5 / 5 ( 3 voices)
The article talks about a complex of heart diseases, united by a common name - acute coronary syndrome. The main manifestations of the conditions and the required measures are described.
Acute coronary syndrome is a concept that combines two acute cardiac pathologies. ACS includes unstable angina and two types of myocardial infarction. This term is used by doctors for urgent treatment.
ACS is a condition that is extremely life-threatening
A little more about terminology
Currently, acute coronary syndrome refers to two conditions that manifest similar symptoms:
Unstable angina
Unstable angina is a condition in which, against the background of physical activity or rest, pain appears behind the sternum, which has a pressing, burning or squeezing nature. This pain radiates to the jaw, left arm, left shoulder blade. It may also manifest itself as abdominal pain and nausea.
Unstable angina is said to occur when these symptoms are either:
- just arose (that is, the person previously performed exercise without heart pain, shortness of breath or discomfort in the abdomen);
- began to occur at less load;
- become stronger or last longer;
- began to appear alone.
Unstable angina is based on a narrowing or spasm of the lumen of a larger or smaller artery that supplies, respectively, a larger or smaller area of the myocardium. Moreover, this narrowing must be more than 50% of the diameter of the artery in this area, or the obstacle in the path of blood (this is almost always an atherosclerotic plaque) is not fixed, but fluctuates with the blood flow, sometimes blocking the artery more or less.
Myocardial infarction
Myocardial infarction - without ST segment elevation or with ST segment elevation (this can only be determined by ECG). It occurs when more than 70% of the diameter of the artery is blocked, as well as in the case when “flying off” plaque, blood clot or drops of fat clog the artery in one place or another.
Acute coronary syndrome without ST segment elevation is either unstable angina or non-ST segment elevation infarction. At the stage before hospitalization in a cardiology hospital, these 2 conditions are not differentiated - there are no necessary conditions and equipment for this. If ST segment elevation is visible on the cardiogram, a diagnosis of “Acute myocardial infarction” can be made.
The treatment of acute coronary syndrome depends on the type of disease - with or without ST elevation.
If the ECG immediately shows the formation of a deep (“infarct”) Q wave, a diagnosis of “Q-myocardial infarction” is made, rather than acute coronary syndrome. This suggests that a large branch of the coronary artery is affected, and the focus of dying myocardium is quite large (large-focal myocardial infarction). This disease occurs when a large branch of the coronary artery is completely blocked by a dense thrombotic mass.
Pathogenesis
Diagnosis of acute coronary syndrome is impossible without understanding how it occurs.
External and internal causes of coronary heart disease lead to the formation of atherosclerotic plaques in the walls of the coronary vessels. A special role here is played by response inflammation - a protective reaction of the vascular wall aimed at its restoration. Therefore, cells that secrete special chemicals accumulate around the accumulation of fats. These substances attract platelets, the cells responsible for blood clotting.
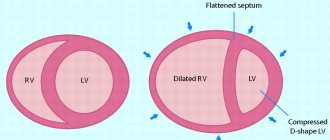
With thrombosis or critical blockage of a vessel, or with plaque rupture, blood flow through the coronary artery is sharply reduced. Each such vessel supplies blood to a separate section of the myocardium - the interventricular septum, apex, lateral or posterior wall, right ventricle. At rest, the amount of blood passing through the narrowed area may still be sufficient to nourish the heart.
During exercise, the heart rate increases. Myocardial cells work more actively, and they no longer have enough of the small amount of oxygen that is delivered through the narrowed artery. Myocardiocytes begin to experience oxygen starvation. The process of normal “combustion” of nutritious foods with the formation of energy is disrupted. Under-oxidized, that is, “under-burnt” substances are poisonous and damage the cell membrane.
This is how ACS occurs, accompanied by prolonged chest pain. This is a “heart signal” about severe distress and the need for urgent rest and restoration of blood flow. These are signs of unstable angina. When blood flow completely stops, heart cells die and a heart attack develops.
We recommend reading about how to relieve an angina attack. You will learn what triggers attacks and how to relieve them at home yourself. And here is more information about what an ECG will tell you about cardiac ischemia.
