Hyperglycemic coma occurs acutely when the course of uncontrolled diabetes mellitus enters the decompensation stage. Its main cause is the sudden onset of glycemia due to an absolute or relative lack of production of the hormone insulin by the pancreas. This pathological condition cannot go away on its own without the participation of medical workers and hospitalization. Emergency care for hyperglycemic coma should be provided in the very first seconds after its occurrence, so people who come into contact with diabetics are advised to know what to do in such a situation.
SD
Causes
There are several causes of hyperglycemic coma, and they are divided into 2 groups. The first includes incorrect treatment, an unidentified diagnosis of diabetes mellitus, errors in insulin dosage, diet violations, the use of low-quality drugs for treatment or expired drugs that do not give the desired effect, as well as insulin withdrawal.
The second includes the following conditions and diseases:
- severe stress (it has been established that during stress, blood glucose levels increase markedly);
- pancreatic necrosis (necrosis of the pancreas, as a result of which its production of insulin decreases);
- injuries of various locations and surgical interventions;
- some inflammatory and infectious diseases.
If a precomatose state or coma develops, it is necessary to very quickly find the cause that led to these consequences and eliminate it as soon as possible, if possible.
The occurrence of hyperglycemic coma is possible with uncompensated diabetes mellitus of any type.
Diagnostics
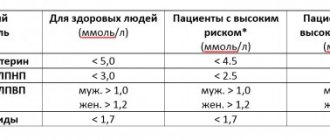
Making a correct diagnosis is not so easy, as you need to take a blood test for sugar or check its level using a glucometer.
A rapid blood test is a mandatory condition when a patient is admitted to the intensive care unit of a hospital, but even this is not enough, since in a comatose state caused by hypoglycemia, any delay can cost the patient’s life.
A regular blood test (biochemical or general) takes a very long time. In our case, it is necessary to obtain results a few minutes after the patient’s admission.
But a situation is also possible when coma can occur even at relatively high glycemic values.
For example, in those diabetics whose sugar previously remained at very high levels, and after taking new drugs for it (glycemic drugs like metformin), glycemia dropped sharply. Such a drop provokes the launch of the body’s defense mechanisms, which over several years of hyperglycemia have already managed to somewhat adapt to such sugary conditions.
Do not sharply lower your glucose level! The same applies to blood pressure.
For example, a patient with type 2 diabetes was switched to insulin therapy and unknowingly administered slightly more insulin than was recommended by the doctor. In response to this, the body began to intensively consume glucose, the concentration of which dropped significantly in a few minutes from 22.0 mmol/liter to 11.1 mmol/l. Afterwards, the man felt very weak, he became dizzy, his vision became blurred, and he began to sink to the ground, almost losing consciousness.
Therefore, any doctor on duty in an ambulance will take the only correct decision in a comatose state of a person - he will urgently administer the nth dose of glucose. He will do the same in case of hyperglycemic coma and he will be right, since death as a result of coma with a deficiency of glucose occurs much faster than with its excess.
Symptoms of hyperglycemic coma
Hyperglycemic coma is a condition that does not develop immediately. It is preceded by a long process of accumulation of glucose in the bloodstream, which lasts from several days to a week, during which there is an increase in such symptoms as:
- polyuria (frequent urination), which is abruptly replaced by acute urinary retention;
- polydipsia (a state of unquenchable thirst, dry mouth);
- weight loss;
- dehydration;
- weakness and decreased performance;
- skin itching;
- poor wound healing;
- dry skin;
- nausea and vomiting;
- disturbance of consciousness.
When examining the patient, you may notice that the skin is pale, dry and cold. Breathing is shallow, frequent and noisy. Chest movements are active. Eyeballs, usually sunken, without movement. There may be an odor of acetone from the mouth. There is a decrease in blood pressure. No physical activity. If this condition is not stopped soon, death is possible.
By the way, we recommend reading the article Gestational diabetes mellitus during pregnancy: what you need to know
Clinical picture
The disease develops slowly, from several hours to several days. During this time, the patient clearly exhibits symptoms - signs of a diabetic coma. If measures are not taken, precoma will occur, and then the patient will fall into an unconscious state. Staying in this state for more than a day without medical care in a hospital will lead to death.
According to statistics, diabetics in old age rarely develop hyperglycemic coma. It is also rarely recorded in patients with T2DM. Children and adolescents, who are characterized by a state of mental and hormonal instability, are most at risk. Often it is gross deviations from the diet in children, uncontrolled by parents, that lead to an attack.
