What is the aorta
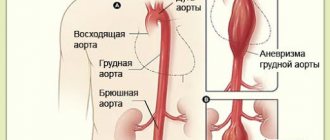
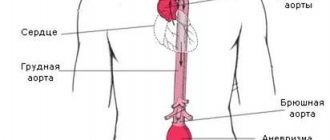
The aorta is the largest vessel in the human body, which carries blood from the heart to the organs and limbs. The upper section of the aorta runs inside the chest, this section is called the thoracic aorta . The lower part is in the abdominal cavity and is called the abdominal aorta . It delivers blood to the lower part of the body. In the lower abdomen, the abdominal aorta divides into two large vessels - the iliac arteries , which carry blood to the lower extremities.
The aortic wall consists of three layers: internal (intima), middle (media), external (adventitia).
Abdominal aortic aneurysm
Abdominal aortic aneurysm is a chronic degenerative disease with life-threatening complications. An abdominal aortic aneurysm is defined as an increase in its diameter by more than 50% compared to the norm or a local bulging of its wall. Under the pressure of blood flowing through this vessel, the dilatation or bulging of the aorta may progress. The diameter of a normal aorta in the abdominal region is approximately 2 cm. However, at the site of an aneurysm, the aorta can be dilated to 7 cm or more.
Why is an aortic aneurysm dangerous?
An aortic aneurysm poses a major health risk as it can rupture. A ruptured aneurysm can cause massive internal bleeding, which in turn leads to shock or death.
An abdominal aortic aneurysm can cause other serious health problems. Blood clots (thrombi) often form in the aneurysm sac or parts of the aneurysm tear off, which move with the blood flow along the branches of the aorta to the internal organs and limbs. If one of the blood vessels becomes blocked, it can cause severe pain and lead to organ death or loss of a lower limb. Fortunately, if an aortic aneurysm is diagnosed early, treatment can be timely, safe and effective.
What is atherosclerotic cardiosclerosis?
Atherosclerotic (not to be confused with post-infarction) cardiosclerosis is a kind of mythical diagnosis inherited from previous generations in our polyclinic network. Atherosclerotic cardiosclerosis is diagnosed in all patients who present vague complaints from the heart and/or have some vague changes on the ECG, as well as in all those over 55-60 years old.
As for the medical part, in Russia, Ukraine and other neighboring countries there is no such diagnosis in the official classifications.
In some cases, this diagnosis is a stigma on the life of a relatively healthy person, and sometimes it is a step towards obtaining the social status of a disabled person, even group III, desired by many patients.
To be fair, it must be said that in the West, ICD-10 is the international classification of diseases. And in one of the headings, something similar is actually mentioned under code I 25.1, but not at all what our therapists mean.
I 25.1 - atherosclerotic heart disease is atherosclerosis of the coronary arteries, detected by coronary angiography, which can be asymptomatic and has nothing to do with cardiosclerosis.
In the same ICD there is such a heading as 125.5 ischemic cardiomyopathy, it is more suitable under the concept of atherosclerotic cardiosclerosis. But this cardiomyopathy occurs against the background of long-term chronic ischemic heart disease, usually angina, and the criteria for diagnosing “ischemic cardiomyopathy” are not age over 60, not “some” complaints that cannot be attributed to anything, and not “penny” changes in ECG.
In conclusion, I would like to appeal to patients not to terrorize clinic doctors on this issue. They did not come up with the diagnosis “atherosclerotic cardiosclerosis”; this is a kind of tradition that only the Ministry of Health can change.
Types of aortic aneurysms
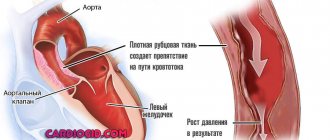
There are “true” and “false” aortic aneurysms. A true aneurysm develops due to the gradual weakening of all layers of the aortic wall. A false aneurysm is usually the result of trauma. It is formed from the connective tissue surrounding the aorta. The cavity of the false aneurysm is filled with blood through a crack in the aortic wall. The aortic walls themselves do not participate in the formation of an aneurysm.
