Hemorrhagic shock is a form of hypovolemic shock, in which severe blood loss leads to disruption of the delivery of oxygen to the body's tissues.
Decreased tissue perfusion leads to a lack of oxygen and nutrients at the cellular level. When cellular oxygen demand cannot be adequately met, the cells and body go into a state of shock. At the multicellular level, defining shock becomes more difficult because not all tissues and organs will experience the same amount of oxygen imbalance characteristic of a given clinical disorder. There are many possible factors for the occurrence of hemorrhagic shock, for example, penetrating abdominal injury, obstetric hemorrhage, gastrointestinal bleeding.
The human body is able to compensate for significant blood loss using various neurological and hormonal mechanisms. Modern advances in trauma treatment allow patients to survive even when these adaptive compensatory mechanisms are overloaded.
Despite this, high mortality from hemorrhagic shock remains one of the global health problems: every year about 1.9 million people die from hemorrhage and the shock state provoked by it. Of these, about 1.5 million deaths were associated with physical injuries. At the same time, the mortality rate among those patients who manage to survive the state of hemorrhagic shock is quite high.
Pathophysiology
The body's responses to acute loss of circulating blood volume have been well studied and described. Teleologically, these reactions represent a systematic diversion of blood circulating in the body from less vital organs. The diverted blood volume can be used to maintain the functioning of the most vital organs. Severe blood loss causes a decrease in cardiac output and pulse pressure. These changes are recognized by baroreceptors in the aortic arch and atrium. As circulating blood volume decreases, nerve reflexes cause increased sympathetic outflow to the heart and other organs. The response is an increase in heart rate, vasoconstriction, and redistribution of blood flow away from some less vital organs such as the skin, gastrointestinal tract, and kidneys.
At the same time, a multisystem hormonal response to acute blood loss occurs. There is direct stimulation of corticotropin-releasing hormone. This ultimately leads to the release of glucocorticoids and beta-endorphins. Vasopressin is released from the posterior pituitary gland, causing water retention in the distal tubules. Renin is released by the juxtamedullary complex in response to a decrease in mean arterial pressure, leading to increased aldosterone levels and ultimately sodium and water resorption.
Hyperglycemia also usually occurs in the setting of acute blood loss. This is due to glucagon and growth hormone-induced increases in gluconeogenesis and glycogenolysis. Circulating catecholamines inhibit insulin release and activity, resulting in increased plasma glucose levels.
In addition to these global changes, many organ-specific reactions occur in the body. The brain has remarkable autoregulation that maintains constant cerebral blood flow over a wide range of systemic mean blood pressure values. The kidneys can tolerate a 90% reduction in total blood flow for short periods of time. With a significant decrease in circulatory volume, intestinal blood flow decreases sharply due to intrarenal vasoconstriction. Early and appropriate resuscitation can prevent damage to individual organs as adaptive mechanisms help protect vital body functions.
Signs of the third stage of hemorrhagic shock
The development of the third stage is accompanied by blood loss, the volume of which exceeds 2 liters. In this case, the patient's condition is characterized as very serious. To save his life, a variety of resuscitation measures must be used. Stage 3 is usually indicated by the presence of the following symptoms:
- the patient is unconscious;
- the skin becomes marbled and pale;
- Blood pressure very often is not determined at all. Sometimes you can measure only the upper indicator, which does not exceed 60 mm. rt. Art.;
- increase in heart rate to 140-160 beats per minute;
- with great skill, the pulse can only be detected in the carotid arteries.
Epidemiology
Hemorrhagic shock is experienced differently depending on the condition of the body and, to some extent, the age of the patient. The very young and very old people are more likely to experience early decompensation after major blood loss.
Children have a smaller total blood volume. Consequently, they risk losing a proportionately larger percentage of blood for an equivalent volume of exsanguination compared with adults. The kidneys of children under 2 years of age are not mature; they have a blunted ability to concentrate solute. Young children cannot maintain circulating blood volume as effectively as older children. In addition, the body surface area of young childhood patients is increased relative to body weight. This promotes rapid heat loss and causes early hypothermia, which can lead to coagulopathy.
Older adults may have certain physiological changes and pathologies that can seriously impair their ability to compensate for acute blood loss. Atherosclerosis and decreased elastin make arterial vessels less elastic, which leads to blunted vascular compensation and decreased vasodilation of the arterial heart. This can provoke the occurrence of angina or heart attack when the myocardial demand for oxygen increases. Older patients are less likely to experience tachycardia in response to decreased blood volume due to decreased beta-adrenergic receptors in the heart and certain other factors. In addition, older patients are often treated with a variety of cardiac medications, which may blunt the normal physiological response to shock. These include beta-adrenergic blockers, nitroglycerin, calcium channel blockers.
