1
Author of the article: Marina Dmitrievna
2017.08.05
16 103
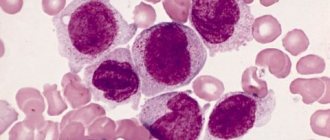
Leukocytes
Basophil and eosinophil are types of leukocytes that act as protectors of the body against various types of bacteria and infections. The deposit of basophilic and eosinophilic cells is located in the human bone marrow, from where these bodies, through the peripheral duct, enter the blood and spread throughout the body. With a normal level of the above-mentioned cells, it is generally accepted that the patient does not have any pathologies in the body, but an increased level of basophils and eosinophils, as a rule, indicates serious abnormalities requiring immediate medical intervention.
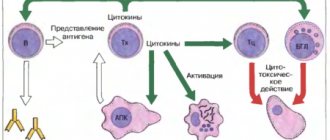
What are lymphocytes and their role in the immune system.
Blood is the only tissue of its kind in the human body. It consists of a liquid part, plasma, which contains several types of cells. These are red blood cells, white blood cells and platelets. Their number and ratio are different for men and women, and also depend on age.
Each of these groups performs its own specific functions. Red blood cells contain a special protein, hemoglobin. In the lungs it combines with oxygen, carries it to the tissues, “exchanges” it for carbon dioxide, which is returned to the lungs. Platelets are the main element of the blood coagulation system. They maintain the integrity of the vascular wall and help stop bleeding.
Leukocytes represent the body's defense system. By their number, you can not only identify the acute or chronic course of the disease, but also the state of the human immune system as a whole. This name combines a group of cells that differ in appearance and mechanism of response to stimuli. The fact is that viruses, bacteria, fungi, and allergens are different from each other, therefore the immune bodies must also be structured differently to fight them. This:
- neutrophils, thanks to the function of phagocytosis, absorb and digest viruses and bacteria;
- eosinophils are involved in the formation of allergic reactions;
- basophils, their functions are not fully understood;
- lymphocytes ensure the normal functioning of all parts of the immune system. Up to 80% of their number are T lymphocytes. Killer T cells react to foreign cells and destroy them. Helper T cells recognize pathogenic microorganisms and initiate a protective response. Suppressor T cells suppress the body's autoimmune reactions. B lymphocytes produce immunoglobulins that neutralize bacteria. NK lymphocytes react to their own cells when they degenerate during malignant processes or the introduction of a virus;
- monocytes accelerate wound regeneration and participate in the development and inhibition of inflammation.
The synthesis of “young” lymphocytes occurs in the bone marrow. They finally “mature” in the spleen, lymph nodes and thymus. The function of this organ in the immune system was discovered by scientist Jackie Miller. The lifespan of these cells is about three months. They are found in the general bloodstream and, if necessary, are delivered to the site of localization of the infectious process.
Reasons for increased levels of leukocytes and lymphocytes in the blood
If leukocytes or lymphocytes are elevated in a person’s blood, this is a serious reason to seek help from a specialist. This condition indicates the presence of pathology in the body.
The main function of leukocytes and lymphocytes is to protect the human body from all kinds of diseases. A change in the level of blood cells characterizes the fact that the immune system mobilizes all its forces to fight foreign bodies. If a high concentration of leukocytes and lymphocytes is detected, we can talk about infection of the body. A specialist, having studied all the information and summarized all the tests and symptoms, can draw a conclusion about the nature of the infection (viral, bacterial), whether the disease is autoimmune in nature or a blood disease.
The mechanism of development of lymphocytosis
What is lymphocytosis and what causes it? Blood “works” as transport for lymphocytes. The main amount is concentrated in organs - depots. These are the spleen, bronchial vessels, lymph nodes. This determines their relatively low number in normal clinical analysis data. However, when any infectious agent enters through damage to the skin, mucous membrane of the genital organs, mouth, and nose, an immune response develops.
