obtained by dividing the total hemoglobin in the blood by the number of red blood cells in it.
Tables of norms by age
The norm of red blood cells in the blood ranges from 3.3 to 5.5 U * 1012 / per liter in adult patients.
Among women
| Age (years) | The norm is in units * 1012 per liter of blood. |
| 18-45 | 3.8-4.9 |
| 50-60 | 3.6-5 |
| 60 years and older | 3.3-5.2 |
Normal levels of red blood cells in the blood of pregnant women will be approximately the same.
In men
The normal level of red blood cells in the blood of men is 3.9 to 5.5 U * 1012 / per liter. The lower limit of values is slightly higher than for women.
| Age | Indicator in units multiplied by 10 to the 12th power per liter of blood. |
| 18-45 | 3.9-5.3 |
| 50-60 | 3.9-5.5 |
| Over 60 years old | 3.9-5.5 |
In children
| Life period | The indicator is in units multiplied by 10 to the 12th power. For one liter of blood. |
| Newborns | 3.9-5.5 |
| Up to 6 years | 3.5-4.7 |
| 6-18 years | 3.6-4.9 |
Red blood cells are designed to be amazingly equipped to do their job.
Firstly, these cells are quite large. And this, of course, increases the area of contact between hemoglobin and oxygen, and leads to the fact that each cell can transfer a fairly large amount of this gas in one “walk”. Secondly, it is not without reason that the vast majority of normal red blood cells have a specific shape - biconcave. This also increases the area of contact between hemoglobin and oxygen and increases the efficiency of each cell. Thirdly, these cells have special “tools” for their work. First of all, this is the same pigment hemoglobin. An important property of hemoglobin is that it easily and simply attaches oxygen to itself where there is a lot of it (oxygen) (in the lungs). And he lets him go there, there is little oxygen (in the tissues). The second tool that red blood cells are equipped with is a special enzyme that converts carbon dioxide into carbonic acid (in tissues). And carbonic acid, unlike carbon dioxide, easily dissolves in blood plasma. It is in the form of acid that carbon dioxide is transported to the lungs. Once in the lungs, carbonic acid breaks down (with the assistance of the same red blood cell enzyme) into water and carbon dioxide. In this case, the gas is removed from the body with exhaled air. And only a small part of this gas travels through the blood, being bound to hemoglobin. Another important feature of red blood cells is their amazing elasticity. Thanks to this property, these cells can squeeze into even the smallest capillaries. And this despite the fact that their diameter is quite large!
Life cycle of red blood cells
Red blood cells are born in the bone marrow. Every second, the bone marrow produces about 2.4 million new red blood cells.
The lifespan of red blood cells is approximately 120 days. By this time, they gradually “age” and change their shape. During death, hemoglobin is released from these cells into the blood plasma. This phenomenon is called hemolysis.
Old red blood cells are destroyed mainly in the spleen. Partially - in the liver and red bone marrow. Here they are “eaten” by special cells - macrophages. In this case, hemoglobin breaks down into its component parts, which are subsequently used by the body to synthesize new normal red blood cells.
Formation of red blood cells
The life of an individual red blood cell is relatively short - 100-120 days, and human red bone marrow reproduces about 2.5 million of these cells every day.
Full development of red blood cells (erythropoiesis) begins in the 5th month of intrauterine development of the fetus. Until this point, and in cases of oncological lesions of the main hematopoietic organ, red blood cells are produced in the liver, spleen and thymus.
The development of red blood cells is very similar to the process of human development. The birth and “intrauterine development” of red blood cells begins in the erythron - the red germ of the hematopoiesis of the red brain. It all starts with a pluripotent blood stem cell, which, changing 4 times, turns into an “embryo” - an erythroblast, and from this moment morphological changes in structure and size can already be observed.
Erythroblast . This is a round, large cell measuring from 20 to 25 microns with a nucleus that consists of 4 micronuclei and occupies almost 2/3 of the cell. The cytoplasm has a purple tint, which is clearly visible on a section of flat “hematopoietic” human bones. In almost all cells, so-called “ears” are visible, formed due to protrusion of the cytoplasm.
Pronormocyte. The dimensions of a pronormocyte cell are smaller than those of an erythroblast - already 10-20 microns, this occurs due to the disappearance of the nucleoli. The purple hue begins to lighten.
Basophilic normoblast. In almost the same cell size - 10-18 microns, the nucleus is still present. Chromantin, which gives the cell a light purple color, begins to gather into segments and the externally basophilic normoblast has a spotted color.
Polychromatophilic normoblast. The diameter of this cell is 9-12 microns. The core begins to change destructively. A high concentration of hemoglobin is observed.
Oxyphilic normoblast. The disappearing nucleus is displaced from the center of the cell to its periphery. The cell size continues to decrease - 7-10 microns. The cytoplasm becomes clearly pink with small remnants of chromantin (Joly bodies). Before entering the blood, normally the oxyphilic normoblast must squeeze out or dissolve its nucleus with the help of special enzymes.
Reticulocyte. The color of the reticulocyte is no different from the mature form of the erythrocyte. The red color provides the overall effect of the yellow-greenish cytoplasm and the violet-blue reticulum. The diameter of the reticulocyte ranges from 9 to 11 microns.
Normocyte. This is the name of a mature form of red blood cell with standard sizes, pinkish-red cytoplasm. The nucleus disappeared completely, and hemoglobin took its place. The process of increasing hemoglobin during red blood cell maturation occurs gradually, starting from the earliest forms, because it is quite toxic to the cell itself.
Another feature of red blood cells that causes a short lifespan is the absence of a nucleus does not allow them to divide and produce protein, and as a result, this leads to the accumulation of structural changes, rapid aging and death.