The kidneys also undergo age-related atrophy, and in many elderly patients, creatinine clearance is significantly reduced in the presence of near-normal serum creatinine. These changes in the heart, blood vessels and kidneys can lead to early decompensation after blood loss. All these factors, combined with comorbidities, make the treatment of elderly patients with hemorrhagic shock quite challenging.
What determines the severity of the development of shock?
The pathogenesis of the body's compensation for intense blood loss depends on many factors:
- the state of the nervous system, which is involved in the process of regulating vascular tone;
- the presence of pathologies of the cardiovascular system, its ability to work effectively under hypoxic conditions;
- intensity of blood clotting;
- environmental conditions (air saturation with oxygen and others);
- general condition of the body;
- level of immunity.
Clinical picture
No single symptom or sign is sufficient to diagnose hemorrhagic shock. Some patients may report fatigue, general lethargy, or low back pain (ruptured abdominal aortic aneurysm). Others may be transported to a medical facility by ambulance with an unclear diagnosis.
It is very important to get clear information about the type, amount and duration of bleeding. Many decisions regarding diagnostic tests and treatment are based on knowledge of the amount of blood loss that has occurred over a period of time.
If bleeding occurs at home or in the field, it is useful to estimate how much blood was lost.
For gastrointestinal bleeding, it is important to determine whether the blood is leaking through the rectum or orally. All cases of bright red blood leaking from the rectum should be considered severe bleeding until proven otherwise.
Bleeding due to injury is also not always easy to detect. The pleural space, peritoneal cavity, mediastinum, and retroperitoneum are sites that may contain enough blood to cause death by exsanguination.
External bleeding due to trauma can be significant and may be underestimated by medical personnel. Scalp lacerations are notorious for causing large, underappreciated blood loss. Multiple open fractures can easily result in the loss of several units of blood.
Signs of the compensated stage in hemorrhagic shock
The first degree of hemorrhagic shock develops with a loss of about 0.7-1.2 liters of blood. This leads to the inclusion of special adaptive mechanisms of the body. The first thing that occurs is the release of substances such as catecholamines. As a result, with the development of hemorrhagic shock, the following symptoms appear:
- pale skin;
- desolation of veins in the arms;
- increase in the number of heart contractions (up to 100 beats per minute);
- decrease in the volume of urine excreted;
- development of venous hypotension, while arterial hypotension is completely absent or weakly expressed.
Such a clinical picture of hemorrhagic shock can be observed for quite a long time, even if blood loss has completely stopped. If the bleeding continues, there is a rapid deterioration in the person’s condition and the development of the next stage.
Physical examination
Physical examination of patients with hemorrhagic shock is a directed process. Often such an examination is of paramount importance in identifying the source of bleeding and allows assessing the degree of blood loss.
The hallmark clinical indicators of hemorrhagic shock are typically the presence of abnormal physiologic findings such as hypotension, tachycardia, decreased urinary output, and altered mental status. These findings represent secondary effects of circulatory failure rather than a primary etiological event. Due to compensatory mechanisms, the effects of age, and the use of certain medications, some patients in shock have normal blood pressure and pulse. A complete physical examination should be performed with the patient undressed.
The general appearance of a patient in a state of shock can be very dramatic.
The skin may have a pale, ashy color, usually with sweating. The patient may appear embarrassed or agitated.
The pulse becomes rapid at first and then decreases as the pulse pressure decreases. Systolic blood pressure may be within the normal range during compensated shock.
The conjunctiva of the eye is checked for pallor (a sign of chronic anemia). The nose and throat are checked for blood.
The chest is auscultated and percussed to diagnose the presence of hemothorax.
When examining the abdominal cavity, signs of intra-abdominal bleeding are revealed, such as bloating, pain when
palpation. The flanks are examined for ecchymosis, a sign of retroperitoneal bleeding. Ruptured aortic aneurysm is one of the most common conditions that cause hemorrhagic shock in patients. Signs that may be associated with rupture are a palpable pulsating mass in the abdomen, enlargement of the scrotum as a result of retroperitoneal blood tracing, mottling of the lower extremities, and decreased femoral pulses.