The release of various types of lymphocytes begins from the depot, which causes an increase in their concentration in the total number of leukocytes. It can be absolute or relative. If the symptoms of increased lymphocytosis consist in the percentage predominance of this type of formed elements without changing their total amount in the blood, they speak of a relative increase. If the analysis notes an increase in their overall value, then this is absolute T lymphocytosis (although it is worth noting that all types of these cells are released).
Causes and forms of eosinophilia
The severity of eosinophilia is determined by the number of eosinophils in the blood. She may be:
- Lung - the number of cells does not exceed 10%;
- Moderate - up to 20%;
- Severe (high) - more than 20% of eosinophils in the peripheral blood.
If a blood test shows an excess of eosinophils in relation to other populations of leukocytes, the doctor will calculate their absolute number based on the percentage, and then it will become clear whether eosinophilia is relative or absolute. More reliable data are obtained by directly counting eosinophils in a counting chamber, after diluting the blood with special liquids.
eosinophilia in the blood
The number of diseases accompanied by eosinophilia includes several dozen nosological forms, and all of them can be combined into groups:
- Parasitic infestations;
- Infectious pathology;
- Allergic reactions;
- Autoimmunization;
- Immunodeficiency conditions;
- Reactions to drugs;
- Malignant tumors, including the hematopoietic system;
- Rheumatic diseases;
- Damage to internal organs;
- Skin diseases.
Parasitic infestations are one of the most common causes of eosinophilia. Pediatricians often encounter it, and many mothers know that slight eosinophilia in the blood of a baby who has begun to actively explore the world around him is most often associated with infection with worms.
Among helminthic diseases accompanied by eosinophilia, one can note ascariasis, trichinosis, opisthorchiasis, filariasis, echinococcosis, the introduction of Giardia, amebiasis and others. Eosinophilia in this case will be a sign of an immune-allergic reaction that develops in response to parasite invasion.
To a greater extent, an increase in eosinophils will be noticeable in those diseases when, at some stage, the parasite migrates throughout the body, entering the tissues, or is there as a mature individual. The migration of larval forms is accompanied by ascariasis, strongyloidiasis, and echinococcal cysts, trichinella, and filariae are constantly present in the tissues.
Just a few decades ago, many parasitic diseases were characteristic of a strictly defined area or climate. For example, residents of tropical countries knew about filaria, and Siberia and the Far East were characterized by a higher prevalence of opisthorchiasis. Today, thanks to the active movement of the planet's inhabitants and the possibility of long-distance travel, the area of occurrence of many diseases has expanded, so a doctor who has detected eosinophilia in a patient must certainly find out which countries or regions the latter has visited in the near future.
With trichinosis, the introduction of echinococcus, and opisthorchiasis, eosinophilia reaches significant figures - more than 40%, which is associated with the constant presence of the parasite in human tissues. Other infestations may cause little or no eosinophilia. For example, the well-known pinworms (enterobiasis) do not always lead to changes in blood counts, as do intestinal parasites (tapeworms, whipworms).
Video: eosinophils, their main functions
Many infections with pronounced symptoms of allergy to the pathogen and its metabolic products show eosinophilia in a blood test - scarlet fever, tuberculosis, syphilis. At the same time, eosinophilia during the recovery stage, which is temporary, serves as a favorable sign of the beginning of recovery.
Allergic reactions are the second most common cause of eosinophilia. They are becoming more common due to the deterioration of the environmental situation, the saturation of the surrounding area with household chemicals, the use of various medications, and food products replete with allergens.
eosinophils perform their function in the “problem” lesion
Eosinophil is the main “actor” in the focus of an allergic reaction. It neutralizes biologically active substances responsible for vasodilation and tissue swelling due to allergies. When an allergen enters a sensitized (sensitive) body, eosinophils immediately migrate to the site of the allergic response, increasing in both the blood and tissues.
Among allergic conditions accompanied by eosinophilia, bronchial asthma, seasonal allergies (hay fever), diathesis in children, urticaria, and allergic rhinitis are common. This group also includes allergies to medications - antibiotics, sulfonamides, etc.