Depending on the form there are:
- saccular aneurysm - expansion of the aortic cavity on only one side;
- spindle-shaped (fusiform) aneurysm - expansion of the aneurysm cavity on all sides;
- mixed aneurysm - a combination of saccular and fusiform forms.
Aneurysm of the ascending aorta
(Fig. 1-3). Operative access - longitudinal sternotomy. After opening the pericardium and connecting the heart-lung machine, the aneurysm of the ascending aorta is isolated and a transverse clamp is applied to the aorta proximal to the origin of the branches of the brachycephalic trunk.
- Surgery for diffuse aneurysm of the ascending aorta with artificial circulation and coronary perfusion
- rice. 1
— aneurysm is highlighted (top left — cut line)
- rice. 2
— distal anastomosis of the prosthesis and the aorta is completed, coronary perfusion continues
- rice. 3
- proximal anastomosis
During artificial circulation with gradual cooling of the blood to a temperature of 28-30°, the aneurysm is opened with a transverse incision, and special cannulas are inserted into the mouths of both coronary arteries for coronary perfusion. After this, the aneurysm itself is resected. The aortic defect is replaced with an allograft. Due to the fact that the operation is performed under artificial circulation (heparinized blood), the graft must be impermeable to blood.
First, a distal anastomosis of the aorta with the prosthesis is performed, and then a proximal one. At this stage of the operation, if necessary, aortic valve insufficiency can be corrected. After suturing, the patient is warmed to normal temperature and artificial circulation is continued until the left ventricle is able to maintain blood circulation. Before suturing the surgical wound, the right mediastinal pleura is widely opened and drains are installed in the right pleural cavity and pericardium.
In some cases, an aneurysm of the ascending aorta is saccular with a relatively narrow neck. The operation in such cases does not require artificial circulation. Apply a parietal clamp to the aortic wall at the base of the aneurysm neck (Fig. 4-6). The latter is cut off, and the neck of the aneurysm is sutured with a series of continuous mattress sutures with additional application of 8-shaped sutures along the free edge.
- Surgery for saccular aneurysm of the ascending aorta
- rice. 4 - an aneurysm with a relatively narrow neck is highlighted (top left - cut line)
- rice. 5 - compression and excision of the aneurysmal sac
- rice. 6 - suturing the neck of the sac (top left - a cuff made of synthetic fabric is placed on the aorta)
In some cases, instead of artificial blood circulation, a temporary bypass shunt made of a plastic prosthesis can be used.
Aneurysm of the aortic arch (Fig. 7, 1). The operation requires wide access and is usually performed from a left-sided thoracotomy with an oblique intersection of the sternum and transition to the right side in the II-III intercostal space.
Rice. 7. Surgery for aortic arch aneurysm without artificial circulation with a temporary shunt. Prosthetics of the aortic arch and its branches (1 - aortic arch aneurysm, 2-4 - stages of the operation)
Against the background of artificial circulation, a bypass shunt is applied between the descending aorta and carotid arteries using a plastic bifurcation prosthesis (Fig. 7, 2).
Perfusion of the vessels of the head is carried out retrogradely from the descending aorta. In rare cases, it is possible to perfuse the right carotid artery retrogradely through the right subclavian artery. Next, the aneurysm is resected. The aortic arch defect is replaced with a prosthesis. Anastomosis of the branches of the aortic arch with this graft can be performed either separately for each vessel (with the “transformation” of the left common carotid and subclavian arteries into a second innominate artery), or using a common base for the mouths of all three brachycephalic vessels (Fig. 7 , 3). After implantation of the branches of the brachycephalic trunk into the prosthesis, first distal and then proximal anastomoses of the aorta with the prosthesis are performed, and the temporary aorto-carotid bypass graft is removed (Fig. 7, 4).