The rectum is examined. If blood is detected, the presence of internal or external hemorrhoids should be checked. In rare cases, they are a source of significant bleeding, especially in patients with portal hypertension.
Patients with vaginal bleeding undergo a complete pelvic examination. Pregnancy tests must be taken to rule out ectopic pregnancy.
Trauma patients should be evaluated systematically, applying the principles of primary and secondary evaluation. Victims may have multiple injuries that require attention simultaneously. Hemorrhage can also accompany other types of shock conditions, such as neurogenic shock.
Primary examination is a superficial study that is aimed at identifying signs of life-threatening pathologies for the patient. Initial examination
could go like this:
- To assess the airway, ask the patient's name. If the response is clearly articulated, the airways are open.
- The throat and oral cavity are checked for blood or foreign objects.
- The neck is examined for hematomas or tracheal abnormalities.
- The lungs are auscultated and percussed for signs of pneumothorax or hemothorax.
- Radial and femoral pulses are palpated to determine their strength and frequency.
- A quick inspection of body surfaces is performed to rule out any external sources of bleeding.
- A general neurological examination is performed. Advanced Trauma Life Support
program , a “miniature” neurological examination can classify a patient's levels of conscious functioning according to whether the patient is alert, responsive to voice, responsive to pain, etc.
(determined by the AVPU
). - During the examination, care must be taken to maintain thermoregulation of the patient's body. Blankets and external heating devices can be used for this.
Secondary inspection
- this is a thorough examination of the patient from head to toe, the purpose of which is to identify any traumatic injuries. It can be carried out according to the following algorithm:
- The scalp is inspected for bleeding wounds. Any active bleeding from the scalp should be controlled before further examination.
- The mouth and throat are checked for blood.
- The abdomen is examined and palpated. Distension, pain on palpation and external ecchymosis are signs of intra-abdominal bleeding.
- The pelvis is palpable. Crepitus or instability may be a sign of pelvic fracture, which can lead to life-threatening retroperitoneal hemorrhage.
- Long bone fractures present with localized pain on palpation and crepitus on the bones at the fracture site. All long bone fractures should be reduced and immobilized with splints to prevent continued bleeding. With femur fractures, the risk of major blood loss is very high. Such fractures should be immediately immobilized with a splint.
- Further diagnostic tests are needed to identify intrathoracic, intra-abdominal, or retroperitoneal bleeding.
Causes and manifestations
Disruption of blood microcirculation, which causes hemorrhagic shock, is caused by open or closed trauma. The causes and signs of pathology are always associated with a sudden loss of at least 1 liter of blood. These include the following factors:
- Postoperative period;
- Disintegration of malignant tumors at the final stage of oncology;
- Perforation of a gastric ulcer;
- Ectopic pregnancy;
- Premature placental abruption;
- Excessive postpartum blood loss;
- Frozen pregnancy;
- Trauma to the birth canal during delivery.
The main signs of shock are the following clinical manifestations:
- The heart and lungs work in an accelerated mode: heartbeat and breathing become more frequent;
- Dyspnea;
- Psycho-emotional agitation;
- Pallor of the skin, its moisture;
- Nausea;
- Feeling of dry mouth;
- Weakness and dizziness;
- Desolation of veins under the skin on the arms;
- The appearance of dark circles before the eyes;
- Loss of consciousness accompanied by extremely low blood pressure.
Symptoms differ significantly at different stages of pathology development.
The severity of hemorrhagic shock and the specifics of its manifestations are presented in the table.
Note!
Blood loss of more than 40% is potentially life-threatening for the patient! In this case, his condition requires urgent resuscitation.
You should know that blood loss in children is assessed by other indicators. For a newborn baby to die, it only needs to lose up to 50 ml of blood. In addition, such a condition in children is much more complicated: in their bodies, compensation processes have not yet fully formed.