Skin lesions in which the immune response is pronounced with symptoms of hypersensitization also occur with eosinophilia. These include infection with the herpes virus, neurodermatitis, psoriasis, pemphigus, eczema, which are often accompanied by severe itching.
Autoimmune pathology is characterized by the formation of antibodies to one’s own tissues, that is, the body’s proteins begin to attack not someone else’s, but their own. An active immune process begins, in which eosinophils also participate. Moderate eosinophilia manifests itself in systemic lupus erythematosus and scleroderma. Immunodeficiencies can also provoke an increase in the number of eosinophils. These include mainly congenital diseases (Wiskott-Aldrich syndrome, T-lymphopathies, etc.).
Taking many medications is accompanied by activation of the immune system with the production of excess eosinophils, while there may be no obvious allergy. Such medications include aspirin, aminophylline, beta-blockers, some vitamins and hormonal drugs, diphenhydramine and papaverine, drugs for the treatment of tuberculosis, certain antihypertensive drugs, spironolactone.
Malignant tumors may have eosinophilia as a laboratory symptom (Wilms tumor, cancer metastases on the peritoneum or pleura, skin and thyroid cancer), others directly affect the bone marrow, in which the maturation of certain cells is impaired - eosinophilic leukemia, myeloid leukemia, polycythemia vera and etc.
Internal organs, damage to which is often accompanied by an increase in eosinophils, are the liver (cirrhosis), lungs (sarcoidosis, aspergillosis, Loeffler's syndrome), heart (defects), intestines (membranous enterocolitis).
In addition to the listed diseases, eosinophilia appears after organ transplant operations (with immune rejection of the transplant), in patients on peritoneal dialysis, with a lack of magnesium in the body, after irradiation.
In children, eosinophil levels are somewhat different. In newborns, they should not be higher than 8%, and before the 5th birthday, a maximum value of eosinophils in the blood of 6% is allowed, which is due to the fact that immunity is just being formed, and the child’s body is constantly faced with new and hitherto unknown potential allergens.
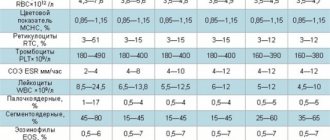
Table: average values of eosinophils and norms of other leukocytes in children by age
The causes of eosinophilia in children are similar to those in adults, but allergies (especially food allergies) and parasite damage are of paramount importance. In the first year of life, the digestive system is formed and adapted to the intake of a variety of foods. During this period, the baby encounters food allergens that act on the too permeable intestinal mucosa, causing severe diathesis (skin reactions), bronchial obstruction, and urticaria.
Starting from the second year, the role of infectious pathology and parasite infection in the appearance of eosinophilia (scarlet fever, tuberculosis, enterobiasis, giardiasis, etc.) increases, but diathesis may not go away by this age if the child is allergic from birth.
Clinical blood test and its interpretation
Lymphocytosis is shown by a general blood test, which is done in the laboratory within 1 to 2 hours. Based on the number of other formed elements and their ratio, the doctor suggests the cause and nature of the disease. The blood test form is a table that lists the indicators, how many of them actually exist in a particular patient and the norm for adults and children. Let us dwell on them, since this is part of the diagnosis of lymphocytosis.
- ESR (erythrocyte sedimentation rate) – up to 15 mm/hour. During an inflammatory reaction, special substances appear in the blood that increase the adhesion of such cells.
- Leukocytes (4.0 – 9.0 × 109 cells/liter) are no less important indicator than lymphocytes. An increase in their concentration (leukocytosis), especially in combination with an acceleration of ESR, indicates a severe bacterial infection. Lymphocytosis with leukopenia (decreased amount) means a viral disease.
- Red blood cells (3.7 – 5.0 × 109 cells/l). When the blood thickens, which often accompanies dehydration, their number increases; a decrease is usually noted after massive bleeding.
- Hemoglobin (120 – 160 g/l) shows the ability of blood to be saturated with oxygen and carry it. A number below normal means the appearance of symptoms of anemia.
