Acute cardiovascular failure is a life-threatening condition. According to the mechanism of development, it is divided into right and left ventricular AHF. Both of these conditions are often fatal. To save a person, an emergency physician must immediately begin resuscitation measures.
The most common type is left ventricular heart failure. It usually follows myocardial infarction, severe arrhythmias and other dangerous conditions. Varieties of AHF include acute cardiogenic shock. It is caused by severe lesions for the body, in which the heart cannot pump blood normally.
The concept of cardiogenic shock
Emergency care for cardiogenic shock is necessary in the first minutes of its development. It should be remembered that this complication will not go away on its own. And in the absence of urgent treatment it will lead to death. Cardiogenic shock is a syndrome in which there is a decrease in cardiac output. Despite the compensatory increase in vascular resistance, the body cannot cope with this complication without the help of doctors.
Its main manifestations include a decrease in blood and pulse pressure, diuresis, and loss of consciousness. If help is not provided in time, death from cardiogenic shock occurs within a few hours after the onset of the disease. This condition does not occur on its own. It is always preceded by acute pathologies of the cardiovascular system.
Symptoms that appear
A critical situation is manifested by sharp acute pain in the area of the heart. The first signs are similar to a heart attack. The pain syndrome is felt as a squeezing pain, it spreads to the chest area, left shoulder blade, arm, jaw. Similar symptoms extend only to the left side of the body, from the side of the heart. Over time, the pain increases.
Heartache
A person’s blood pressure drops (below 80-90), the pulse is frequent but weak. The body turns pale, cold sweat appears, dizziness and weakness throughout the body intensify. Coma may develop. The dangerous condition develops gradually.
Breathing becomes difficult, becomes infrequent and shallow. This occurs due to insufficient blood flow to the lungs. The body spends all its energy on supporting vital systems, minimizing costs for other organs, putting a person into a kind of coma.
Loss of the ability to breathe on your own often occurs. The patient develops disturbing thoughts, fear, and panic increases. The subsequent development of pulmonary edema is characterized by the release of pink or white foam from the mouth. The respiratory rate drops to 10-15 respiratory movements per minute.
Characteristic signs of deterioration:
- Swollen veins in the neck area;
- Decreased temperature, cold hands and feet;
- Blueness of the nose, lips, fingers;
- Lethargy, loss of coordination;
- Increasing panic, feelings of fear;
- Loss of consciousness;
- Barely noticeable breathing;
- Pain in the pectoral muscle;
- The pressure is jumping.
What causes lead to cardiogenic shock?
The causes of cardiac shock include various cardiac and vascular diseases. The most common etiological factor is myocardial infarction. In this case, cardiogenic shock develops only with massive tissue necrosis and the absence of emergency care. Also common causes of its occurrence include life-threatening arrhythmias. They can bother a person for many years. But with their exacerbation and decompensation, these conditions are complicated by shock.
In some cases, a factor in the development of acute heart failure is considered to be a violation of vascular tone. This happens with massive bleeding, pain syndrome, acute renal failure. It must be remembered that cardiogenic shock is not an independent disease, but a complication of the underlying pathology. Therefore, doctors need to do everything to prevent its development.
Treatment of traumatic shock
For the treatment of traumatic shock in the hospital, there are 5 areas:
- Therapy for non-threatening injuries. The first life-sustaining measures are, as a rule, temporary in nature (transport immobilization, application of a tourniquet and bandage) and are carried out directly at the scene of the incident.
- Interruption of impulses (pain therapy). Achieved by combining three methods: local blockade;
- immobilization;
- use of antipsychotics and analgesics.
Cardiogenic shock: classification of the disease
Depending on the cause and pathogenesis, several forms of cardiogenic shock are distinguished. Each of them has its own development mechanism. However, all variants result in the same symptoms. Regardless of the cause of its occurrence, emergency care for cardiogenic shock is necessary in any case. Since this condition is always equally dangerous. The following types of this complication are distinguished:
- True cardiogenic shock. It develops when heart tissue is damaged. In most cases, this form is caused by transmural necrosis of the myocardium.