Differential Diagnoses
- Abdominal trauma, blunt
- Abdominal trauma, penetrating
- Placental abruption
- Acute gastritis
- Acute pancreatitis
- Ampullary carcinoma
- Angiodysplasia of the colon
- Angiosarcoma
- Aortic dissection
- Benign stomach tumors
- Benign neoplasm of the small intestine
- Bile duct tumors
- Biliary Trauma
- Bladder injury
- Chest trauma
- Cancer of the ampulla of Vater
- Cardiac tamponade
- Colon cancer
- Colon polyps
- Distribution shock
- Uterine bleeding
- Ectopic pregnancy
- Esophagitis
- Hemangioblastoma
- Hemolytic anemia
- Hemolitho-uremic syndrome
- Hemophilia
- Haemorrhoids
- Hemothorax
- Hepatic hemangiomas
- Immediate hypersensitivity reactions
- Immune thrombocytopenic purpura (ITP)
- Inflammatory bowel disease
- Intestinal perforation
- Myocardial rupture
- Ovarian cyst rupture
- Pancreatic injury
- Penetrating chest trauma
- Penetrating head injury
- Penetrating neck injury
- Peptic ulcer
- Peritonitis and abdominal sepsis
- Portal hypertension
- Renal artery aneurysm
- Kidney injury
- Septic shock
- Small intestinal diverticulosis
- Splenic rupture
- Toxic shock
- Upper gastrointestinal bleeding
Laboratory research
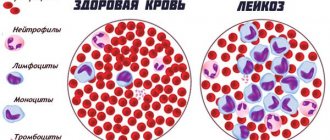
Typically, laboratory tests are not helpful for acute blood loss. This is due to the fact that the values do not differ from normal until the redistribution of interstitial fluid into the blood plasma occurs. This happens within 8-12 hours. Many complications result from the replacement of large amounts of autologous blood with resuscitative fluids.
The values of hemoglobin and hematocrit remain unchanged from the initial level in the first time after acute blood loss. There is no absolute threshold level of hematocrit or hemoglobin level at which a blood transfusion is indicated.
Blood transfusions may be withheld until significant clinical symptoms appear or until the degree of blood loss reaches a level that clearly requires a blood transfusion.
Patients with serious heart disease are at higher risk of myocardial ischemia with anemia. In such cases, blood transfusion should be started when the hemoglobin level falls below 7 mg/dL. Arterial blood gases are perhaps the most important laboratory test in a patient with severe hemorrhagic shock.
In the early stages of shock, acidosis is the best indicator of oxygen imbalance at the tissue level. Blood gas values with a pH of 7.30-7.35 are not normal, but tolerable in acute conditions. Mild acidosis helps to unload oxygen in peripheral tissues and does not affect hemodynamics.
It is believed that a pH below 7.25 may interfere with the action of catecholamines and cause hypotension unresponsive to inotropes. However, current research does not find evidence of this phenomenon. Metabolic acidosis is a sign of disruption of normal oxygen delivery or consumption and requires emergency resuscitation.
Coagulation studies usually give normal results in most patients with severe bleeding. Notable exceptions are patients taking warfarin, low molecular weight heparin, or antiplatelet agents or those with severe liver impairment.
In some cases, tests for primary and secondary hemostasis are required. Prothrombin time (PTT) and activated partial thromboplastin time determine the main problems with secondary hemostasis.
The best test of platelet function is bleeding time. This test is difficult to perform in a patient with acute bleeding.
An alternative is thromboelastography (TEG), which is at least equivalent and possibly superior to bleeding time analysis. This test is an analysis of all components of blood coagulation and is widely used in orthotopic liver transplantation, cardiac surgery and trauma.
Electrolyte studies are usually not helpful in acute situations.
Sodium and chloride levels may increase significantly when large amounts of isotonic sodium chloride are administered. Hyperchloremia can cause nonionic gap acidosis and significantly worsen existing acidosis.
Calcium levels may drop when large volumes of blood are given quickly. Likewise, potassium levels may increase with large blood transfusions.
Creatinine and blood urea nitrogen are usually within normal limits unless pre-existing kidney disease is present. Caution should be exercised when administering iodinated contrast in patients with elevated creatinine levels as it may precipitate nephropathy in addition to chronic renal failure.
For patients with active bleeding, 4 units of packed red blood cells (PRBC) should be prepared, as well as 4 units of fresh frozen plasma (FFP). Platelets may also be used if platelet transfusions are needed.
Possible complications
Hemorrhagic shock is a dangerous condition that, if treated incorrectly or untimely, can lead to the patient’s disability or death. This occurs against the background of the development of disseminated intravascular coagulation syndrome, oxygen paradox, asystole, myocardial ischemia, ventricular fibrillation, etc.
Due to circulatory disorders of the main organs, they begin to function incorrectly. This leads to disruption of basic vital processes, which is the cause of the unfavorable outcome.
Medical imaging
Imaging studies are aimed at identifying the source of bleeding. For many types of severe hemorrhage, therapeutic interventions such as exploratory laparotomy will not allow comprehensive diagnostic testing.
Chest X-rays
A chest x-ray can diagnose hemothorax, which appears as widespread opacity in one or both lung fields.
