Victoria Popova
Cardiologist
Higher education:
Cardiologist
Saratov State Medical University named after. IN AND. Razumovsky (SSMU, media) Level of education - Specialist 1990-1996
Additional education:
“Emergency Cardiology”
1990 - Ryazan Medical Institute named after Academician I.P. Pavlova
Contacts
Acute vascular insufficiency is a clinical syndrome that is characterized by a decrease in the amount of circulating blood and impaired circulation in vital organs. Pathology is caused by a decrease in vascular tone, changes in myocardial contractions, and blood loss. Manifestations of the disease include collapse, shock, and fainting.
Causes and classification
Pathology is a complication of various diseases or occurs as a reaction to negative external influences.
According to the nature of the disease, it can be:
- acute;
- chronic.
Depending on the type of damaged vessels, the following forms of insufficiency are distinguished:
- arterial;
- venous.
When acute vascular insufficiency occurs, the size of the bed exceeds the volume of circulating blood. The development of the disease is characterized by different scenarios.
The main mechanism for the onset of the disease is considered to be sudden dilation of blood vessels. In this case, the amount of blood becomes insufficient for the size of the arteries or veins. Traumatic injuries, stress, and complex poisoning lead to the appearance of the disease. Pulmonary embolism and myocardial infarction are also provoking factors.
The second option for the appearance of the disease is a sharp decrease in the amount of circulating blood, while the size of the bed remains the same. This form of acute vascular insufficiency is caused by significant blood loss. It is also caused by loss of other fluids. Provoking factors include diarrhea, vomiting, bleeding, and dehydration.
Acute vascular insufficiency syndrome can manifest itself in the following clinical forms:
- fainting;
- collapse;
- shock.
Depending on the mechanism, the latter can have the following types:
- Hypovolemic – is a sudden decrease in the amount of circulating blood. This condition can be hemorrhagic, traumatic and dehydrating.
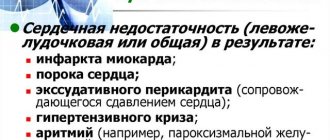
- Cardiogenic – caused by impaired functioning of the heart. This condition is caused by arrhythmia, myocardial infarction, and cardiomyopathy. May occur in acute myocarditis.
- Septic – associated with the influence of toxic substances on the vasomotor centers. This condition may be exotoxic or endotoxic. In the first case we are talking about external toxic influences, in the second – about infectious pathologies.
ethnoscience
Acute vascular insufficiency is a clinical syndrome that develops with a sharp decrease in the volume of circulating blood, its flow to the heart and blood supply to vital organs.
Most often, loss of tone and dilation of blood vessels is observed in the abdominal organs. Acute vascular insufficiency can manifest itself in the form of the following syndromes: fainting, collapse and shock.
Cause of appearance: intoxication, acute infectious diseases, hyperthermia, mental and physical trauma, bleeding, myocardial infarction, severe allergic reaction with the development of anaphylactic shock, burn, surgery, etc.
Fainting (Syncopa) is a mild and rapidly passing form that occurs as a result of acute cerebral ischemia.
It is observed in practically healthy people after a long stay in a stuffy room, with the sight of blood, overwork, as well as after blood loss and with diseases of the cardiovascular system.
Fainting is manifested by sudden weakness, a feeling of lightheadedness, nausea, dizziness, darkening of the eyes and rapid loss of consciousness. The pulse is weak, rare, blood pressure is low, the patient is pale. The muscles are usually relaxed, there are no cramps.
This condition lasts for several minutes, after which it usually goes away on its own; the patient must be placed with a pubescent head to improve blood flow to the brain. They give you ammonia to smell and splash cold water on your face.
Cordiamin or caffeine can be injected under the skin as a tonic.
Emergency care for fainting: place the patient in a horizontal position with the head end of the bed slightly lowered (this is especially important after heavy blood loss), ensure a sufficient flow of fresh air, unbutton (tear) tight clothing, sprinkle cold water on the chest, face, warm the extremities (heating pad), give ammonia a whiff.
Collapse by a drop in blood pressure and deterioration of blood supply to vital organs. In humans, it manifests itself as severe weakness, sharpened facial features, pallor, and coldness of the extremities.
Causes of collapse . Occurs due to infectious diseases, poisoning, large blood loss, overdose, cardiovascular, infectious and other diseases, side effects of certain drugs, etc.