When to suspect acute coronary syndrome
The alarm should be sounded if you or your relative has the following complaints:
- Pain behind the sternum , the spread of which is shown with a fist, not a finger (that is, a large area hurts). The pain is burning, baking, severe. It is not necessarily found on the left, but can be localized in the middle or on the right side of the sternum. It radiates to the left side of the body: half of the lower jaw, arm, shoulder, neck, back. Its intensity does not change depending on the position of the body, but several attacks of such pain may be observed (this is typical for ST-segment elevation syndrome), between which there are several practically painless “gaps”. It is not relieved by nitroglycerin or similar drugs. Fear joins the pain, sweat appears on the body, and there may be nausea or vomiting.
- Shortness of breath , which is often accompanied by a feeling of lack of air. If this symptom develops as a sign of pulmonary edema, then suffocation increases, a cough appears, and pink, frothy sputum may be coughed up.
- Rhythm disturbances , which are felt as interruptions in the functioning of the heart, discomfort in the chest, sharp jolts of the heart against the ribs, pauses between heartbeats. As a result of such irregular contractions, in the worst case, loss of consciousness occurs very quickly, in the best case, headache and dizziness develop.
- Pain can be felt in the upper abdomen and is accompanied by loose stools, nausea, vomiting , which does not bring relief. It is also accompanied by fear, sometimes by a feeling of rapid heartbeat, irregular heartbeat, and shortness of breath.
- In some cases, acute coronary syndrome may begin with loss of consciousness .
- There is a variant of the course of acute coronary syndrome, manifested by dizziness, vomiting, nausea , and in rare cases, focal symptoms (facial asymmetry, paralysis, paresis, impaired swallowing, and so on).
One should also be wary of intensified or more frequent pain in the chest, about which a person knows that this is the manifestation of his angina, increased shortness of breath and fatigue. Within a few days or weeks of this, 2/3 of people develop acute coronary syndrome.
The following people are at particularly high risk of developing acute cardiac syndrome:
- smokers;
- overweight persons;
- alcohol abusers;
- lovers of salty dishes;
- leading a sedentary lifestyle;
- coffee lovers;
- having a lipid metabolism disorder (for example, high levels of cholesterol, LDL or VLDL in a blood lipid profile);
- with an established diagnosis of atherosclerosis;
- with an established diagnosis of unstable angina;
- if atherosclerotic plaques are identified in one of the coronary (which feeds the heart) arteries;
- who have already suffered a myocardial infarction;
- lovers of eating chocolate.
Symptoms of the disease
The main clinical symptom of ACS is chest pain, varying in both intensity and sensation. It can be squeezing, pressing, burning - these are the most typical forms of pain. An attack of ischemia is provoked by stress, physical activity, emotional stress, and taking certain medications and drugs (amphetamines, cocaine).
Often the pain is not localized only behind the sternum, but radiates to various regions of the body - neck, left arm, shoulder blade, back, lower jaw. Situations are possible when pain is felt exclusively in the upper abdomen, simulating the clinical picture, for example, of acute pancreatitis. In this case, the diagnosis is facilitated by instrumental and laboratory studies. However, the abdominal form of myocardial ischemia still remains the most difficult to diagnose.
The second most common symptom is shortness of breath. Its occurrence is associated with a decrease in the functions of the heart in pumping blood. The appearance of this clinical sign indicates a high probability of life-threatening acute heart failure with pulmonary edema.
The third symptom is the occurrence of various arrhythmias. Sometimes heart rhythm disturbances are the only sign of an impending myocardial infarction, which can occur in a painless form. In this case, there is also a high risk of developing fatal complications in the form of cardiac arrest or cardiogenic shock, followed by the death of the patient.
First aid
Help needs to start at home. In this case, the first action should be to call an ambulance. Next, the algorithm is as follows:
- It is necessary to place the person on the bed, on his back, but at the same time the head and shoulders should be raised, making an angle of 30-40 degrees with the body.
- Clothes and belts must be unbuttoned so that the person’s breathing is not hampered.
- If there are no signs of pulmonary edema, give the person 2-3 tablets of aspirin (Aspekarda, Aspetera, Cardiomagnyl, Aspirin-Cardio) or Clopidogrel (that is, 160-325 mg of aspirin). They need to be chewed. This increases the likelihood of dissolving a blood clot, which (by itself, or layered on an atherosclerotic plaque) has blocked the lumen of one of the arteries supplying the heart.