Hemothoraxes large enough to cause shock usually present as complete disappearance of the pleural space.
Abdominal radiographs
Abdominal radiographs are rarely helpful. Hemoperitoneum (intra-abdominal bleeding) is usually not visible on plain film.
Sometimes the radiograph has a ground glass appearance, which indicates a large amount of intraperitoneal fluid, but this sign is not reliable.
CT scan
Computed tomography (CT) is sensitive and specific for the diagnosis of intrathoracic, intra-abdominal, and retroperitoneal hemorrhage. CT is excellent for diagnosing bleeding in these cavities.
Ultrasound is rapidly replacing computed tomography as a diagnostic test for detecting hemorrhages in major body cavities. However, the ability of this test to examine the retroperitoneum is limited. The study of retroperitoneal cavities remains the subject of computed tomography.
Esophagogastroduodenoscopy
Esophagogastroduodenoscopy (EGD) is the main test to detect acute bleeding from the upper gastrointestinal tract. This test allows you to make an accurate diagnosis.
Before the procedure, the stomach should be flushed with a large gastric tube to remove as many clots as possible.
Aortoenterological fistulas are diagnosed quite rarely and are usually caused by erosion of the aortic aneurysm into the duodenum. EGD can diagnose this problem, but the false negative rate in these cases is very high.
Colonoscopy
Colonoscopy is used to diagnose acute lower gastrointestinal bleeding.
This test is considered difficult to perform in the acute setting and may not correctly identify the source of blood loss in cases of severe bleeding.
Although there is some experience with therapeutic interventions such as cauterization for acute arteriovenous malformation hemorrhage, these methods are not widely used.
Ultrasound
Ultrasound is a useful method for diagnosing intraperitoneal hemorrhage in patients with traumatic injuries.
Focused ultrasound testing of trauma patients (FAST) has effectively replaced diagnostic peritoneal lavage as the test of choice for identifying intraperitoneal fluid in trauma patients.
The FAST examination includes 4 anatomical images of the pericardium, abdomen and pelvis, the examination of which allows the identification of free intra-abdominal fluid.
Bedside ultrasound can be performed by radiologists, surgeons, and emergency medicine physicians who have specialized training and certification.
Angiography
Angiography is extremely useful for diagnosing acute bleeding of various origins.
For low gastrointestinal bleeding, angiography is one of the best tests to localize the source of bleeding. Angiography can usually detect bleeding that is at least 1-2 ml/min. Selective angiograms of the celiac, superior mesenteric, and inferior mesenteric arteries are performed to identify sites of bleeding. The best time to conduct an examination is during active bleeding. Once the source of blood loss is determined, embolotherapy can be used as a means to stop bleeding. If embolotherapy is not used, identifying the site of bleeding will allow for a more limited bowel resection if surgery is necessary.
Angiography can be used to diagnose and treat severe bleeding from pelvic fractures. Although most bleeding due to severe pelvic fractures is of venous origin, significant arterial bleeding is occasionally diagnosed and is effectively treated with embolization.
Severe liver injuries pose a major challenge to the trauma surgeon due to the large blood loss and difficulty in quickly obtaining surgical control. Many serious liver injuries are now diagnosed and treated using angiographic embolization. Angiography is increasingly considered a first-line intervention (before laparotomy) for severe liver injury in centers that are equipped to perform rapid angiography and angiographic intervention. Similar techniques can be used to diagnose and treat injuries to other internal organs, such as the spleen and kidneys.
Angiography can be used in the diagnosis of massive hemoptysis of unknown etiology. Selective angiography of the bronchial arteries in combination with a selective pulmonary angiogram through separate venous catheterization helps localize the bleeding.
The role of angiography in upper GI bleeding is more limited. Hemobilia is a rare cause of bleeding from the upper gastrointestinal tract. If blood is observed emanating from the ampulla of Water, angiography should be performed to localize and control the source of the bleeding.
Nuclear scan
Diagnostic nuclear medicine methods are used to study the location of gastrointestinal bleeding.
Tagged red blood cell scanning helps differentiate between upper and lower gastrointestinal bleeding.
The test requires a significant amount of time to complete, but is very sensitive and can detect bleeding as low as 0.5 ml/min.
Procedures
Diagnostic peritoneal lavage
is a bedside procedure in which a small midline laparotomy is made and a catheter is inserted directly into the abdominal cavity. Percutaneous administration methods are available but carry an increased risk of damage to underlying tissue.
