For what heart diseases is a disability group given?
Heart diseases for which a disability commission is assigned.
Disability can be given if a person has suffered severe heart disease, although disability is not given for all diagnoses of cardiovascular diseases.
During a medical and social examination, disability can be given - in case of heart defects, if it is a congenital defect; aortic valve defects; with hypertensive heart disease of the 3rd degree; myocardial infarction; serious changes in the functioning of the heart muscle and circulatory disorders of the 3rd degree; constant angina.
In general, if you have the above-mentioned heart diseases, you can be given disability if you contact a medical and social expert with all the necessary documents, as directed by a doctor.
Be healthy!
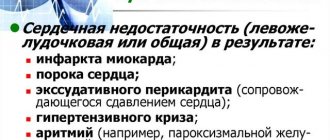
The indication for determining the disability group is not so much the disease itself of some organ or system, but the functional disorders to which it led. In heart disease, for example, this may be
-severe circulatory failure, sharply reducing the patient’s quality of life or depriving him of the ability to work.
- this is a stroke, after which there was a pronounced neurological deficit, and so on.
Heart diseases can be different, but their outcome is often the same, for example, a stroke can be complicated by hypertension, atrial fibrillation, some heart defects, and ultimately all will lead to circulatory failure.
A conclusion on disability is given by an expert doctor in a hospital after a series of examinations. So, for example, disability is given to people who have been diagnosed with cardiovascular diseases such as:
According to this list, the doctor decides to assign a disability group. And since diseases can progress, approximately once a year the patient undergoes a second commission for the purpose of re-examination and assignment of a different disability group.
Heart disease is a serious condition of the body that prevents a person from living and working, just like many other diseases for which doctors are in no hurry to give disability.
However, there are heart diseases that necessarily result in disability.
Disability is assigned only if health problems lead to restrictions on a person’s social activity. The disability group depends on the degree of impairment.
Diseases of the cardiovascular system themselves are not indications for establishing disability, but can lead to severe health disorders, which can be considered by medical and social cardiological commissions as conditions for establishing disability.
Previously, such diseases were listed in the recommendations for commissions, but now this approach is considered incorrect, and the basis for establishing disability is solely the limitations and functional disorders of the body, such as a person’s inability to move, self-care, communicate, work, and learn. Moreover, to obtain disability, not one parameter must be present, but several at the same time.
Disability criteria for patients with pacemaker
Third group. Against the background of a normally performed operation and an improvement in the patient’s quality of life, the following is observed: a positive bicycle ergometry test, a moderate hemodynamic disturbance, and a determination of persistent rejection of the implanted device, expressed in a change in personality. Also, after implantation of an pacemaker and the development of arrhythmia, they are given disability in the event of a change in place of work with an expected reduction in the load of production work, a change in profession or qualifications.
Second group. The operation to implant a permanent pacemaker was ineffective: previously identified arrhythmias persist; There is interference between the rhythms of the patient’s own and the pacemaker, and severe coronary or heart failure has appeared.
4.50 Aug. rating ( 89 % score) – 6 votes – ratings
How does atrial fibrillation occur?
Atrial fibrillation affects approximately 1% of adults worldwide. The frequency of this pathology among adults doubles with every decade of life. In addition to old age, risk factors for the development of MA include organic diseases of the cardiovascular system: arterial hypertension (hypertension), coronary heart disease (CHD), mitral valve defects (stenosis, insufficiency) usually of a rheumatic nature, as well as increased function of the thyroid gland (hyperthyroidism) .
However, less than a tenth of patients with this pathology do not have any organic heart disease. Atrial fibrillation can also be caused by conditions that are not accompanied by structural changes in the atria: intoxication, hypoxia (oxygen starvation) of the myocardium).
For any of the reasons described above, electrical impulses begin to appear chaotically in the atria. Abnormal electrical activity causes the muscle fibers of the atria to contract erratically, called fibrillation. Atrial fibrillation looks like twitching of the atrial muscle bundles separately, “in discord.” Because of this, the atrium does not contract completely. For this reason, the phase of active blood ejection from the atria is disrupted (cardiac output decreases).
As a result of these disorders, exercise tolerance decreases and symptoms of heart failure increase (shortness of breath, swelling of the legs, etc.). In the enlarged chambers of the heart, blood stagnates and thickens, thus forming blood clots that are life-threatening. Blood clots can enter the arteries of vital organs, such as the brain, and clog them - increasing the risk of thromboembolism.