- Hematocrit, color index, mean erythrocyte volume, and platelet count play a role in the diagnosis of specific rare blood diseases and are not usually associated with lymphocytosis.
- Lymphocytes. The form has two values - absolute (1.32 - 3.57 × 109 cells/l) and relative (19 - 37%). It is by these indicators that the type of lymphocytosis is determined.
- Monocytes (0.24 – 0.82×109 cells/l and 3 – 10%). An increase (monocytosis) indicates a protracted course of some diseases of a bacterial nature (for example, tuberculosis). This is also a specific symptom of infectious mononucleosis.
- Eosinophils (0.04 – 0.54×109 cells/l and 0.5 – 5.0%). Exceeding the norm is called eosinophilia. This means allergies, parasitic infestations. This phenomenon is also observed during recovery.
The number of neutrophils is indicative when deciphering the leukocyte formula. Pay attention to their ratio in terms of maturity. Doctors call this a left or right shift. Neutropenia or granulopenia (content below normal) simultaneously with lymphocytosis more often indicates an acute severe viral disease.
Treatment of eosinophilia
After identifying the true cause of the change in the blood formula, treatment is carried out by a specialist doctor. In case of blood pathology, this is a hematologist; if the prerequisite for the development of the condition was parasites - an infectious disease specialist; allergies will be cured by an allergist; lungs - pulmonologist and so on. There is no single way to get rid of eosinophilia; the doctor takes into account the patient’s age, concomitant diseases, general health, medications taken and many other factors on an individual basis.
You should also not be upset if eosinophils are moderately elevated; this may indicate the beginning of recovery and the formation of a healthy immune system response to the infection. Let the doctor do his job and strictly follow his recommendations.
Leukocyte formula (leukogram) is the percentage of the main types of leukocytes: neutrophils, eosinophils, basophils, lymphocytes and monocytes.
Neutrophils
Neutrophils are the most numerous group of leukocytes. Depending on the degree of maturity, young, band and segmented neutrophils are distinguished. The main function of neutrophils in the body is phagocytosis of microorganisms. The lifespan of neutrophils is 5–9 days.
Limits of the normal content of neutrophils in the leukocyte formula:
| Adults | 47 – 72 % |
| Children under 1 year | 15 – 45 % |
| 16 years | 25 – 60 % |
| 6 – 12 years | 35 -65 % |
| 12 – 16 years old | 40 – 65 % |
Band neutrophils normally make up 1–6%.
An increased level of neutrophils in the leukocyte formula occurs when:
- Infectious diseases: bacterial, fungal (candidiasis), spirochetosis, some viral, rickettsial, parasitic
- Inflammatory process: rheumatism, rheumatoid arthritis, ischemic necrosis, gout, colitis, pancreatitis, nephritis, myositis, thyroiditis, dermatitis, peritonitis
- Intoxication: diabetes mellitus, uremia, eclampsia, hepatocyte necrosis
- Blood diseases: myeloproliferative diseases, condition after removal of the spleen (splenectomy), hemolytic anemia, hemorrhage, chronic idiopathic leukemia
- Smoking
- Mental and emotional agitation
- Exposure to high (low) temperatures, physical activity, pain, injury, burns, pregnancy, childbirth, anorexia, after surgery
- Malignant neoplasms: tumors of various localizations
- Taking acetylcholine, chlorpropamide, corticosteroids, corticotropin, digitalis, endotoxins, epinephrine, ethylene glycol, heparin, insecticides, norepinephrine, potassium chlorate, tarpentine, histamine
- Lead and mercury poisoning
- Consumption of casein (found in fermented milk products)
A reduced level of neutrophils in the leukocyte formula occurs when:
- Infectious diseases: bacterial (typhoid, paratyphoid, brucellosis), viral, debilitating infections
- Blood diseases: aplastic anemia, subleukemic acute leukemia, idiopathic neuropathy, hypersplenism, megaloblastic anemia, anemia due to decreased bone marrow function, iron deficiency anemia, paroxysmal nocturnal hemoglobinuria
- Other diseases, such as anaphylactic shock, hypothyroidism, thyrotoxicosis, hypopituitarism, liver cirrhosis, periodic neutropenia, congenital neutropenia, Chediak-Higashi syndrome
- Hypersensitivity to painkillers, anticonvulsants, antihistamines, antimicrobial, antithyroid, antiviral, cardiovascular, diuretic, hypoglycemic and other drugs taken
- Use of antitumor drugs
An increase in the number of young and band neutrophils in the blood: indicates the presence of blood loss or an acute inflammatory process in the body.
