Reasons for appearance
The mechanism of development of shortness of breath is due to the close relationship between the functioning of the cardiac and pulmonary systems.
Its pathogenesis is determined by a decrease in the volume of blood flowing from the left ventricle into the aorta, which provokes slow blood circulation in the lungs and causes disruption of gas exchange in the alveoli.
In heart failure, the heart is unable to maintain normal oxygen metabolism. Failure of ventilation capacity in the lungs creates favorable conditions for rapidly developing oxygen starvation (hypoxia). Our brain, in response to a threat, tries to compensate for the situation by activating the respiratory system, increasing the frequency of movements of the diaphragm.
The patient begins to take frequent and short breaths in and out, trying to restore the lack of oxygen. In a person with a healthy heart, this mechanism should equalize gas exchange, but in “heart patients” the opposite situation is observed.
Heart failure manifests itself in a decrease in ventricular contractility. If the pathology affects the left ventricle, then disturbances occur in the pulmonary circulation; if the right ventricle affects the systemic circulation.
Over time, the pathology acquires a combined form, exposing both ventricles to pathological changes, and passes into the chronic stage (CHF - chronic heart failure).
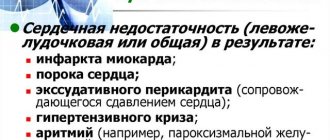
Impaired breathing (dyspnea) in heart failure can occur for a number of reasons:
- prolonged increase in blood pressure (arterial hypertension);
- lack of oxygen supplied to the heart muscle (coronary heart disease - IHD);
- defects in the structure of the heart, its valves and large vessels (heart disease, valvular disease, chronic aneurysm, mitral stenosis, mitral valve insufficiency);
- damage to the heart muscle of inflammatory origin (myocarditis);
- an increase in the thickness (hypertrophy) of the walls and expansion (dilatation) of the cavities of the heart (for example, with ischemic cardiomyopathy).
Symptoms and accompanying manifestations
All signs of the pathological process can be divided into those caused by increasing symptoms of respiratory failure and others that are explained by cardiac dysfunction.
There is no strict distinction; both factors play a role.
Asthenia
Constant fatigue. A person cannot perform daily duties at work and at home, he is lethargic and drowsy. Rest does not bring relief, strength is never restored.
The reason is a disruption in the normal saturation of the brain with blood. The body goes into a gentle mode of functioning, saving energy. As trophism is restored, the symptom recedes.
Actually shortness of breath or tachypnea
An increase in the number of movements to 20 or more per minute, more than usual. The body tries to improve gas exchange by increasing the amount of respiratory rate, but to no avail.
In the early stages of heart failure, the symptom manifests itself after intense physical activity (running 200 meters, climbing to the fifth floor without an elevator, and other options).
The bar is then lowered until the patient is gasping for air at complete rest. This is an indication of advanced heart failure (dystrophic stage of heart failure).
Decreased exercise tolerance
Gradual increase in intolerance to any mechanical activity. Unable to walk, work, or perform daily duties.
Total compensation for this disorder is difficult to achieve even with complex treatment. In the absence of an effect, the question of disability can be raised.
Arrhythmia
According to the type of sinus tachycardia. Develops as a result of insufficient gas exchange. Shortness of breath and palpitations are part of the same whole.
The body increases heart rate and respiratory rate to significant levels in order to somehow compensate for insufficient blood circulation in the brain. The effect, of course, is zero. Therefore, progression does not take long to occur.
As heart failure develops, more serious arrhythmias begin. Ventricular, atrial fibrillation, or extrasystoles. They can lead to sudden cardiac arrest.
Cerebral manifestations
Disorders of the central nervous system. In particular, dizziness and pain.
They occur first, immediately after the onset of shortness of breath. Because nervous tissues are very demanding on the amount of nutrition and react to the slightest disturbances.
Subjectively, the symptom manifests itself as an inability to navigate in space. The pain is observed in the back of the head, the crown of the head, and pulsates in time with the beat of the heart.
Loss of consciousness
Quite a late sign. Indicates severe heart failure. It can develop as a result of inadequate physical activity against the background of shortness of breath over 25 movements per minute.
Fainting is superficial and lasts no more than 3-5 minutes. They can be repeated several times over the course of one day.
Attention:
Syncope is considered an unfavorable prognostic sign because it indicates involvement of the brain in the pathological process. This means that acute ischemia—a stroke—is not far off.
Typical picture for heart failure of moderate degree and above. The man goes out and goes about his business. After several minutes, the number of breathing movements increases, there is not enough air, there is no satisfaction with the process.
The heart rate increases, a beat is felt, and pulsation is heard in the head. The eyes become dark, nausea develops, and weakness in the legs.
On the side, there is pallor of the skin and cyanosis of the nasolabial triangle. If you continue to move, you may faint. And so on for a long time until treatment begins.