Emergency care is carried out vigorously, which determines the prognosis. It is necessary to replenish the mass of circulating blood, which is especially important in case of blood loss.
Vasoconstrictors are administered (norepinephrine, preferably mesaton), prednisolone intravenously, plasma up to 100 ml, strychnine subcutaneously, 850-1000 ml of saline or 5% glucose solution with the addition of 5% ascorbic acid solution (3-5 ml} and 0.4- 1 ml of 10% caffeine solution subcutaneously. The liquid can be administered by drip, enema or subcutaneously.
When indicated, painkillers (promedol, analgin) are administered, after improvement of the condition - cordiamine, for persistently low blood pressure - ephedrine 0.3-0.75 ml of a 5% solution intravenously.
After this, causal treatment begins. Stimulation of cardiac activity does not make sense, since the heart muscle suffers little.
Restoring vascular tone and increasing blood flow to the heart will improve the functioning of the heart muscle.
Types of collapse:
- cardiogenic collapse - decreased cardiac output.
- hypovolemic collapse - decrease in blood volume.
- vasodilatory collapse - vasodilation.
Shock is a severe form of acute vascular insufficiency that develops as a result of trauma, burns, surgery, blood transfusion, anaphylactic reaction, for example, to the administration of an antibiotic or other drug to which the patient is hypersensitive.
Causes of shock: infections (typhoid and typhus, infectious pneumonia, poisoning, significant blood loss, diseases of the endocrine and nervous system, tumors, acute diseases of the abdominal organs - peritonitis, etc.), myocardial infarction, anesthesia. Also, in case of shock, the most common cause of vascular insufficiency is trauma, extensive crushing of tissue (bruise, surgery), blood loss.
Anaphylactic shock when administered various allergens, such as medications, can last from several minutes to a day or more, depending on the amount of allergen administered. In this case, shock occurs as a result of an increase in vascular permeability and the release of a significant part of the blood from the bloodstream into the tissue.
Traumatic shock has a so-called erectile phase, in which the patient is excited, often suffers from pain, and blood pressure may be elevated. Somewhat later, the phenomena of vascular insufficiency described above appear. With myocardial infarction, vascular insufficiency can be combined with heart failure and stagnation in the pulmonary circulation.
Treatment of vascular insufficiency.
Treatment of vascular insufficiency is closely related to the treatment of the underlying disease. Depending on the cause - stopping bleeding, removing toxic substances from the body, using specific antidotes, eliminating hypoxia, etc.
All therapeutic measures are carried out:
- against a background of absolute peace;
- the patient is not transportable;
- hospitalization is carried out only after the patient has been brought out of collapse (if the therapy started on site is ineffective - by a specialized ambulance, in which all necessary treatment measures are continued).
The diagnosis of collapse requires the immediate initiation of active therapy and at the same time calling a doctor.
Drug treatment begins with the introduction of tonics and stimulants under the skin (cordiamin, mezatone, sulfocamphocaine).
If the effect of these drugs is insufficient, 1-2 ml of a 0.2% solution of norepinephrine in a glucose solution or isotonic sodium chloride solution (150-200 ml) is administered intravenously.
Intravenous drip administration of hydrocortisone (100-200 mg or more, depending on the severity of vascular insufficiency) is very effective.
Intravenous administration of blood substitutes (polyglucin, blood plasma, etc.), which increase the volume of circulating fluid, is also important.
Source: //www.prirodlekar.ru/archives/3981
Clinical picture
The key sign of pathology is a sudden decrease in blood pressure. Other manifestations of the disease are associated with this symptom.
Symptoms of fainting
The term refers to a sudden short-term loss of consciousness that lasts 3 minutes. As a rule, it is preceded by certain symptoms.
The harbingers of this disorder include the following:
- nausea and vomiting;
- tinnitus;
- dizziness;
- darkness in the eyes;
- cold sweating.
Symptoms of fainting include the following:
- loss of consciousness – it lasts from a few seconds to 3 minutes;
- sudden pallor of the skin and mucous membranes;
- constriction of the pupils;
- pressure drop;
- lack of reaction to light;
- muffled heart sounds.
Usually, fainting goes away on its own and does not require specific therapy. If such symptoms recur, first aid for acute vascular insufficiency should be provided.
Signs of collapse
This term refers to an acute form of vascular insufficiency, in which, against the background of a drop in pressure, hypoxia of the brain occurs and vital functions are inhibited.