- Open the vents or windows (if necessary, the person needs to be covered): this will allow more oxygen to flow to the patient.
- If blood pressure is more than 90/60 mm Hg, give the person 1 tablet of nitroglycerin under the tongue (this drug dilates the blood vessels that supply the heart). Nitroglycerin can be given again 2 more times, with an interval of 5-10 minutes. Even if after 1-3 doses a person feels better, the pain has gone away, under no circumstances should he refuse hospitalization!
- If before this a person took drugs from the group of beta blockers (“Anaprilin”, “Metoprolol”, “Atenolol”, “Corvitol”, “Bisoprolol”), after aspirin he should be given 1 tablet of this drug. It will reduce the myocardium's need for oxygen, giving it the opportunity to recover. Note! A beta blocker may be given if blood pressure is greater than 110/70 mmHg and heart rate is greater than 60 beats per minute.
- If a person is taking antiarrhythmic drugs (for example, "Ari") and he feels a rhythm disturbance, he needs to take this pill. At the same time, the patient himself should begin to cough deeply and forcefully until the ambulance arrives.
- All the time before the ambulance arrives, you need to stay close to the person, monitoring his condition. If the patient is conscious and experiences a feeling of fear and panic, he needs to be calmed down, but not given valerian-motherwort (resuscitation may be necessary, and a full stomach can only interfere), but calmed down with words.
- If you have a seizure, a person nearby should help keep your airway open. To do this, it is necessary, taking the corners of the lower jaw and the area under the chin, to move the lower jaw so that the lower teeth are in front of the upper teeth. From this position, you can perform mouth-to-nose artificial respiration if spontaneous breathing has disappeared.
- If the person has stopped breathing, check the pulse in the neck (on both sides of the Adam's apple), and if there is no pulse, proceed with resuscitation measures: 30 straight-arm pressures on the lower part of the sternum (so that the bone moves down), followed by 2 breaths into the nose or mouth. In this case, the lower jaw must be held by the area under the chin so that the lower teeth are in front of the upper teeth.
- Find ECG films and medications that the patient is taking to show them to medical professionals. They won't need it first, but they will need it.
I 20.0 – Unstable angina – example of writing a call card
Patient, 64 years old
Reason for calling – Chest pain (history of coronary artery disease)
Complaints, medical history
Complaints of general weakness, pressing pain behind the sternum, burning sensation radiating to the left shoulder, back (between the shoulder blades), sweating, feeling of lack of air.
The feeling worsened for about 6 hours, the pain arose at rest, intensified with the slightest physical activity, short-term relief after taking isoket spray. I took isoket spray about 10 doses, bisoprolol 10 mg, lisinopril 10 mg, cardiomagnyl 1 tablet. This is not the first time this condition has happened; he was previously treated as an inpatient. During physical activity, she notes infrequent short-term attacks of chest pain, which are relieved with rest after taking nitrates, after 5-10 minutes.
Anamnesis of life
Hypertension stage III. IBS. PEAKS (2012). Diabetes mellitus type II. Cerebrovascular disease.
Regularly takes enalapril 10 mg/day, bisoprolol 10 mg/day, cardiomagnyl 1 tablet/day, maninil 1 tablet/day.
Comfortable blood pressure – 140/90
Physical examination
Condition: moderate;
Consciousness – clear, Glasgow scale – 15 points, behavior – calm;
Pupils – normal, D = S, reaction to light – lively, no gaze paresis, no nystagmus;
Skin – pale, dry, clean;
Heart sounds are muffled, rhythmic, no murmurs. The pulse in the peripheral arteries is of satisfactory quality, rhythmic;
Nervous system – without pathology, no meningeal symptoms;
The pharynx is calm, the tonsils are normal;
Excursion of the chest - normal, type of breathing - normal, percussion - pulmonary sound, auscultation - vesicular breathing, no shortness of breath;
There is no peripheral edema;
The tongue is clean and moist. The abdomen is soft, painless, participates in the act of breathing, there are no symptoms of peritoneal irritation, the liver is not enlarged, stool is formed, 1 time per day;
Urine output is normal, SSPO is negative.