30% of diabetic patients were first diagnosed while they were in a precoma state.
Signs of a diabetic coma
Gradual dehydration and intoxication caused by high concentrations of glucose in the blood are externally manifested as follows:
- Increasingly persistent thirst;
- Increased urination (at the beginning of the process);
- Stopping urination (in a state of precoma);
- Headache;
- Abdominal pain, vomiting, nausea;
- Diarrhea, constipation (precoma);
- Weakness;
- Low blood pressure (precoma);
- Low temperature (precoma);
- Dry skin;
- Redness of the face;
- Tachycardia (precoma);
- Decreased muscle tone;
- Noisy breathing with the smell of acetone (precom).
Urgent Care
Anyone may encounter a situation where it is necessary to provide first aid before medical workers arrive. If you suspect that a person is in a hyperglycemic coma, you need to perform the following algorithm:
- Determine whether there is a pulse (you can do this on any vein or artery. The easiest way to do this is on the neck or hand).
- Check for foreign objects in the mouth (such as dentures or food).
- Turn the person on their side to prevent tongue retraction or suffocation due to vomit.
- Wait for the doctors to arrive, and if the patient has a phone, call relatives.
Complications and prognosis
The consequences for the body in the described case depend on the general health of the patient, his age and the time during which he was in a coma. Hypoglycemic coma is not as dangerous to health and life as diabetic coma, so deaths are rare and the overall prognosis is favorable. However, if the syndrome occurs regularly, chronic interruptions in the supply of carbohydrates to the brain can eventually cause irreversible consequences in its tissues due to cell death.
As a rule, we are talking about cerebral pathologies, including dementia and motor disorders. In addition, if the patient has a history of cardiovascular diseases, there is a risk of myocardial infarction or stroke during a hypoglycemic coma (retinal hemorrhage is also likely). In other cases, the recovery of a person who has suffered a similar syndrome occurs normally and quickly, right up to its original state.
Treatment
The treatment for hyperglycemic coma, regardless of the cause, is insulin therapy.
Therapy is carried out in a medical institution. If the patient is in a state of precoma, then treatment consists of administering insulin and measuring blood glucose levels hourly. Timely treatment will prevent the development of coma.
If the patient is already in a coma, then he needs urgent medical attention. This assistance includes the following activities:
- transfer to artificial ventilation, installation of a tracheostomy;
- installation of a urinary catheter;
- insulin therapy (carried out with short-acting insulin);
- blood glucose control;
- replenish the volume of circulating blood by infusing saline or Ringer's solution (i.e., reduce dehydration);
- administration of a 5% glucose solution after stabilizing blood sugar levels (to restore the internal environment of the body);
- replenishment of electrolyte losses by drip infusions;
- detoxification (removing toxins from the body).
In addition, the hospital performs general and biochemical blood tests several times a day, as well as a urine test for ketone bodies. After the neurological symptoms have disappeared and the person has regained consciousness, it is recommended to perform a CT scan of the brain. It is used to determine whether there are any organic lesions in the brain.
The rehabilitation period is different for each person and depends on the severity of the metabolic disorder. After drug correction of the coma, which takes several days, the patient is transferred to the endocrinology department.
At the next stage of treatment, it is necessary to establish the cause of this pathology. You may need to consult other specialists (cardiologists, surgeons, gastroenterologists) and perform instrumental examinations (ultrasound diagnostics).
In the future, the task of the patient and the attending physician is to select the correct dose of insulin, which will keep the sugar level normal.
Resuscitation actions
Indications for resuscitation measures are:
- lack of breathing or pulse;
- heart failure;
- blue discoloration of the skin surface;
- absence of any reaction of the pupils when light hits them.
If you have these symptoms, you should not wait for the ambulance to arrive.
The patient's relatives should begin to act independently according to the following recommendations:
- Place the patient on a hard surface.
- Open access to the chest, freeing it from clothing.
- Tilt the patient's head back and place one hand on his forehead, and with the other push the lower jaw forward to ensure airway patency.
- Remove food debris from the mouth (if necessary).
When performing artificial respiration, it is necessary to firmly touch your lips with the patient’s mouth, having first placed a napkin or a piece of clean cloth on it. Then you need to take deep exhalations, closing the patient’s nose in advance. The effectiveness of the actions taken is determined by the raising of the chest at this moment. The number of breaths per minute can be up to 18 times.