Key symptoms of collapse include the following:
- sudden disturbance of general condition;
- increased sweating;
- blanching or marbling of the dermis and mucous membranes;
- blue lips;
- shallow breathing;
- increased heart rate;
- decrease in body temperature;
- state of stupor - in this case the person does not respond to external factors;
- sharpening of facial features;
- decrease in pressure - the severity of a person’s condition depends on specific indicators;
- so-called clapping heart sounds;
- collapse of veins.
Are you familiar with the symptoms of vascular insufficiency?
Not really
Manifestations of shock
This is a form of the disease characterized by severe deterioration in well-being and disruption of the nervous system, heart and blood vessels.
Regardless of the reasons for the appearance of this condition, the following manifestations occur:
- reduction in pressure parameters to 90 mm Hg. Art. and less;
- decrease in pulse pressure to 20;
- increased heart rate;
- pallor of the dermis;
- impairment of consciousness and even loss of consciousness;
- lack of urination;
- cyanosis of the dermis of the extremities;
- the appearance of sticky sweat;
- a symptom of the so-called white spot - when pressing with a finger on the skin of the foot for three seconds, it does not immediately smooth out;
- change in the acid-base composition of the blood.
Shock requires emergency hospitalization. In this case, intensive therapy is carried out for acute cardiovascular failure, since the person is not able to get out of this condition on his own.
Extreme manifestations of the disease
Acute vascular insufficiency is characterized by a decrease in blood pressure - hypotension. Its extreme manifestations are fainting, collapse, shock.
Fainting
This is a mild form of blood supply deficiency. The patient suddenly feels dizzy and nauseated. Notices blurred vision and ringing in the ears. The skin of the face turns pale.
Then the person loses consciousness. Breathing becomes rare, deep, the pupils are dilated. Within a few minutes the patient comes to his senses.
If fainting lasts more than five minutes, convulsions may occur.
Reasons for development:
- A sharp decrease in blood pressure. Occurs if there are heart diseases accompanied by heart rhythm disturbances.
During physical stress, blood flow in the muscles increases due to blood redistribution. The heart cannot cope with the increased load, blood output decreases, and blood pressure decreases.
- Dehydration. In this case, the total blood volume decreases due to increased sweating, fluid loss due to diarrhea, and excessive urination.
- Impulses from the nervous system. Pain, fear, strong emotional arousal can lead to sharp vasomotor reactions.
- Severe tension in internal organs. During coughing and urination, tension in the internal organs increases, which reduces the volume of blood that returns to the heart.
- Partial disruption of the blood supply to the brain, a micro stroke can also lead to fainting.
- Hypocapnia. A decrease in carbon dioxide in the blood due to frequent, deep breathing can lead to fainting.
Collapse
This is a more serious manifestation of acute vascular insufficiency. It comes up unexpectedly. The patient's consciousness is preserved, but inhibition is observed.
The skin is pale, there is slight cyanosis of the extremities. Breathing is shallow and rapid. The face is covered with cold sweat. The blood pressure is low and the pulse is weak.
Further development of collapse can lead to loss of consciousness.
Types of collapse:
- Cardiogenic. Occurs in heart diseases that cause impaired cardiac output and decreased blood circulation to organs.
- Hypovolemic. Characterized by a decrease in the volume of blood circulating in the system.
- Vasodilator. There are pronounced changes in vascular tone, microcirculation of organs and tissues is disrupted.
The causes of disturbances leading to collapse make it possible to distinguish some of its forms.
- Infectious-toxic. Occurs in diseases whose pathogens can produce endotoxins (peritonitis, pneumonia). An increase in their content in the patient’s blood (septic condition) can lead to collapse.
- Pancreatic. Occurs due to trauma to the pancreas. The proteolytic enzymes produced by it enter the blood and destroy the walls of blood vessels.
- Hemorrhagic. Accompanied by posthemorrhagic anemia. Occurs due to blood loss.
- Dehydration. A pathological condition characterized by a decrease in the liquid portion of the blood. An increase in vascular permeability leads to its leakage into the intercellular space.
- Orthostatic. In the mechanism of orthostatic collapse, with a sharp change in body position, both hypovolemic and vasodilator disorders may be present.
- Hypoxic. Occurs in conditions of low atmospheric pressure, in the mountains, or when there is low oxygen content in the air.
- Hyperthermic. It is observed when the body overheats in a bath, sauna or sunstroke.
Shock
This is the most serious form of acute heart failure. Many researchers find no difference in the pathogenesis of collapse and shock.