Main pathology
Consciousness is preserved, the patient is adequate. The skin is pale and dry. Heart sounds are muffled and rhythmic. The pulse in the peripheral arteries is of satisfactory quality, rhythmic.
| time | 15-30 | 15-50 | 16-10 | 16-30 | Etc. peace |
| NPV | 18 | 16 | 16 | 16 | 16 |
| Pulse | 86 | 64 | 66 | 64 | 62 |
| Heart rate | 86 | 64 | 66 | 64 | 62 |
| HELL | 160/100 | 150/90 | 140/90 | 140/90 | 140/90 |
| Pace. ºС | 36,6 | ||||
| SpO2 | 95 | 98 | 98 | 98 | 98 |
Blood glucose – 6.5 mmol/l
Troponin test – negative
Electrocardiography
15-35 – Sinus rhythm 86 per minute. Signs of left ventricular hypertrophy. Signs of subepicardial damage to the anterior wall (ST depression I, II, aVL, V1-V4 1-2 mm). Negative dynamics with previous ECGs.
15-50 – Sinus rhythm 64 per minute. No dynamics from the previous ECG.
16-30 – Sinus rhythm 64 per minute. No dynamics from the previous ECG.
Diagnosis by the EMS team
IBS. Unstable angina III B (Braunwald). Post-infarction cardiosclerosis.
What should emergency doctors do?
Medical care for acute coronary syndrome begins with simultaneous actions:
- providing vital functions. For this, oxygen is supplied: if breathing is spontaneous, then through nasal cannulas; if breathing is absent, then tracheal intubation and artificial ventilation are performed. If blood pressure is critically low, special drugs are injected into the vein to increase it;
- parallel recording of the electrocardiogram. They look at it to see if there is ST elevation or not. If there is an increase, then if there is no possibility of quickly transporting the patient to a specialized cardiology hospital (provided that the team leaving is sufficiently staffed), they can begin to carry out thrombolysis (dissolution of a blood clot) in an out-of-hospital setting. In the absence of ST elevation, when it is likely that the clot blocking the artery is “fresh” and can be dissolved, the patient is taken to a cardiology or multidisciplinary hospital where there is an intensive care unit.
- eliminating pain syndrome. To do this, narcotic or non-narcotic painkillers are administered;
- in parallel, using rapid tests (strips where a drop of blood is dropped, and they show whether the result is negative or positive), the level of troponins, markers of myocardial necrosis, is determined. Normally, troponin levels should be negative.
- if there are no signs of bleeding, anticoagulants are injected under the skin: Clexan, Heparin, Fraxiparin or others;
- if necessary, Nitroglycerin or Isoket is administered intravenously;
- Intravenous beta blockers may also be started to reduce myocardial oxygen demand.
Note! The patient can only be transported to and from the car in a lying position.
Even the absence of changes in the ECG against the background of complaints characteristic of acute coronary syndrome is an indication for hospitalization in the cardiology hospital or intensive care unit of a hospital that has a cardiology department.
Treatment tactics
Treatment begins simultaneously with the diagnosis - oxygen inhalation, establishment of venous access. The therapeutic course is carried out in a hospital setting, as round-the-clock ECG monitoring and medical supervision are required.
Treatment is aimed at eliminating the causes of ischemia, pain, reducing anxiety, restoring blood flow, stopping the load on the myocardium and preventing/eliminating complications.
Depending on the severity of the disease, conservative or surgical treatment is prescribed. In addition, the patient must follow general recommendations - strict bed rest, avoidance of stress and physical activity, diet and physical activity after the condition improves.
First aid
If acute coronary syndrome is suspected, emergency care is carried out in the first half hour, only in this case the chance of survival will be quite high. If you have heart pain, you should call a doctor.
Before the specialists arrive, you should lay the person on his back, raising his shoulders and head by 30-40*. Measure the pressure, and if it is within normal limits, give a nitroglycerin tablet. The patient must not be left alone; his condition must be closely monitored.
WHO offers the following algorithm for emergency care by specialists:
- place the patient on a hard, flat surface;
- carry out oxygen therapy to saturate the heart muscle cells with oxygen;
- nitroglycerin under the tongue;
- give the patient an aspirin tablet to chew;
- subcutaneous administration of anticoagulants;
- administration of narcotic painkillers to relieve acute pain.
After stabilization of the patient's condition, he is hospitalized in the nearest cardiology department.