Eosinophils
Eosinophils are motile cells capable of phagocytosis, but their phagocytic activity is lower than that of neutrophils. The role of eosinophils has been established in reactions to foreign proteins, in allergic and anaphylactic reactions, where they participate in the metabolism of histamine produced by mast cells of connective tissue. They play an important role in anthelmintic immunity. Eosinophils remain in the peripheral blood for less than 12 hours and then pass into the tissues. Their targets include organs such as the skin, lungs and gastrointestinal tract.
Normal limits for the content of eosinophils in the leukocyte formula:
| Adults | 0,5 – 5,0 % |
| Children under 12 years old | 0,5 – 7,0 % |
| 12 – 16 years old | 0,5 – 6,0 % |
An increased level of eosinophils in the leukocyte formula occurs when:
- Allergic reactions to drugs such as anticonvulsants (carbamazepine, chloramphenicol), antibiotics (erythromycin, penicillin, tetracyclines, vancomycin), sulfonamides, antituberculosis drugs, phenothiazides
- The use of aminosalicylic acid, chlorpropamide, imipramine, mephenesin, nitrofurantoin, penicillin, sulfasalazine, sulfonamides (in all these cases, eosinophilia is part of Loeffler's syndrome)
- Use of allopurinol, dapsone, etretinate, methotrexane, methyldopa, nafarelin, penicillamine, procarbazine, triamterene
A reduced level of eosinophils in the leukocyte formula occurs when:
- Purulent infections, after childbirth, surgery, shock
- Taking corticotropin, epinferin, glucocorticoids, methysergide, niacin (nicotinic acid), procainamide
Basophils
Basophils mediate inflammation and secrete eosinophil chemotactic factor. Basophil degranulation occurs in immediate hypersensitivity reactions (eg, asthma, anaphylaxis, rash that may be associated with reddening of the skin). The trigger mechanism for anaphylactic degranulation is the receptor for immunoglobulin class E. Basophils, releasing heparin and histamine, participate in the regulation of blood coagulation and vascular permeability. Basophils remain in the peripheral blood for about 1–2 hours.
Limits of the normal content of basophils in the leukocyte formula:
| Adults | 0,0 – 1,0 % |
An increased level of basophils in the leukocyte formula occurs when
- Myxedema, ulcerative colitis, chronic sinusitis, chickenpox, hypersensitivity reactions to foods, use of certain medications or inhalants
- Reactions to the introduction of a foreign protein, nephrosis, chronic hemolytic anemia, Hodgkin's disease, condition after removal of the spleen (splenectomy)
- Taking estrogens, antithyroid drugs, desipramine
A reduced level of basophils in the leukocyte formula occurs when:
- Hyperthyroidism
- Ovulation, pregnancy, stress
- Acute infectious diseases
- Cushing's syndrome
- The use of corticosteroids, corticotropin, chemotherapy, procainamide, thiopentane, X-ray irradiation
Lymphocytes
Among lymphocytes, there are three main functional classes: B lymphocytes, T lymphocytes and null lymphocytes. The main function of lymphocytes is participation in immune reactions. The main function of B lymphocytes is to provide humoral immunity, T lymphocytes are to provide cellular immune reactions and regulate humoral immunity. Null lymphocytes are regarded as a reserve population of undifferentiated lymphocytes. The lifespan of lymphocytes varies from several weeks to several years.