The patient is on artificial circulation all this time.
Causes and risk factors for the development of abdominal aortic aneurysm
The causes of the development of abdominal aortic aneurysms are very diverse. The most common cause of aneurysm development is atherosclerosis. Atherosclerotic aneurysms account for 96% of the total number of all aneurysms. In addition, the disease can be either congenital (fibromuscular dysplasia, Erdheim's cystic medianecrosis, Marfan syndrome, etc.) or acquired (inflammatory and non-inflammatory). Inflammation of the aorta occurs when various microorganisms invade (syphilis, tuberculosis, salmonellosis, etc.) or as a result of an allergic-inflammatory process (nonspecific aortoarteritis). Non-inflammatory aneurysms most often develop with atherosclerotic lesions of the aorta. Less commonly, they are the result of injury to its wall.
Risk factors for developing an aneurysm
- Arterial hypertension;
- Smoking;
- The presence of aneurysms in other family members. Which indicates the role of hereditary factors in the development of this disease;
- Gender: men over 60 years of age (abdominal aortic aneurysms occur less frequently in women).
Symptoms and signs of abdominal aortic aneurysm
In most patients, abdominal aortic aneurysms occur without any symptoms and are an incidental finding during examinations and operations for other reasons.
When signs of an aneurysm develop, the patient experiences one or more of the following symptoms:
- A feeling of pulsation in the abdomen, similar to a heartbeat, an unpleasant feeling of heaviness or fullness.
- Dull, aching pain in the abdomen, in the navel area, usually on the left.
Indirect signs of abdominal aortic aneurysm are important :
- Abdominal syndrome. Manifested by the appearance of belching, vomiting, unstable stool or constipation, lack of appetite and weight loss;
- Ischioradic syndrome. Manifested by lower back pain, sensory disturbances and movement disorders in the lower extremities;
- Syndrome of chronic ischemia of the lower extremities. Manifests itself in the appearance of pain in the muscles of the lower extremities when walking, sometimes at rest, coldness of the skin of the lower extremities;
- Urological syndrome. It manifests itself as pain and heaviness in the lower back, difficulty urinating, and the appearance of blood in the urine.
Harbingers of rupture may be increased abdominal pain.
When an aneurysm ruptures, the patient suddenly feels an increase or appearance of abdominal pain, sometimes “radiating” to the lower back, groin area and perineum, as well as severe weakness and dizziness. These are symptoms of massive internal bleeding. The development of such a situation is life-threatening! The patient needs emergency medical care!
What are the symptoms of the disease
Intestinal ischemia occurs when blood vessels become blocked or narrowed. Under these conditions, cells cannot receive the required amount of blood. Ischemia can develop in both the large and small intestines.
- Causes of ischemia
- Symptoms of the disease
- Diagnosis of the disease
- Treatment methods
- Possible consequences
- Preventive measures
Causes of ischemia
Many reasons depend on the form in which the disease occurs.
- Occlusive ischemia. It often develops with thrombosis of certain veins and their tributaries, embolism of the mesenteric arteries and thrombosis. Ischemia often occurs in people who have undergone heart valve replacement, as well as in those who have heart defects and atrial fibrillation. Thrombosis itself can occur due to decreased cardiac output and atherosclerosis. Thrombosis of the mesenteric veins is rare and occurs with peritonitis, increased blood clotting, portal hypertension and inflammatory processes occurring in the abdominal cavity.
- Nonocclusive ischemia. This form occurs in half of patients. The exact cause is unknown, but it is believed that it may develop due to arrhythmia, hypotension, the use of certain medications, heart failure and dehydration.
Mesenteric artery embolism
Most often, elderly people suffer from ischemia occurring in the intestines. In addition to the listed forms, such ischemia can be:
- acute, when symptoms appear suddenly;
- chronic, when symptoms occur periodically and gradually.