- Arrhythmic shock. Its causes include ventricular fibrillation and flutter, extrasystole, and severe bradycardia. In addition to arrhythmias, cardiac conduction disturbances can lead to shock.
- Reflex cardiogenic shock. With this option, cardiac dysfunction does not precede the complication. It usually develops with massive blood loss and renal failure.
- Areactive shock. Is the most dangerous option. It is placed in a separate group, since it almost always leads to death and cannot be treated.
Causes of shock
All viral microorganisms produce toxic substances that poison the body. However, only some of them lead to shock. Most often, cases of ITS are recorded when the body is damaged by microorganisms of a protein nature. This pattern is due to 2 reasons:
- A larger surface area of the protein contains more antigens, molecules that trigger a response from the immune system;
- The protein contains several enzyme centers, each of which has a pathogenic effect on the body.
For this reason, ITS condition is most often provoked by staphylococci and streptococci. Staphylococci synthesize proteins that bind immunoglobulins and destroy collagen. Streptococci destroy blood cells, completely dissolving them.
However, it should be noted that the infectious process leading to shock also develops in other diseases. Let us list the pathological factors that cause ITS:
- Pneumonia;
- Sinusitis;
- Meningitis;
- Acute otitis media;
- Opening an abscess after injury;
- Peritonitis;
- Septic abortion;
- Tonsillitis;
- Endocarditis.
The presence of these pathologies is not a prerequisite for the development of a shock state. For pathology to occur, one of the following factors must be present:
- Great pathogenic potential of the pathogen;
- Weak immune system;
- Failure to contact medical personnel in a timely manner;
- A large amount of infectious dosage of a pathogenic agent;
- Incorrectly chosen treatment tactics.
Infections should be separated into a separate group, at the first manifestations of which toxic shock (especially in children) occurs most often. This is meningococcal disease. It is dangerous for babies at an early age. Thus, one of its subtypes (meningococcemia) causes disturbances in hemodynamics and the functioning of the adrenal glands. In this case, the symptoms and treatment will differ from the usual regimens.
It should be noted the conditions, during the development of which there is also a slight risk of developing ITS:
- Infectious complication after surgery;
- Open type injuries (wounds and burns);
- HIV;
- Postpartum sepsis;
- Intestinal infections;
- Dermatitis caused by an infectious process;
- Intravenous drug administration.
This is interesting!
Even women who regularly use tampons are susceptible to ITS. The risk is minimal, but such cases have been recorded.
True cardiogenic shock: mechanism of development
True cardiac shock is the most common. It occurs if a large part of the myocardium is affected (50% or more). In this case, necrosis spreads not only throughout the entire thickness of the muscle, but also occupies a large area. In addition to a heart attack, other illnesses can lead to true shock. Among them: septic endocarditis, severe heart defects, decompensated myodystrophies, etc. Acute hyperthyroidism and some genetic pathologies also lead to severe cardiac disorders.
As a result of necrosis of cardiac tissue, contractility is significantly reduced. Therefore, the organ cannot work at full capacity and supply blood vessels. The minute volume also decreases. This results in an increase in vascular resistance. Despite this, the heart still cannot cope with its job. The result is impaired blood supply to all organs and tissues.
Causes of traumatic shock
A traumatic condition occurs as a result of severe damage to the human body:
- extensive burns;
- gunshot wounds;
- traumatic brain injuries (falls from heights, accidents);
- severe blood loss;
- surgical intervention.
Other causes of traumatic shock:
- intoxication;
- overheating or hypothermia;
- DIC syndrome;
- starvation;
- vasospasm;
- allergy to insect bites;
- overwork.
Pathogenesis of arrhythmic cardiogenic shock
This form of the disease is based on disturbances in the conduction and rhythm of the heart. They can occur either spontaneously (as a result of myocardial infarction) or develop gradually. Most often, arrhythmias bother the patient for many years. The same applies to conduction disorders. However, life-threatening conditions develop over a short period. We are talking about hours and even minutes. Most often, cardiogenic shock is caused by ventricular rhythm disturbances. Among them: tachycardia, turning into fibrillation, and flutter. In addition, frequent group extrasystoles can lead to these processes.