Unlimited certificate
In certain situations, re-examination is canceled for disabled people. The ITU body issues a certificate of lifelong disability. This is possible with the following diagnoses:
- oncological diseases with metastases;
- inoperable neoplasms in the brain (brain and spinal column), leading to disruption of the functioning of organs and systems;
- blindness, deafness, deaf-blindness that cannot be cured;
- amputation of arms, legs, important joints;
- limb deformities that cannot be corrected;
- dementia;
- degenerative conditions of the cerebral cortex;
- progressive pathologies;
- diseases of the central nervous system;
- chromosomal abnormalities (including Down syndrome);
- cerebral palsy;
- schizophrenia;
- liver cirrhosis, etc.
Read more: What exams do you need to take to become a lawyer
? Hint: an unlimited certificate until April 2020 was issued within two years from the date of the initial determination of violations. In April of this year, a new Decree of the Government of the Russian Federation was issued, according to which the indefiniteness of disability can be confirmed during an initial medical examination. Including for children, including the correspondence form of ITU.
The full register of violations is given in government resolution No. 247 of 04/07/2008. In addition, the document contains a list of criteria for the appointment of a lifelong group. You should know that the following can count on relaxation in this matter:
- pensioners and citizens of pre-retirement age;
- minor patients;
- military personnel injured during military operations.
Download for viewing and printing:
What are the types of atrial fibrillation?
Pathology differs in frequency of contractions:
- The bradysystolic form develops when an insufficient number of impulses pass to the ventricles. Then the frequency of ventricular contractions is less than 60 minutes;
- normosystolic – from 60 to 90 contractions per minute;
- tachysystolic form is the most common; There is a high frequency of contractions of the ventricles of the heart (over 90 minutes).
MA is also divided according to the nature and duration of attacks.
- Paroxysmal (attack-like) form – spontaneously stopping. The attack lasts less than 7 days (usually less than 24 hours).
- Persistent form – does not stop spontaneously. An attack of arrhythmia lasts more than 7 days. At the same time, stopping an attack with drugs or electrical cardioversion does not affect the diagnosis (form). The persistent form may be the first manifestation of arrhythmia or the result of repeated attacks of the paroxysmal form.
- Permanent form - drug therapy, electrical cardioversion are ineffective (or were not performed).
How does atrial fibrillation manifest?
Atrial fibrillation often may not reveal itself in any way. The most common symptoms are palpitations, shortness of breath, chest pain, dizziness, weakness or fainting. Sometimes these manifestations are combined with increased frequency of urination. Fainting and angina are much less common symptoms of atrial fibrillation.
On clinical examination, an irregular pulse is noted; There is a continuous fluctuation in blood pressure values. In most cases, the pulse is frequent (with a tachysystolic form).
More often, an attack of atrial fibrillation occurs for no apparent reason; less often it is associated with alcohol abuse, strong coffee, smoking, stress, and excessive physical activity.
How to treat atrial fibrillation?
Atrial fibrillation is difficult to treat. Drug therapy is aimed at correcting atrial rhythm and preventing attacks.
The following drugs are used: quinidine (quinipek, kinylentine, kinitard), procainamide (novocainamide), propafenone (propanorm, propastad, profenan), esmolol (breviblok), metoprolol (vasocardin, corvitol, metolol), propranolol (anaprilin, prolol, obzidan), amiodarone (aldarone, sedacorone, cardiodarone), sotalol (darob, loritmic, sotahexal), diltiazem (diazem, diacordin, Herbesser), verapamil (isoptin, veramil, danistol), digoxin (dilanacin, lanicor), korglykon (lily of the valley leaf glycoside), as well as many other drugs of different groups.
To prevent thrombosis, acetylsalicylic acid (aspirin) is prescribed. To stop attacks of atrial fibrillation, electrical cardioversion is used - a current discharge synchronizes the atrial rhythm.
Therapy is prescribed taking into account the cause of the pathology and the patient’s condition. The dosage and method of administration of drugs (orally or intravenously) depend on the form of atrial fibrillation. Invasive (surgical) treatment is also carried out.
TREATMENT
Drug treatment
Group I (membrane stabilizing agents) A: quinidine, novocainamide, etc.; B: Lidocaine, diphenylhydantoin; C: ajmaline, ethmoznn, etacizin, allapinin. Group II (beta-blockers). Group III (drugs that slow down repolarization): amiodarone, bretylium tosylate. Group IV (calcium antagonists): verapamil, nifedipine.