Acute mesenteric ischemia also has causes similar to those already listed. The lumen of the artery suddenly narrows due to a blood clot. This usually happens with atrial fibrillation. Let us recall that atrial fibrillation is a heart rhythm disorder that occurs when the bicuspid heart valve narrows.
This arrhythmia causes the heart muscle to contract very quickly, causing blood clots to appear in the heart cavity. They enter the aorta, and from there into the intestinal arteries. A sudden blockage affecting these arteries causes the intestinal walls to quickly die, leading to dangerous complications.
Acute mesenteric ischemia
DETAILS: Cardiac ischemia in children
The chronic form occurs due to atherosclerosis. After eating, intestinal peristalsis increases, however, due to the fact that blood flows to the intestines in reduced quantities, pain occurs, which is the main manifestation of ischemia.
At the onset of the disease, acute pain usually appears in the abdomen, especially in the right upper quadrant of the abdomen and the umbilical region. Ischemia of the intestinal wall also leads to violent peristalsis and the urge to defecate. During the initial period, other symptoms also occur.
- nausea;
- vomit;
- diarrhea;
- blood in the stool (this symptom most often appears within a few hours after the disease begins, that is, infarction of the mucous membrane).
With intestinal ischemia, the stomach may hurt
Despite the fact that intense pain appears, there may be no tension in the abdominal wall muscles at all, or it may be very small. If symptoms of peritoneal irritation appear, the prognosis is serious, as necrosis occurs, spreading to all layers of the intestinal wall.
Body temperature is initially normal. Subsequently, symptoms of hypovolemia begin to progress, and pronounced leukocytosis, metabolic acidosis, and hyperamylasemia are also observed. Let us highlight the main symptoms and briefly describe them.
- Abdominal pain. If chronic mesenteric ischemia occurs, the pain is described as “abdominal pain.” It differs in that it is often associated with food intake and occurs approximately half an hour after eating. This pain does not have a specific localization, but is felt near the navel, in the epigastrium and in the projection of the large intestine. The nature of the pain is spastic and cramping; in the initial period it can be relieved with antispasmodics and nitrates. If the pathological process progresses in the mesenteric arteries, the pain will intensify.
- Auscultatory signs. These include increased peristaltic bowel sounds, which is also observed after eating, as well as systolic noise that occurs at a point located midway between the navel and the xiphoid process.
Long-term dysfunction in the intestines is a signal of a health problem
- Intestinal dysfunction. This is expressed by rumbling in the stomach that occurs after eating, severe flatulence and constipation. If the disease lasts for a long time, diarrhea may occur.
- Pronounced weight loss in patients. The weight of patients decreases especially with mesenteric severe ischemia. This happens because patients refuse to eat because the above symptoms occur after eating. The absorption capacity of the intestine is also impaired.
Frequent companions are also:
- vomit;
- diarrhea or constipation;
- loss of appetite.
But these symptoms have little impact on diagnosis. Diagnostics consists of several methods that help make an accurate diagnosis and identify the form of ischemia.
Diagnosis of the disease
Intestinal ischemia is diagnosed by a number of methods.
- CT scan. Thanks to this method, you can view the abdominal organs layer by layer.
- Blood analysis. Leukocytosis indicates an inflammatory process.
Magnetic resonance angiography
- Angiography. This method is especially useful when quick diagnosis is needed. The bottom line is that a catheter is inserted into the femoral artery through the area where the inguinal fold is located. The end of the catheter is passed beyond the point where the branch of the mesenteric arteries from the aorta is located. A radiopaque substance is injected through it. Then X-rays are taken, which help to quickly make a diagnosis and begin treatment.
- Magnetic resonance angiography. Using it, you can obtain a layer-by-layer image of organs and vessels in 3D format.
- Doppler ultrasound. It allows you to evaluate the speed of blood flow and see the place of narrowing or blockage of the lumen in the artery.
- Colonoscopy. Helps examine the large intestine by inserting a flexible colonoscope tube through the rectum, which has a light and a video camera.