In the absence of breathing and heartbeat, resuscitation measures are carried out until doctors arrive
Basic treatment
After the patient has received first aid for acute coronary syndrome, basic therapy is carried out aimed at restoring the structure and function of the myocardium. The main treatment for acute coronary syndrome depends on the final diagnosis.
Angina pectoris
The main group of drugs for the treatment of angina are beta blockers. This group includes medications such as:
- Anaprilin;
- Metoprolol;
- Atenolol.
The action of these drugs is based on reducing the area of ischemia of the heart muscle and normalizing heart function. The dose of the drug is calculated individually; the medication must be taken constantly. When an attack occurs, use nitrate-containing drugs and aspirin.
For Prinzmetal's angina, calcium antagonists are prescribed - the drug Nifedipine. All patients are prescribed medications that help normalize cholesterol levels. The two most commonly used groups are statins and fibrates.
Myocardial infarction
To treat an acute heart attack, the patient is hospitalized in the cardiac intensive care unit.
Table. Drugs for the treatment of AMI:
| A drug | Effect | Mode of application |
| Morphine | Elimination of acute pain syndrome | Administered intravenously or intramuscularly, dosage is calculated individually |
| Thrombolytics – Streptokinase, Alteplase | Dissolve the blood clot | The greatest effect is observed when the drugs are administered in the first 6 hours |
| Disaggregants – Aspirin, Curantil | Prevents the formation of new blood clots | First administered intramuscularly, then switched to tablet administration |
| Antiarrhythmics - Dopamine | Prevent cardiac arrhythmia | Administered intravenously |
In some cases, when a blood clot cannot be dissolved by medications, surgical removal is required.
Treatment in hospital
Recommendations for acute coronary syndrome concern both additional examination and treatment:
- While continuing therapy necessary to maintain vital functions, a 10-lead ECG is taken again.
- Repeatedly, using (preferably) a quantitative method, the levels of troponins and other enzymes (MB-creatine phosphokinase, AST, myoglobin), which are additional markers of myocardial death, are determined.
- When ST segment elevation occurs, if there are no contraindications, a thrombolysis procedure is performed. The following conditions are contraindications to thrombolysis:
- internal bleeding;
- traumatic brain injury suffered less than 3 months ago;
- “upper” pressure is above 180 mm Hg. or “lower” - above 110 mm Hg;
- suspected aortic dissection;
- previous stroke or brain tumor;
- if a person has been taking anticoagulant drugs (blood thinners) for a long time;
- if there was an injury or any (even laser correction) surgery in the next 6 weeks;
- pregnancy;
- exacerbation of peptic ulcer;
- hemorrhagic eye diseases;
- the last stage of cancer of any localization, severe degrees of liver or kidney failure.
- In the absence of ST segment elevation or its decrease, as well as in T-wave inversion or newly emerging left bundle branch block, the question of the need for thrombolysis is decided individually - according to the GRACE scale. It takes into account the patient’s age, heart rate, blood pressure level, and the presence of chronic heart failure. It also takes into account whether there was a cardiac arrest before admission, whether ST is elevated, or whether troponins are high. Depending on the risk on this scale, cardiologists decide whether there is an indication for clot-dissolving therapy.
- Markers of myocardial damage are determined every 6-8 hours on the first day, regardless of whether thrombolytic therapy was carried out or not: they are used to judge the dynamics of the process.
- Other indicators of the body’s functioning must also be determined: levels of glucose, electrolytes, urea and creatinine, and the state of lipid metabolism. A chest X-ray is performed to evaluate the condition of the lungs and (indirectly) the heart. An ultrasound of the heart with Doppler sonography is also performed to assess the blood supply to the heart and its current condition, and to predict the development of complications such as cardiac aneurysm.
- Strict bed rest - in the first 7 days, if the coronary syndrome ended in the development of myocardial infarction. If a diagnosis of unstable angina has been established, the person is allowed to get up earlier - on the 3-4th day of illness.
- After suffering from acute coronary syndrome, a person is prescribed several medications for continuous use. These are angiotensin-converting enzyme inhibitors (Enalapril, Lisinopril), statins, blood thinners (Prasugrel, Clopidogrel, Aspirin Cardio).
- If necessary, to prevent sudden death, an artificial pacemaker (pacemaker) is installed.