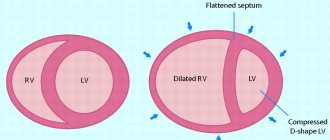
Another condition that can lead to shock is sinus bradycardia. A decrease in heart rate is usually characterized by conduction disturbances. Less commonly, atrial fibrillation and flutter lead to cardiogenic shock. As a result of pathological contractions and ectopic foci in the myocardium (extrasystoles), the heart cannot perform its function. Therefore, there is a decrease in stroke and minute volume, a drop in pulse pressure, and blood pressure. With this option, the emergency doctor must first stop the arrhythmia by performing defibrillation or artificial cardiac massage.
Symptoms
The clinical picture of cardiogenic shock is characterized by the following manifestations:
- the skin turns pale, the nasolabial triangle acquires a color characteristic of circulatory disorders - gray or bluish;
- cold extremities, increased sweating;
- the heartbeat is frequent (over 100 beats per minute), while the pulse is weak, thread-like;
- Blood pressure drops to critical levels - systolic below 90 mm. rt. column, diastolic below 30 mm. rt. column;
- drop in pulse pressure to 20-25 mm. rt. pillar and below;
- decreased body temperature (below 35.5 degrees);
- wheezing is heard when breathing, the nature of breathing is superficial;
- a decrease in urine output to 20 ml per hour (oliguria) or complete cessation of urination (anuria);
- possible cough with foamy sputum;
- pain is concentrated in the chest area, spreading to the upper shoulder girdle and arms;
- complete loss of consciousness, coma, lethargy, sometimes preceded by a short period of excitement.
What is reflex shock?
This form of shock develops due to reasons not initially related to damage to the heart muscle. The trigger for such a complication can be severe pain or bleeding. However, these symptoms are rarely related to the heart. Typically, such shock is diagnosed after an accident or acute renal failure.
This option has the most favorable prognosis. Emergency care for cardiogenic shock of a reflex nature should be aimed at eliminating its cause - pain, as well as stopping bleeding. As a result of these factors, the regulation of vascular tone is disrupted. Because of this, blood stagnates in the veins and arteries, and fluid leaks into the interstitial space, forming edema. All this leads to a decrease in venous flow to the heart. Further, the mechanism is the same as for other forms.
Causes and pathogenesis of areactive shock
Areactive cardiogenic shock occurs if the entire myocardium is affected. This occurs with repeated heart attacks. Cardiac tamponade may also be the cause. In this case, fluid appears in the pericardium, which compresses the organ, preventing it from contracting. In some cases, tamponade can lead to heart rupture. This condition leads to death. Unfortunately, it is not possible to help the patient in this case. The mechanism of shock development is associated with a complete cessation of cardiac function, unlike other forms in which cardiac output decreases. The mortality rate from this complication is close to 100%.
Causes
The causes of cardiogenic shock are:
- Myocardial infarction. This is the most common cause of acute heart failure. During a heart attack, an area of tissue necrosis forms in the thickness of the heart muscle, as a result of which the contractility and pumping function of the heart are impaired. Shock most often occurs against the background of extensive shock, when the entire thickness of the muscle layer is affected. This occurs when more than 40-50% of the functional tissue dies. A heart attack develops with atherosclerosis, thrombosis of the coronary arteries, thromboembolism and arterial hypertension.
- Acute poisoning. Various poisons that enter the body accidentally or intentionally can disrupt the functioning of the heart. The greatest dangers come from organophosphorus compounds, pesticides, insecticides (products used to kill insects) and some cardiotoxic drugs (cardiac glycosides).
- . With this pathology, a large vessel is blocked by a thrombus. This leads to acute heart failure of the right ventricular type.
- Hemorrhage inside the heart. Possibly due to a ruptured aneurysm.
- Cardiac tamponade. It most often occurs when blood accumulates in the pericardial sac, pericarditis, severe injuries, etc.
- Severe forms of cardiac arrhythmia.
- Hypertrophic cardiomyopathy.
- Damage to the papillary muscles.
- Ventricular septal defect.
- Heartbreak.
- Bacterial endocarditis.
- Valve insufficiency.
- Pneumothorax.
- Electrical injury.