- Endoscopy. A special endoscope tube is inserted through the patient's mouth, thanks to which the condition of the small intestine can be examined.
Treatment methods
Ischemia of the large intestine can go away on its own. However, your doctor may prescribe antibiotics to prevent infection. It happens that it is necessary to find and treat the underlying disease that provoked ischemia.
Sometimes you need to stop taking certain medications that also led to this condition. If intestinal damage occurs due to ischemia, surgery may be required to remove the damaged tissue.
Typical symptoms of impaired blood flow with damage to the aorta in the abdominal cavity:
- pain associated with eating (during eating, the stomach and intestines need more blood, but the vessels cannot provide good blood circulation);
- dysfunction of the intestines, as indicated by typical symptoms (diarrhea or constipation, flatulence);
- change in body weight towards weight loss.
DETAILS: Foot ischemia of the lower limb photo
Pain syndrome can be of varying intensity.
If at first the symptoms are not expressed (pulling or pressing in the abdomen), then as the disease progresses, the severity of the pain will increase. In some cases, when the correct diagnosis has not yet been made, treatment may begin with an exploratory operation: the doctor will perform endoscopic surgery in search of the cause of the pain. Ischemia of internal organs in atherosclerosis of the abdominal aorta
| Damage level | Internal organs suffering from impaired blood flow |
| Celiac trunk | Liver, pancreas, stomach, spleen, duodenum |
| Mesenteric | Small and large intestine |
| Visceral | Stomach and duodenum |
| Region of bifurcation and iliac arteries | Pelvic organs and lower limbs |
Symptoms are most pronounced when the arterial trunks are blocked in the area of the visceral and iliac arteries. In the first case, the formation of an acute ulcer in the stomach or duodenum will be typical. In the second, symptoms of lack of blood flow in the lower extremities occur. Treatment in all cases must be carried out with the help of several specialists.
Diagnosis of abdominal aortic aneurysms
Most often, abdominal aortic aneurysms are detected by ultrasound examination of the abdominal organs. Typically, the discovery of an aneurysm is an incidental finding. If a doctor suspects a patient has an aortic aneurysm, modern diagnostic methods are used to clarify the diagnosis.
Methods for diagnosing abdominal aortic aneurysm
- Computed tomography in angio mode;
- Magnetic resonance imaging in angio mode;
- X-ray contrast aorto- and angiography;
- Ultrasound duplex or triplex angioscanning of the abdominal aorta.
If necessary, the abdominal and thoracic aorta is examined.
Diagnostics
Photo: organserdce.com
How to identify an aortic aneurysm if in some cases it develops asymptomatically and is discovered by chance during some examination or autopsy, but is not the cause of death? Some cases have specific signs of aortic aneurysm and lead to all sorts of life-threatening complications. This disease is most often observed in older people. This is caused by age-related pathologies of the vascular walls, the presence of hypertension or metabolic disorders.
There are two types of aneurysm, differing in location in the human body:
- Thoracic aortic aneurysm – located in the thoracic region;
- Abdominal aortic aneurysm is located in the abdominal cavity.
These aneurysms are distinguished by shape, parameters and complications. Signs of an aortic aneurysm determine the course of the disease and the surgical procedure. A complication in the form of internal bleeding in 2 out of 5 cases leads to death.
Establishing diagnosis
Diagnosis of dissecting aortic aneurysm is quite difficult due to several reasons:
- Signs of an aortic aneurysm are not monitored;
- Symptoms correspond to other diseases (for example, cough and discomfort in the thoracic region are observed with pulmonary diseases); Pathology is rarely encountered in medical practice.
If there are signs of the disease, you should consult a therapist or cardiologist. They will conduct an initial examination, based on the results of which examinations are prescribed. After testing, the diagnosis of aortic aneurysm is often confirmed.
How to diagnose an aortic aneurysm?