The purpose of diagnostic peritoneal lavage is to detect significant intra-abdominal bleeding or damage to hollow organs.
If more than 5 ml of blood is aspirated, the test result is considered positive and laparotomy is usually indicated.
If blood is not aspirated, 1000 mL of warm lactated Ringer's solution is injected into the peritoneal cavity and then allowed to drain into an IV bag. The contents of the package are tested in the laboratory. A red blood cell count greater than 10,000 per microliter is considered a minimally positive test result.
Other conditions that make the test result positive include the following: White blood cell count greater than 500/µL; High levels of amylase, lipase, or bilirubin; Presence of particulate matter, which may be from an intraluminal source.
Central venous catheter
A central venous catheter is considered an addition to large-bore peripheral catheters (16 or 14).
The capacity of the catheter is inversely proportional to the length and directly proportional to the diameter. Thus, long, small-caliber catheters, such as a standard triple-lumen catheter, will provide significantly less volume than short, large-caliber catheters, such as a peripheral venous catheter.
Chest drainage
Initial treatment of hemothorax involves insertion of a large bore chest catheter for drainage or open thoracotomy. In most patients with hemothorax, thoracotomy alone is sufficient.
Surgical exploration with open thoracotomy is mandatory in the presence of persistent bleeding. The latter is diagnosed if there is more than 1500 ml of blood in the initial drainage of the chest catheter or if there is more than 200 ml/h of blood drainage for 2-4 hours.
Treatment
The main treatment for hemorrhagic shock is to stop bleeding as quickly as possible and replace lost fluids.
In controlled hemorrhagic shock, when the source of bleeding has been blocked, fluid replacement is aimed at normalizing hemodynamic parameters. In cases of uncontrolled hemorrhagic shock, when bleeding has temporarily stopped due to hypotension, vasoconstriction and clot formation, fluid treatment is aimed at restoring the radial pulse.
When the evacuation time is less than 1 hour (usually urban trauma), emergency evacuation to a surgical facility is carried out after ensuring respiratory function. In this case, you should not waste precious time inserting an intravenous catheter.
When the expected evacuation time exceeds 1 hour, an intravenous catheter is inserted and fluids are administered prior to evacuation. Resuscitation should be performed before or simultaneously with any diagnostic testing.
Crystalloid is the main fluid used for resuscitation. At the first signs of hemorrhagic shock, 2 liters of isotonic sodium chloride solution or lactated Ringer's solution should be immediately administered into the victim's body. Fluid administration should continue until the patient's hemodynamics are stabilized. Since crystalloids quickly flow out of the vascular space, each liter of fluid increases blood volume by 20-30%; therefore, 3 L of fluid must be administered to increase intravascular volume by 1 L.
Colloids restore blood volume in a 1:1 ratio. Currently available colloids include human albumin or hypertonic saline solutions.
The combination of dextran and hypertonic saline may be useful in situations where infusion of large volumes of fluid may pose a risk, such as in older adults with cardiac problems.
If possible, blood and crystalloid infusions should be delivered via a fluid warmer.
Comprehensive diagnostics
Diagnosis of HS is aimed at determining the volume of blood loss. With the help of research, the stage and severity of shock is established. Primary diagnosis is carried out to clarify the volume of lost blood for infusion therapy. The doctor examines the skin.
The following indicators, characteristic of any degree of hemorrhagic shock, are monitored:
- pressure;
- heart and breathing rhythm;
- diuresis;
- shock index;
- hemoglobin.
Additionally, a biochemical blood test is performed. The treatment regimen is carried out after determining the amount of blood loss. The following methods are used for this:
- Indirect. Visual assessment of the patient.
- Direct. Diagnostics is carried out by performing certain actions.
The main indicator of indirect methods is the shock index. It is used in the post-hemorrhagic period, at the pre-hospital stage. In a hospital, doctors rely on the results of laboratory tests.
Surgical intervention
Acute, life-threatening bleeding in the abdominal or chest cavity is an indication for surgery. Retroperitoneal bleeding is difficult to control surgically; as a rule, it is treated without surgery.
Severe bleeding from the upper gastrointestinal tract is most often treated with esophagogastroduodenoscopy (EGD), with the option of cauterizing the source of bleeding and administering epinephrine. Failure of endoscopic treatment is usually an indication for surgery.
Severe vaginal bleeding requires early intervention by a gynecologist. Ectopic pregnancies are treated with immediate surgery. Placental abruption is an emergency and requires an immediate cesarean section.