Normal limits for the content of lymphocytes in the leukocyte formula:
| Adults | 19 – 37 % |
| Children under 1 year | 38 – 74 % |
| 16 years | 26 – 60 % |
| 6 – 12 years | 24 – 54 % |
| 12 – 16 years old | 22 – 50 % |
An increased level of lymphocytes in the leukocyte formula occurs when
- Infectious diseases (infectious mononucleosis, infectious lymphocytosis, viral hepatitis, cytomegalovirus infection, whooping cough, toxoplasmosis, herpes virus type 6, rubella, acute HIV infection)
- Taking albuterol, aminosalicylic acid, epinephrine, griseofulvin, isoproterenol, levodopa, narcotic analgesics, niacinamide, norepinephrine, phenytoin, mephenytoin, organic arsenic compounds, valproic acid
- Poisoning by carbon disulfide, lead or tetrachloroethanol
A reduced level of lymphocytes in the leukocyte formula occurs when:
- Blood diseases: lymphocytic leukemia, lymphosarcoma, heavy chain diseases
- Acute infections and diseases, miliary tuberculosis, lymphogranulomatosis, systemic lupus erythematosus, aplastic anemia, renal failure, terminal stages of cancer
- Immunodeficiency conditions associated with a decrease in the number of T-lymphocytes
- The use of antilymphocyte serum, asparaginase, chlorambucil, corticotropin, glucocorticoids, lithium, mechlorethamine, methysergide, niacin
- After radiation sessions during X-ray therapy
Causes of lymphocytosis and its types
Lymphocytosis in adults is diagnosed when the number of these blood cells exceeds 3.74 × 109 cells per liter (absolute form) or 37% (relative type). First of all, it is worth noting that sometimes such a symptom occurs for completely physiological reasons. This could be stress, lack of sleep, or in women the first days of menstruation. In addition, there are several types of increases in the number of leukocytes in the blood. Reactive or benign lymphocytosis develops against the background of:
- viral respiratory infections, influenza, mononucleosis (an atypical type of monocytes also appears - mononuclear cells), chickenpox, cytomegalovirus;
- initial stages of HIV;
- such severe acute or chronic bacterial diseases as tuberculosis, typhoid fever, syphilis, tonsillitis;
- parasitic infections (toxoplasmosis);
- autoimmune pathologies;
- disorders of the thyroid gland;
- food poisoning, ingestion of chemical toxins, overdose of drugs or medications;
- bronchial asthma, eczema, psoriasis.
The causes of lymphocytosis ((in Latin lymphocytosis), as lymphocytosis is called in other words, can also be side effects of certain medications, these are antibiotics, sulfonamides, anti-inflammatory drugs. Immunosuppressants (for example, like Azathioprine), steroids and cytostatics, on the contrary, lead to deficiency neutrophil cells, leukopenia and anemia.The simultaneous combination of a constant relative and absolute increase in the number of lymphocytes indicates oncology (acute or chronic lymphocytic leukemia, thymoma, etc.).It should be emphasized that such a condition requires immediate treatment.
Infectious lymphocytosis deserves special attention. This disease is caused by a lymphotropic virus. The routes of transmission and the mechanism of its development have not been fully studied to date. Its feature is simultaneous leukocytosis.
Clinical picture
Symptoms of lymphocytosis are different and are determined by the disease, which provoked deviations from the norm in blood test parameters. Typically, clinical manifestations develop gradually. Those who develop the pathology complain of decreased ability to work, drowsiness, and a feeling of constant fatigue. Then the following may appear:
- increase in temperature, specific numbers are determined by the type of pathology and individual characteristics, usually this value ranges from 37.3 to 38°;
- catarrhal phenomena, this is pain and redness of the throat, hoarseness, possibly cough, nasal congestion;
- lacrimation;
- an increase in the size of the lymph nodes (this is especially pronounced in acute mononucleosis);
- a rash may appear;
- reluctance to eat.