Diagnosis of dissecting aortic aneurysm is performed using certain instrumental research methods:
- A physical examination serves to collect initial data (complaints) without the use of complex examination methods. Diagnosis of an aortic aneurysm consists of external examination, percussion (tapping), palpation (palpation), auscultation (listening with a stethoscope) and pressure measurement. After detecting characteristic signs, further diagnosis of dissecting aortic aneurysm is prescribed;
- X-ray shows the internal organs of the chest and abdomen. The image clearly shows the protrusion of the aortic arch or its enlargement. To identify the parameters of the aneurysm, a contrast agent is injected into the vessel. Due to the danger and traumatic nature, such diagnosis of dissecting aortic aneurysm is prescribed for special indications;
- Electrocardiography is used to determine the activity of the heart muscle. An ECG of an aortic aneurysm will help distinguish this disease from coronary heart disease. With atherosclerosis, which causes the formation of an aneurysm, the coronary vessels suffer, which can cause a heart attack. How to detect an aortic aneurysm? On the cardiogram, you can track specific signs of an aortic aneurysm corresponding to this pathology of the cardiovascular system;
- Magnetic resonance and computed tomography make it possible to determine all the required parameters of the aneurysm - its location, size, shape and thickness of the vessel walls. The pathognomonic CT sign of a dissecting aortic aneurysm shows wall thickening and a sharp dilation of the lumen of the vessel. Based on these data, possible treatment is determined;
- Ultrasound examination – ultrasound of an abdominal aortic aneurysm is one of the most common diagnostic methods. It helps to determine the speed of blood flow and the existing turbulence that separates the walls of the vessel;
- Laboratory tests include general and biochemical blood tests, as well as urine tests. How to diagnose an aortic aneurysm using tests? They reveal the following signs of an aortic aneurysm: A decrease or increase in the number of leukocytes, characteristic of acute or chronic forms of infectious diseases that precede the formation of an aortic aneurysm. An increase in the number of unsegmented neutrophils is also observed. Increased blood clotting manifests itself in the form of an increase in platelet levels, changes in coagulation factors and indicates the probable formation of blood clots in the aneurysm cavity. High cholesterol levels indicate the presence of atherosclerotic plaques in the vessel. A urine test may show a small amount of blood.
The listed signs of aortic aneurysm are not characteristic symptoms of this disease and are not found in all patients.
Treatment methods for aortic aneurysm
There are several methods for treating aortic aneurysm. It is important to know the advantages and disadvantages of each of these techniques. Approaches to the treatment of abdominal aortic aneurysms:
Monitoring the patient over time
If the aneurysm is less than 4.5 cm in diameter, the patient is recommended to be monitored by a vascular surgeon, since the risk of surgery exceeds the risk of rupture of the aortic aneurysm. Such patients should undergo repeated ultrasound examinations and/or computed tomography at least once every 6 months.
When the aneurysm diameter is more than 5 cm, surgical intervention becomes preferable, since as the size of the aneurysm increases, the risk of aneurysm rupture increases.
If the size of the aneurysm increases by more than 1 cm per year, the risk of rupture increases and surgical treatment also becomes preferable.
Open surgery: aneurysm resection and aortic replacement
Surgical treatment is aimed at preventing life-threatening complications. The risk of surgery is associated with possible complications that include heart attack, stroke, limb loss, acute intestinal ischemia, male sexual dysfunction, embolization, prosthetic infection, and renal failure.
The operation is performed under general anesthesia. The essence of the operation is to remove the aneurysmal expansion and replace it with a synthetic prosthesis. The average mortality rate for open procedures is 3-5%. However, it may be higher if the renal and/or iliac arteries are involved in the aneurysm, as well as due to the patient’s concomitant pathology. Observation in the postoperative period is carried out once a year. Long-term treatment results are good.
Endovascular repair of aortic aneurysm: installation of a stent graft
Endoprosthetics of aortic aneurysm is a modern alternative to open surgery.