The mechanisms of their development are similar, but shock is characterized by a sharp effect on the body of damaging factors. Leads to severe circulatory disorders.
It has three flow phases.
- Erectile. The patient is excited and screams. Blood pressure may be elevated and the pulse may be rapid. This phase quickly flows into the next, sometimes it is so short-lived that it ends faster than the patient comes under the supervision of a doctor.
- Torpidnaya. The central nervous system is inhibited. The pressure drops and the pulse becomes thready. The patient is inhibited and apathetic. The skin is pale, cyanosis of the extremities is pronounced. Frequent shallow breathing, shortness of breath.
- Terminal. Occurs when the adaptive capabilities of the body are completely disrupted. The pressure is below critical, there is no pulse. There is no consciousness. Death comes quickly.
Depending on the reasons that cause shock, there are:
- Hemorrhagic. Occurs in case of heavy blood loss.
- Traumatic shock. Occurs with severe or multiple bone fractures and soft tissue injuries.
- Burn shock. Often depends on the size and depth of the burn surface.
- Anaphylactic shock. This is an acute complication of allergies. The introduction of an allergen into the body causes an immediate allergic reaction. Develops quickly.
The patient is excited, he experiences fear, possibly skin itching, convulsions, and bronchospasm. Occurs when administered medications or insect bites.
- Blood transfusion. It develops as a result of transfusion of blood or red blood cells that are incompatible with the patient’s blood group.
Features of pathology in children
Children react more sharply to external factors compared to adults. Their different forms of the disease are characterized by specific symptoms. Thus, warning signs of fainting include ceasing contact with adults. Children often experience high convulsive readiness.
With the development of collapse against the background of acute vascular insufficiency in children, in addition to the main manifestations, there is a risk of blue discoloration of the epithelium of the extremities. This condition has several stages:
- At the first stage, there is excitement, increased muscle tone and blood pressure. There is also a risk of tachycardia. It represents an increase in heart rate.
- The second stage is characterized by inhibition. The baby's skin takes on an earthy tint, the legs become blue, muscle tone decreases, blood pressure drops and the pulse slows down. There is also a decrease in the volume of urine excreted.
- The third stage is characterized by depression of the baby’s consciousness, a decrease in body temperature, and the appearance of bluish spots on the skin. The child's breathing and heartbeat slow down, blood pressure drops, and there is no urine output.
Children most often develop hypovolemic shock. The younger the patient, the sooner dangerous symptoms occur. Babies are characterized by rapid dehydration. This is due to unstable thermoregulation. It is also common for children to have insufficient development of neurohumoral regulation of tone. Therefore, in this case, emergency care for acute vascular insufficiency is of primary importance.
First aid
Providing emergency care for acute cardiovascular failure is aimed at restoring and preserving the life of a person with such a diagnosis. The relevance and timeliness of this is noted by doctors.
First of all, it is worth assessing the patient’s condition, and then starting appropriate measures. When fainting due to acute cardiovascular failure, consciousness may be blurred or completely lost. In this case, paleness of the epithelium, dilation of the pupils, weakening of the pulse and decreased breathing are observed.
First aid tactics for acute cardiovascular failure involve performing the following actions:
- The patient should be placed on his back and his head slightly lowered;
- unbutton clothes and provide fresh air;
- in a fan-shaped manner, bring a cotton swab dipped in ammonia to your nose;
- Spray your face with cool water.
Collapse may also occur, characterized by a decrease in vascular tone, symptoms of cerebral hypoxia, and suppression of many important functions. In this case, the patient seems weak, he experiences chills, dizziness, and a decrease in temperature.
In such a situation, it is first of all necessary to remove the cause of circulatory disorders in the vessels. Then it is recommended to do the following:
- lay the patient horizontally;
- loosen tight clothing to provide fresh air;
- warm a person with a heating pad or hot tea;
- rub the limbs with alcohol.
If possible, it is recommended to immediately administer Cordiamine or Caffeine subcutaneously. In difficult situations, intravenous administration of Strophanthin with glucose solution is indicated. Ephedrine or Adrenaline can also be administered subcutaneously.
In a state of shock, the patient should be hospitalized immediately. This will help save the patient's life. Shock is a certain reaction to the influence of external factors. It is characterized by a sudden suppression of all important body functions.
At the initial stage of the pathology, a person experiences increased agitation, anxiety, and chills. As the disease progresses, pressure rapidly drops, temperature decreases, and tachycardia increases.