- After some time (depending on the patient’s condition and the nature of the changes on the ECG), if there are no contraindications, a study such as coronary angiography is performed. This is an x-ray method in which a contrast agent is injected through a catheter passed through the femoral vessels into the aorta. It enters the coronary arteries and stains them, so doctors can clearly see what kind of patency each segment of the vascular path has. If there is significant narrowing in any area, additional procedures may be performed to restore the original diameter of the vessel.
Stages
Acute phase
A person usually feels the onset of MI as a sharp deterioration in health and acute pain behind the sternum or in the stomach area. This is how the acute phase of the disease begins. Treatment of the acute phase takes place in the intensive care unit of the cardiology hospital that was closest to the patient at the time of the attack. Its duration is usually 8-12 days. The acute phase ends with the formation of a scar on the heart muscle.
Subacute phase. Why does treatment not end after discharge from intensive care?
After the acute phase of myocardial infarction has been stopped, the health hazard remains. If the blood supply to the heart muscle is not fully restored, a second heart attack may occur. And this happens often. Mortality in the subacute period from repeated attacks is only slightly less than in the primary acute phase.
It is at this point that the patient should consider receiving the most complete modern treatment in a well-equipped clinic. In the subacute phase, it is already possible to move to such a clinic. This is especially important if the necessary measures were not taken in the acute phase—myocardial revascularization was not performed.
Post-infarction period - return to life
It lasts 6-8 months. During this period, proper rehabilitation is of paramount importance, which becomes the basis for the prevention of recurrent MI. In addition, if in the acute and subacute period there was no radical restoration of the vascular network of the heart, this restoration should be carried out as early as possible in the post-infarction period. This way you can minimize the risk of relapse.
Forecast
The overall mortality rate for acute coronary syndrome is 20-40%, with most patients dying before they are taken to the hospital (many from a fatal arrhythmia such as ventricular fibrillation). The fact that a person has a high risk of death can be determined by the following signs:
- a person over 60 years old;
- his blood pressure decreased;
- increased heart rate developed;
- Acute heart failure has developed above Kilip class 1, that is, there are either only moist rales in the lungs, or the pressure in the pulmonary artery has already increased, or pulmonary edema has developed, or a state of shock has developed with a drop in blood pressure, a decrease in the amount of urine discharge, and impaired consciousness;
- the person suffers from diabetes;
- the infarction developed along the anterior wall;
- the person has already suffered a myocardial infarction.
Author:
Krivega Maria Salavatovna resuscitator
Myocardial infarction
Category: Emergency cardiology
In the painful version of MI, the intensity of the pain syndrome (if similar pains have occurred before, with MI they are especially intense), duration (an unusually long attack lasting more than 15–20 minutes), and the ineffectiveness of sublingual nitrates are of diagnostic importance. It must be remembered that with MI, in addition to pain, there are other clinical options.
Therefore, the absence of a convincing clinical picture is not evidence of the absence of MI. Regarding the diagnosis of “myocardial infarction with or without Q wave.” In any case, the patient must be hospitalized in the intensive care ward (unit) of the infarction department. Whether a heart attack turns out to be a Q wave or not is a question that must be decided when the patient is hospitalized. In typical cases, the diagnosis is not in doubt. However, when the ECG picture is unconvincing, preference is given to clinical manifestations. In such situations, overdiagnosis is justified, but only on the condition that the doctor clearly outlined the course of his reasoning and it will be clear to the expert why the doctor acted in this way. Once, one doctor, in response to an expert’s remark about the fact that the patient was not hospitalized, replied: “What should I take him with, because there is nothing on the ECG!” Depending on the diagnosis, the tactical task is also solved. The patient is hospitalized on a stretcher after adequate pain relief.
Myocardial infarction (MI) is necrosis of a section of the heart muscle due to disruption of its blood supply.
The immediate cause of MI is most often the rupture of an atherosclerotic plaque, leading to segmental spasm and thrombosis of the coronary artery. IMs are divided into:
A — By the depth of the lesion (based on ECG changes):
Transmural or large-focal - with a Q wave, with ST elevation in the first hours of the disease and the formation of a Q wave subsequently.
Non-transmural or small-focal, without Q waves, manifested by negative T waves.
B.- According to the clinical course:
Uncomplicated and complicated.
B. By localization:
Left ventricular infarction: anterior, inferior (posterior), septal.
Right ventricular infarction.