The operation is performed under spinal or local anesthesia through small incisions/punctures in the groin areas. Through the above approaches, catheters are inserted into the femoral artery under X-ray control. According to which, in the future, the endoprosthesis will be brought to the aneurysmal extension. An endoprosthesis or stent-graft of the abdominal aorta is a mesh frame made of a special alloy and wrapped in synthetic material. The last stage of the operation is the installation of a stent graft at the site of the aneurysmal expansion of the aorta. Eventually, the aneurysm is “switched off” from the bloodstream and the risk of rupture becomes unlikely. After aortic replacement, the patient is observed in the hospital for 2-4 days and discharged.
This technique allows to reduce the incidence of early complications, shorten the length of patient stay in the hospital and reduce the mortality rate to 1-2%. Observation in the postoperative period is carried out every 4-6 months using ultrasound techniques, CT angiography, X-ray contrast angiography. The endovascular treatment method is certainly less traumatic. About 40,000 such operations are performed annually in the United States alone.
Thus, the choice of treatment method for abdominal aortic aneurysm is based on the individual characteristics of the patient.
Doppler of renal vessels is normal
The normal diameter of the renal artery in adults is 5 to 10 mm. If the diameter is 180 cm/sec. In young people, the aorta and its branches may normally have a high PSV (>180 cm/sec), while in patients with heart failure, the PSV is low even in the area of stenosis. These features are leveled by the renal-aortic ratio RAR (PSV in the area of stenosis/PSV in the abdominal aorta). RAR for renal artery stenosis >3.5.
| Renal artery stenosis | PSV at the site of stenosis | RAR | |
| Norm | 180 cm/sec | 180 cm/sec | ≥3,5 |
| Occlusion | No signal | — |
Direct criteria are preferable; diagnosis should not be based solely on indirect signs. In the post-stenotic region, the flow attenuates - tardus-parvus effect. In renal artery stenosis on the intrarenal arteries, PSV is too late (tardus) and too small (parvus) - AT >70 ms, PSV/AT 0.05 and PI >0.12.
| Signs | Main renal artery | Segmental or interlobar arteries |
| Direct | PSV >180 cm/sec, RAR >3.5 | |
| Indirect | AT >70 ms, AI 5 |
Drawing. A 60-year-old female patient with refractory arterial hypertension. PSV on the abdominal aorta 59 cm/sec. In the proximal part of the RAA with CDK aliasing (1), PSV is significantly increased 366 cm/sec (2), RAR 6.2. In the middle segment of the PPA with CDK aliasing, PSV 193 cm/sec (3), RAR 3.2. On segmental arteries without a significant increase in acceleration time: upper - 47 ms, middle - 93 ms, lower - 33 ms. Conclusion: Stenosis in the proximal part of the right renal artery.
Drawing. Patient with acute renal failure and refractory arterial hypertension. Ultrasound of the abdominal aorta and renal arteries is difficult due to gas in the intestine. On the segmental arteries on the left RI is about.68 (1), on the right RI is 0.52 (2), the difference is 0.16. The spectrum of the right segmental artery has a tardus-parvus shape - acceleration time is increased, PSV is low, the apex is rounded. Conclusion: Indirect signs of stenosis of the right renal artery. CT angiography confirmed the diagnosis: at the mouth of the right renal artery there are atherosclerotic plaques with calcification, moderate stenosis.
Drawing. Patient with arterial hypertension. PSV in the aorta is 88.6 cm/sec (1). In the proximal part of the RPA there is aliasing, PSV 452 cm/sec, RAR 5.1 (2). In the middle section of the PPA there is eleasing, PSV 385 cm/sec, RAR 4.3 (3). In the distal part of the RCA, PSV is 83 cm/sec (4). On the intrarenal vessels tardus-parvus the effect is not determined, on the right RI is 0.62 (5), on the left RI is 0.71 (6), the difference is 0.09. Conclusion: Stenosis in the proximal part of the right renal artery.