In this condition, first aid consists of intravenous administration of Prednisolone, Trisol and Contrical solutions. The nursing process for acute failure is to manage symptoms and transport the patient to the intensive care unit.
Medical therapy
Before transporting the patient to the hospital, the introduction of vasoconstrictors can be used - Cordiamin, Caffeine, Mezaton, Norepinephrine. If collapse occurs due to loss of fluid or blood, then the administration of such drugs is carried out only after restoration of the volume of circulating blood with the help of Reopoliglucin, Stabizol, Refortan or saline solutions.
In severe cases and in the absence of peptic ulcer, hormonal drugs (Dexamethasone, Prednisolone, Hydrocortisone) are used.
Inhalation of humidified oxygen is indicated for patients with hypoxic collapse, carbon monoxide poisoning, and severe infections. In case of intoxication, infusion therapy is carried out - the introduction of glucose, isotonic solution, and vitamins. In case of bleeding, blood transfusions or plasma substitutes are used.
Patients with heart failure additionally receive cardiac glycosides; in case of arrhythmia, it is necessary to restore the rhythm with the help of Novocainamide, Cordarone, Atropine (for conduction block, bradycardia). If collapse develops against the background of a severe attack of angina or heart attack, then intravenous administration of neuroleptics and narcotic analgesics and anticoagulants is carried out.
Treatment methods
For treatment of pathology to be effective, it is necessary to make a correct diagnosis. It is important that therapy is comprehensive.
If acute vascular insufficiency is accompanied by fainting, medications are not required. In this case, the patient should be laid down and his legs raised, loosen tight clothing and rinse his face with water. If they do not help, it is worth injecting vasoconstrictors.
When collapse develops, it is important to take measures to eliminate the causes of its occurrence. Therapy is carried out in a hospital setting. The patient should be laid down, legs elevated, and warmed. Before transportation, it is worth giving an injection of a vasoconstrictor medication.
In the hospital, medications are used that influence the mechanism of development of the pathology and eliminate the cause of its occurrence. The following remedies are usually indicated:
- Drugs that lead to stimulation of the respiratory and vascular centers. They tone blood vessels. These substances also increase the stroke volume of the heart.
- Vasoconstrictor drugs. With this diagnosis, intravenous administration of Adrenaline, Dopamine and other hormones is indicated. They are used by drip method.
- Detoxification products. These include antidotes and detoxification solutions. Such treatment is required for intoxication of the body and infectious pathologies.
- Blood and its substitutes. These substances are needed for anemia and blood loss. When administering them, it is recommended to perform a compatibility test with the patient's blood. Otherwise, there is a risk of hemorrhagic shock.
- Anti-inflammatory drugs. If the cause of the problem is an infection, antibacterial medications are prescribed.
- Oxygen therapy. This treatment is aimed at improving metabolic processes and oxygen saturation of the blood.
- Volume restoration. To do this, colloidal solutions or plasma are administered. Salt-containing products can also be used.
If a person is in a state of shock, treatment is aimed at normalizing system functions and eliminating the causes of the disorder. The following remedies are usually indicated:
- Painkillers. Their use is especially important for traumatic injuries and burns. With this diagnosis, narcotic medications are usually chosen. It is worth considering that Morphine suppresses the respiratory center. That is why it is not prescribed to people with such disorders.
- Substances for normalizing blood circulation. These include glucose, saline and colloidal solutions.
- Oxygen therapy. Such treatment is required in a state of shock. If necessary, artificial ventilation is performed.
- Normalization of acid-base balance. In this case, alkalizing solutions and products based on potassium and calcium salts can be used.
- Hormones. Such drugs help restore blood pressure parameters and normalize hemodynamics.
- Diuretics. Such medications cope with swelling.
Prevention
To prevent pathology, it is recommended to monitor the condition of blood vessels. Doctors advise:
- Take hypertensive drugs with great caution. This should only be done as prescribed by a doctor.
- Exercise. It is best to give preference to physical therapy and aerobics.
- Avoid overheating in the sun or in a bath.
- Reduce the consumption of alcoholic beverages, eliminate smoking.
- Adjust your diet. You should definitely give up junk food, which negatively affects the condition of blood vessels.
Acute vascular insufficiency is a dangerous pathology that can have different course options. To cope with the symptoms of the disease, it is necessary to make a correct diagnosis and select effective treatment.