With a common ARVI, these symptoms disappear after 7–9 days, even in the absence of treatment. If the temperature persists (or rises) and the patient's condition worsens, this may indicate bacterial complications. In this case, you need to repeat a general clinical blood test. Symptoms of acute malignant lesions of the hematopoietic system develop quickly. Note:
- weakness;
- pallor;
- attacks of dizziness;
- nausea or vomiting;
- constant, successive respiratory infections.
Autoimmune diseases manifest themselves in different ways. A rash that looks like bruises or reddened spots may appear on the body or face. The temperature persists for a long time, although there are no other symptoms characteristic of ARVI. Then morning stiffness of movements, swelling of the joints, and nodular rash on the skin appear.
Diagnostics
When contacting a physician, diagnosis begins with a physical examination and medical history. The presence of lymphocytosis can only be determined through clinical studies. To do this, the patient donates blood for a general clinical blood test. Collect material in the morning. Before the analysis, the patient must inform the attending physician about what medications he took during the day. This information is important because taking certain medications affects your white blood cell count and can skew your results.
In addition to the general detailed clinical analysis, the following studies are carried out:
- for the presence of antibodies;
- immunophenotyping of lymphocytes to determine cell structure and lymphoblast profile;
- cytological examination of lymph node tissue - to exclude malignant tumors;
- bone marrow myelogram for comparison with the clinical picture provided by a peripheral blood test;
- if monocytes and lymphocytes exceed normal values, then this gives reason to assume that the patient has myelodysplastic syndrome or monocytic leukemia.
The diagnosis is made based on the following points:
- An increase in the blood lymphocyte formula and a decrease in the number of platelets - thrombocytopenia, indicates hypersplenism and autoimmune thrombocytopenic purpura. Hypersplenism is when the spleen quickly disposes of dead or spent blood cells along with healthy cells. It is also an accompanying symptom of liver diseases, blood diseases, spleen injuries and some types of lymphomas and leukemia.
Spleen in the human body
- Leukopenia, which is a symptom of a complication of a viral disease, including tuberculosis.
- Simultaneous increase in the level of red blood cells and lymphocytes. It is observed in bacterial and viral infections, which are accompanied by dehydration of the body - loose stools, vomiting, elevated body temperature, fever.
- Imbalance with a simultaneous decrease in lymphocytes and leukocytes.
Since lymphocytosis often accompanies oncological diseases, if there are no clinical symptoms of infectious diseases, the doctor prescribes additional examination:
- blood test for tumor markers;
- tomography - computed tomography or magnetic resonance imaging;
- ultrasound examination of the abdominal and pelvic organs;
- X-ray examination;
- fibrogastroduodenoscopy;
- If any formations are detected, a tissue biopsy is indicated.
Differential diagnosis
As doctors emphasize, it is not tests that need to be treated, but a specific disease. Before starting therapy, the exact cause of lymphocytosis should be established. For this purpose, one general blood test is not enough. To diagnose a respiratory infection, a thorough examination of the patient is necessary, listening to wheezing in the bronchi or lungs to exclude pneumonia.
Measles, rubella, and chickenpox are accompanied by the appearance of a characteristic rash. Mononucleosis occurs in the form of a sore throat, accompanied by severe enlargement of the lymph nodes. Although, to clarify the type of virus, additional tests for lymphocytosis, such as PCR, should be done. This is a way to detect the DNA of the pathogen.
In terms of diagnostics, autoimmune diseases are difficult, especially if there are no other symptoms other than lymphocytosis. A specific marker for such pathologies is an increase in antibody titer in the ANA analysis. Then, if the result is positive, the presence of a number of interleukins, peptides and other protein compounds is checked. They are specific and are produced for any one type of autoimmune disease.
Oncology is diagnosed in a similar way. Additionally, it is necessary to do an ultrasound of the internal organs. Long-term chronic lymphocytosis is characterized by hepato- and splenomegaly (an increase in the size of the liver and spleen, respectively). Hearts and joints are also checked. It is necessary to emphasize that lymphocytosis is a condition that persists for several weeks after recovery (this form is called post-infectious).