Predisposing factors are lipid metabolism disorders, obesity, stress, diabetes mellitus and frequent.
Symptoms of cardiogenic shock
The clinical picture is the same, regardless of what caused the cardiogenic shock. Symptoms of the complication are as follows: a drop in blood and pulse pressure, tachycardia, oliguria (decreased diuresis). Depending on the value of blood pressure and clinical data, there are 3 degrees of severity. When examining the patient, other signs of cardiogenic shock can be identified. These include:
- Cold and clammy sweat.
- Fear of death or lack of consciousness.
- Cyanosis is a bluish appearance of the skin.
- The patient's facial features may be sharpened, and his facial expressions may be pained.
- In severe cases, the skin color takes on a gray tint.
How to diagnose shock?
Diagnosis of cardiogenic shock is usually based on clinical data and questioning of the patient's relatives. Since action must be taken immediately, doctors evaluate blood pressure, skin condition, pupil reaction, heart rate and respiratory rate. If the patient shows signs of shock, emergency care is provided immediately.
If medical personnel are available, the medical history is ascertained. The doctor asks: did the patient suffer from arrhythmia, angina pectoris, or perhaps have suffered a myocardial infarction before? If the complication develops at home or on the street, then the diagnosis of shock by emergency doctors ends there. When a patient is kept in an intensive care unit, in addition, pulse pressure, vascular resistance, and diuresis are measured. The gas composition of the blood is also examined.
Diagnostics
Differential diagnosis of cardiogenic shock caused by acute myocardial infarction often has to be carried out with other conditions that have a similar clinical picture. These are massive pulmonary embolism, dissecting aortic aneurysm, acute cardiac tamponade, acute internal bleeding, acute cerebrovascular accident, diabetic acidosis, overdose of antihypertensive drugs, acute adrenal insufficiency (mainly caused by hemorrhage into the adrenal cortex in patients receiving anticoagulants), acute pancreatitis. Considering the complexity of differential diagnosis of these conditions, even in specialized hospitals, one should not strive for its mandatory implementation at the prehospital stage.
Cardiogenic shock: emergency care, algorithm of actions
It is worth remembering that the patient’s life depends on how quickly and efficiently the assistance is provided. If there are signs of such a complication, doctors begin to take action immediately. If you do everything necessary in time, you can overcome cardiogenic shock. Emergency assistance - the algorithm of actions is as follows:
- Place the patient in a horizontal position with the leg end raised. In addition, it is necessary to provide access to air (unbutton clothes, open a window).
- Oxygen supply. It can be performed through a special mask or nasal catheter.
- Anesthesia. In case of myocardial infarction and reflex shock, narcotic drugs are used for this. The most commonly used medication is Morphine. It is diluted in saline and administered intravenously slowly.
- Restoration of blood volume and blood flow. To do this, administer the “Reopoliglucin” solution.
- If there is no effect, it is necessary to increase blood pressure using the drug "Atropine" 0.1%. Administer in an amount of 0.5-1 ml.
In addition, it is necessary to eliminate the cause of shock. In case of myocardial infarction, thrombolytic and antiplatelet therapy is carried out (drugs Alteplase, Clopidogrel, Aspirin). Heparin solution is also used to thin the blood. For ventricular arrhythmias, the drug Lidocaine is administered. In some cases, defibrillation is necessary.
Actions of others
It is very important to seek medical help at the first signs of a heart attack and admit the patient to the intensive care unit. It is possible that in the case of myocardial infarction or cardiogenic shock, the symptoms will not be correctly interpreted by the patient's family members
However, the cost of an error here is minimal, since help for these conditions is provided according to a similar algorithm.
It is important to remember that the appearance of pressing and burning pain in the heart with shortness of breath, acute respiratory distress and loss of consciousness, regardless of whether others understand the cause of these symptoms, are reasons to seek emergency medical help. It is impossible to help the patient independently without narcotic pain relief, cardiotonic drugs, oxygen therapy with antifoam agents, nitrates and osmotic diuretics
Without treatment, he will certainly die in any variant of the course of CABG, while therapy according to the standard algorithm in the conditions of emergency medical care and intensive care unit gives the patient a good chance of survival.