To perform indirect cardiac massage, the hands should be placed on the lower third of the patient’s sternum, located on the left side of him. The basis of the procedure is energetic pushes made towards the spine. At this moment, the surface of the sternum should shift by a distance of 5 cm in adults and 2 cm in children. You need to perform about 60 presses per minute. When combining such actions with artificial respiration, each breath should alternate with 5 compressions on the chest area.
The described steps should be repeated until the doctors arrive.
Video lesson on resuscitation measures:
Medical measures:
- In case of ketoacidosis coma, it is necessary to administer insulin (first in a stream manner, and then in a drip method with dilution in a glucose solution to prevent hypoglycemia). Additionally, sodium bicarbonate, glycosides and other agents are used to maintain heart function.
- In case of hyperosmolar coma, infusion drugs are prescribed to replenish fluid in the body, and insulin is administered intravenously by drip.
- Lactic acidosis is eliminated by using the antiseptic Methylene Blue, Trisamine, sodium bicarbonate solution, and insulin.
The actions of specialists depend on the type of coma and are performed in a hospital setting.
Hyperglycemic coma in children
Hyperglycemic coma is a terrible complication that can occur in diabetics of any age, children are no exception. In children, this is most often a consequence of type 1 diabetes mellitus, which is typical for children and young adults.
In a child, just like in an adult, with elevated blood sugar levels, intoxication of the brain occurs, and subsequently a disturbance and loss of consciousness.
By the way, we recommend reading the article Can diabetes give you disability?
Often, the first manifestation of diabetes is hyperglycemic coma, that is, the parents did not know about the existence of diabetes in the child. The root causes and symptoms of hyperglycemic coma are exactly the same as in adults. If treatment is not carried out on time, the child's life is at risk.
The danger lies in the fact that the child cannot objectively assess his well-being or suspect any symptoms. Responsibility for this lies entirely with the parents; it is important to be attentive to the health of their children. Doctors urge routine medical examinations, even if the child is not worried .
Unfortunately, undetected diabetes mellitus threatens such a serious complication as hyperglycemic coma. Late resuscitation measures reduce the percentage of successful outcome.
Consequences
Unfortunately, if the coma lasts for a long time, its consequences may be irreversible. This primarily concerns the nervous system. Glucose intoxication can have a detrimental effect on the brain. Memory impairment, confusion, and even swelling of brain tissue are possible. In addition, since vomiting is possible during a coma, the entry of vomit into the lungs can provoke pneumonia.
Children who have suffered this condition may also have the above-mentioned consequences. The role of parents and doctors is to prevent this complication from happening again.
Prevention
Glucometer
Any condition is easier to prevent than to treat. First, once diabetes is diagnosed, you must strictly follow your doctor's orders. Compliance with a diet, dosed physical activity and correct drug therapy will reduce the risk of coma to zero. You should independently check the expiration date of medications and insulins and do not use them after the expiration date has expired. Medicines must be stored according to storage conditions.
Diabetics should monitor their blood glucose levels at home with a glucometer, and if diabetes decompensates, consult a doctor in a timely manner. If your blood glucose level increases, you can increase your fluid intake to 2-3 liters before visiting a specialist.
Patients should make scheduled visits to doctors once a year.
As for children, responsibility rightfully lies with the parents. You need to be attentive and vigilant in relation to the health of your child.
Preventive measures
The appearance of insulin shock is caused by the onset of hypoglycemia. To prevent a sharp drop in glucose, you should carefully follow the treatment regimen, as well as take preventive measures.
Basic recommendations:
- monitor the glycemic level - to do this, it is enough to monitor the glucose value before and after meals, as well as unscheduled snacks;
- monitor the urine reaction;
- monitor the condition before and after insulin injections;
- correctly select the dose of insulin prescribed by your doctor;
- do not leave home without sweets;
- do not increase the dosage of hypoglycemic drugs on your own;
- follow the diet and diet prescribed by your doctor;
- check your glycemic index every time before doing physical activity;
- tell people around you about all the complications associated with the disease and teach them the rules of behavior when a hypoglycemic state occurs.
It is important for all people, especially in adulthood, to undergo periodic examinations with a doctor in order to detect diabetes in the early stages of its development. This will help prevent the development of many complications, including hypoglycemia, even in those who are unaware of the progression of the disease.