At the prehospital stage, the diagnosis of acute myocardial infarction (or ACS with ST elevation) is made based on the clinical picture and ECG changes. An indirect sign of MI, which does not allow one to determine the phase and depth of the process, can be an acutely occurring bundle branch block, of course, with an appropriate clinical picture [19]. The most typical places of localization and irradiation of pain during MI are shown in the following figure (Fig. 33).
The daily work of an ambulance provides a wealth of material that can be used to analyze defects, and therefore for training. The famous domestic therapist, cardiologist, great expert on emergency medicine, Professor L. A. Leshchinsky, in his review of the book by V. A. Fialko, wrote:
“Study other people’s mistakes so you can make fewer of your own!”
Let us give another example, which was the subject of analysis at a meeting of the LEC, which has been operating at the station for more than 50 years
B-ya M, 76 years old, the call came at 5:29. Arrival – 5 hours 43 minutes.
Complaints: pain in the chest over the entire surface, “goosebumps” in both arms on the skin and fingertips, diffuse headache, pain when trying to breathe deeply.
History: pain in the chest and spine has been bothering me for a long time. This morning I woke up with a feeling of numbness in my back, tried to turn around and felt a sharp pain in my back. Didn't take any pills. (The style of writing the map has been preserved).
Objective examination data: Heart sounds are rhythmic, sonorous, no murmurs. The chest is hypersthenic, there is vesicular breathing in the lungs, there is no wheezing. The abdomen is soft and painless in all parts. Blood pressure – 180/100 mm. RT. Art. (with the usual for the patient – 120/80), pulse rate 75 per 1 min. The patient had an ECG recorded (See Fig. 34).
Conclusion: Signs of incomplete blockade of the left branch of the His bundle, left ventricular hypertrophy. There is no ECG for comparison. The patient was prescribed: clonidine – 2t, nitroglycerin. After therapy, blood pressure decreased to 160/80 mm (Whether the pain attack was stopped is unknown).
Diagnosis: Hypertension, crisis II, spinal osteochondrosis. The patient was left at home; instead of transferring the call to the clinic, the doctor wrote down: “They will call the local doctor themselves.” The brigade is released at 6:06 am. The time spent on the call is 23 minutes. Just 20 minutes later (6 hours 26 minutes) the call comes again.
Complaints: pressing pain behind the sternum, intense, radiating to both arms, wavy in nature.
History: I fell ill at night, when pain appeared in the chest, I took nitroglycerin, without effect. History: IHD, exertional angina pectoris II - III functional class, hypertension II B, crisis course. The doctor noted that the ambulance was called again. On the repeated electrocardiogram: signs of damage to the myocardium of the anteroseptal region with transition to the apex (Fig. 35).
The second doctor called the cardiology team to clarify the diagnosis of myocardial infarction. The specialist team doctor wrote down: (See page 70).
Complaints: intense pressing pain in the chest area, without irradiation, general weakness.
History: These complaints first appeared at 11 p.m., lasted about 30 minutes, and were relieved by taking nitroglycerin. This morning, at about 5 o'clock, I woke up due to similar pressing pains. Taking nitroglycerin - no effect. She called an ambulance. After therapy carried out by the second line team, the pain disappeared and the patient fell asleep. By the time the special team arrived, the patient woke up and again complained of pressing pain.
Objectively: Pulse rate – 45 beats per minute, blood pressure 60/40 mm. rt. Art. (usual-140/80). After the therapy, the patient was anesthetized, blood pressure stabilized at 100/60 mm, then 110–70 mm. With a diagnosis of coronary artery disease, acute primary myocardial infarction of the anteroseptal, apical localization, lateral wall of the left ventricle, shock I, the patient was hospitalized in the cardiology center. According to information received from the cardiocenter, the patient’s condition remained serious and she was in the intensive care unit for 5 days.