Read more: Coap failure to comply with the order within the prescribed period
Any antiarrhythmic drug can cause both antiarrhythmic and arrhythmogenic effects. The probability of an antiarrhythmic effect for most drugs is on average 50% and very rarely, only in a few clinical forms of arrhythmias, reaches 90-100%: a) relief of reciprocal atrioventricular tachycardia using intravenous administration of ATP, adenosine or verapamil; b) relief and prevention of paroxysmal tachycardia with complexes such as right bundle branch block and sharp deviations of the heart axis to the left with the help of verapamil; c) elimination of ventricular extrasystole with etacizine, flecainide.
In all other cases, the selection of antiarrhythmic therapy will be done by trial and error. In this case, the probability of an arrhythmogenic effect is on average 10%, in some cases life-threatening for the patient. The more severe the rhythm disturbances and the degree of myocardial damage, the higher the risk of an arrhythmogenic effect. Therefore, at present, most researchers believe that for asymptomatic and low-symptomatic arrhythmias, as a rule, the prescription of antiarrhythmic drugs is not required (A. S. Smetnen et al., 1993).
If drug therapy is necessary, the selection of antiarrhythmic drugs is based on the nature of the rhythm disturbance.
Supraventricular rhythm disturbances
1. Acute (extrasystole, paroxysmal atrial fibrillation, atrial flutter): procainamide, quinidine; (paroxysmal tachycardia): physical methods, isoptin, ATP, beta-blockers. 2. Prevention of paroxysms: cordarone, quinidine, beta-blockers.
1. Acute (extrasystole, paroxysmal tachycardia, fibrillation): lidocaine, nonocainamnd, etacizium, cordarone. 2. Prevention of paroxysms: cordarone, quinidine, diphenylhydantoin, novocainamide.
1. WPW syndrome: cordarone, ethmozin, gilurythmal (ajmalin). Contraindicated: cardiac glycosides and partially isoptic. 2. Sick sinus syndrome: rhythmylene, quinidine (under control of sinus node activity).
Non-drug treatments
1. Electrical defibrillation. 2. Electrical stimulation of the heart.
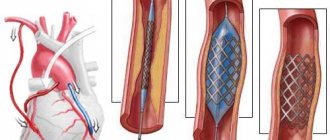
Surgery
1. Intersection of additional pathways. 2. Removal, destruction or isolation of arrhythmogenic foci in the heart. 3. Cardiac stimulation (permanent, temporary). 4. Destruction of the atrioventricular node with implantation of a pacemaker.
Why is atrial fibrillation dangerous?
Fainting is an alarming symptom that usually indicates sinus node dysfunction or an obstruction to blood flow (aortic valve stenosis, hypertrophic cardiomyopathy, cerebrovascular disease, etc.). It may also be complicated by an attack of angina pectoris or pulmonary edema. The main danger is an increased risk of stroke due to thromboembolism.
Atrial fibrillation is the most common cause of severe heart rhythm disturbances, often leading to disability or death. The life expectancy of patients with this pathology is sharply reduced; over a significant age interval, mortality doubles.
Related articles:
Mitral valve prolapse: causes, symptoms, diagnosis and treatment
What is mitral valve prolapse, its two forms: primary and secondary. Causes, types and characteristic symptoms of pathology. Diagnostics (ECG, EchoCG, X-ray) and treatment methods.
Diagnosis of the disease
To make a diagnosis of atrial fibrillation, the following examination methods are used:
- Initial examination, patient interview.
- Electrocardiogram (ECG).
- Daily recording of heart function indicators during the patient’s daily life - ECG and blood pressure monitoring.
- One of the monitoring options, in which a portable device transmits a signal over the phone in the event of an attack, is recording paroxysms in real time.
- Ultrasound - ultrasound examination of the heart and blood vessels.
To make a diagnosis of atrial fibrillation, it is enough to have patient complaints describing the characteristic symptoms, as well as an electrocardiogram that shows signs of atrial fibrillation.
However, to find out the true cause of the disease, it is necessary to conduct a thorough examination of the patient with all the necessary tests.
With the modern level of medicine, diagnosing atrial fibrillation is not difficult. In addition to the basic diagnostic methods, there are additional methods that allow you to obtain complete information about the condition of the patient’s heart, previous diseases and the general condition of the body. All this information is very important for prescribing the correct treatment.