Let's analyze this case. It is noteworthy that the amount of information obtained from the same patient is directly dependent on the qualifications of the doctor who received this information. Let's compare: at the first doctor - the attack began in the morning, she did not take any pills. Special brigade doctor - the pain appeared in the evening, around 11 p.m., lasted about 30 minutes, was relieved by taking nitroglycerin. The first doctor’s diagnosis was hypertension, crisis. Osteocondritis of the spine. The second doctor’s diagnosis, which she made literally 30 minutes later, was myocardial infarction. (This is a young doctor who recently completed her emergency medicine internship). Her diagnosis was confirmed by a doctor from the special team, and later at the cardiology center. It is quite possible that the patient also has osteochondrosis of the thoracic region. But no differential diagnosis was carried out, with ischemic heart disease, which cannot be excluded at the age of 76 years, and there was no attempt to make this differentiation. Although the answer would be obvious: in the evening nitroglycerin helped, in the morning with similar pain there was no effect. The above example is another confirmation of what was said above: a superficial, formal collection of anamnesis, such as “I got sick at that time, took this and that,” does not provide anything to obtain the information necessary to get an idea about the patient and, therefore, to make a correct diagnosis. And if the first doctor did not receive the necessary data, as a result of which she made an incorrect diagnosis, and therefore acted tactically incorrectly - she left the patient at home, it is her own fault. All three doctors had the same capabilities, especially since as the disease progressed, the patient’s condition worsened: by the time the specialized team arrived, the blood pressure had dropped to 60/40 mm. rt. Art. and this gave the right to the doctor of the special team to diagnose shock - I. As for the increase in blood pressure, which the first doctor regarded as a crisis, this, of course, was compensatory hypertension, with which the body sought to improve regional blood circulation, in this case coronary. Therefore, the prescription of an antihypertensive drug (clonidine) was not indicated, to say the least. One more detail. The information contained in the first doctor’s card (without ECG data!) was entered into the differential diagnostic computer program SOMIVTs “Emergency Cardiology”. The answer was: “Spontaneous angina. The most likely diagnosis." And this is another confirmation of the fact that even the meager data contained in the first card was enough to make a correct diagnosis (even without an ECG).
In such analyses, opponents like to object, arguing that when the result is known, it is easy to look for “something to complain about,” in this case, the lack of convincing data on the first ECG. Indeed, with a quick glance at the first entry it is difficult to pay attention to anything. After all, it is unknown how this episode will end. But the whole point is that you need to look at the ECG not at the beginning of meeting the patient, but... at the end. And “in the beginning there was the word,” that is, complaints, anamnesis. Close attention to the ECG should be caused by the patient’s leading complaints and a carefully collected and analyzed anamnesis and, above all, an anamnesis of the attack. And not just a formal anamnesis, as a list of unrelated facts, which we pointed out above, but a comparative analysis of these facts, it is then that the ECG should be examined especially carefully, i.e., you need to predict the situation, paying attention to every “little detail” ", especially if there is a possibility of comparison. If this is not possible, any changes present on the ECG should be perceived as fresh. This will help avoid mistakes. Moreover, if it is known that in the evening the attack was stopped with nitroglycerin, and in the morning, with a similar nature and localization of pain, it no longer helped, what else is needed in order to diagnose or at least suspect a real threat and make the right tactical decision? Do you need dynamics on the ECG for this? It seems that this entry appears as some kind of means of protecting the doctor from an illiterate conclusion!
The analyzed example once again confirmed the truth that the clinical manifestation of the disease should be given preference over its electrocardiographic display.
The well-known monograph by Ukrainian authors “Coronary heart disease in young people” [6] provides a list of clinical symptoms preceding myocardial infarction (Fig. 36) and the first symptoms of myocardial infarction (Fig. 37). The authors also give percentages of these symptoms. The given schemes can provide significant assistance in the early diagnosis of this terrible disease, even without the use of ECG data.
Back to section
www.03-ektb.ru
How is ACS detected?
Prehospital physicians are extremely limited in the means of diagnosing acute coronary syndrome.
Therefore, they are not required to make an accurate diagnosis. The main thing is to correctly interpret the data available at the time of examination and transport the patient to the nearest medical center for final identification of the disease, observation and treatment. An emergency physician or therapist suspects ACS based on:
- medical history data (what could have provoked the attack, whether it was the first, when the pain occurred and how it developed, whether the pain was accompanied by shortness of breath, arrhythmia and other signs of ACS, what medications the patient took before the attack);
- data from listening to heart sounds, blood pressure numbers;
- electrocardiographic study data.
However, the main diagnostic criterion is the duration of chest pain. If the pain lasts more than 20 minutes, the patient is given a preliminary diagnosis of ACS. Depending on the ECG signs, it can be supplemented with information about the presence or absence of ST segment elevation.