Types of shortness of breath
Shortness of breath can be of two types - physiological and pathological.
Physiological shortness of breath is a natural response of the body to exercise. In a healthy person, it goes away after a couple of minutes of being at rest.
Pathological shortness of breath is characterized by the fact that it is observed even in the absence of any physical activity.
It is divided into the following types:
- Inspiratory - a person has difficulty breathing in. This type of shortness of breath can be caused by heart failure (so-called cardiac dyspnea), decreased patency of the trachea, bronchi or larynx as a result of their pathological narrowing. This condition occurs due to swelling of the mucous membranes of the airways, inflammation of the pleura - abnormalities in the structure of the respiratory organs, entry of a foreign object into the respiratory tract, etc.
- Expiratory - it is difficult for a person to exhale. This shortness of breath is caused by diseases that are accompanied by a narrowing of the diameter of the openings of the bronchioles (small bronchi). For example, asthma, bronchitis, chronic obstructive pulmonary disease, bronchiolitis and others.
- Mixed - manifests itself in difficulty in both inhalation and exhalation, detected in severe forms of cardiopulmonary diseases, such as acute respiratory failure and CHF.
Preventive actions
To avoid attacks of shortness of breath, you need to carefully monitor your health. Follow these guidelines:
- Try to avoid stressful situations, don’t worry about trifles.
- Give up bad habits. Smoking and drinking alcohol worsens the condition of the heart muscle.
- Do therapeutic exercises. Don't forget about breathing exercises that help saturate your blood with oxygen.
- Take more walks in the fresh air. Walking at a slow pace trains the heart muscle well.
If you notice the first signs of heart failure and shortness of breath, immediately seek help from a specialist.
Folk remedies show good results in the treatment of shortness of breath. But before use, make sure there are no contraindications.
Degrees of shortness of breath and its symptoms
The severity of shortness of breath will depend on the stage of heart failure.
The degree of shortness of breath is determined depending on the symptoms:
- Zero degree - shortness of breath occurs only during heavy physical exercise, restoration of normal breathing occurs after a short rest (physiological shortness of breath).
- The first (initial) degree is mild shortness of breath. Dyspnea occurs during physical activity, such as climbing stairs, brisk walking, and intense exercise.
- Second (medium) degree - difficulty breathing occurs during normal everyday physical and household activities; when walking, the patient is forced to make periodic stops. A person feels that he is moving slower than others, and when he tries to speed up, he feels that he does not have enough air.
- Third (severe) degree - normal walking causes significant discomfort, there is a need for frequent stops to restore breathing (every 2-3 minutes). The patient experiences a constant feeling of overwork and fatigue, the skin acquires a bluish tint, and there is pronounced swelling on the lower part of the lower leg.
- Fourth (extremely severe) degree – breathing is difficult even at rest, minimal physical activity is accompanied by a feeling of suffocation. A person finds himself unable to go outside or dress independently. The patient loses his ability to work, since even a slight load can cause an exacerbation. There is a significant decrease in the quality of sleep; staying in a horizontal position causes a deterioration in the condition, so patients are forced to sleep in a reclining or sitting position (orthopnea).
Shortness of breath due to allergies
Nasal congestion, causing expiratory dyspnea due to allergies, is quite common. In addition to taking medications, in such a situation, some remedies from folk wisdom can alleviate the condition.
- Bran
Bran shows good results in getting rid of shortness of breath. It is recommended to immediately drink a glass of purified water after waking up. After an hour, steam a tablespoon of bran with boiling water and eat it. You can have breakfast in 15-20 minutes.
- Birch tar
Birch tar effectively copes with allergic dyspnea. Start using it with one drop, dissolving it in half a glass of milk. Increase the portion daily drop by drop. Having reached 15 pieces, count down in the opposite direction. After a two-week break, the course is repeated.
- Herbal collection
Combine mint, chamomile inflorescences, string and sage herbs, viburnum flowers, observing the ratio 3:3:5:5:8. In the evening, pour a tablespoon of the plant mixture into a thermos and pour in 250 ml of boiling water. After eight hours, the infusion is filtered and divided into four servings, consumed until the evening.
Differences between cardiac and pulmonary dyspnea
Cardiac dyspnea has a number of characteristic signs:
- manifests itself when performing everyday habitual actions;
- a decrease in physical activity leads to a decrease in the severity of symptoms;
- it is characterized by difficulty in inhaling, in severe forms of heart failure - in inhaling and exhaling;
- the patient's condition worsens when lying on a horizontal surface;
- rapid heartbeat, coldness in the extremities, blueness of the nose, lips, fingers and toes;
- there is swelling in the ankle area;
- in the initial stages of deficiency, there is no sputum during coughing (“dry” cough).
The cause of shortness of breath, in addition to cardiovascular diseases, is also diseases of the bronchi and lungs. Specific symptoms of pulmonary dyspnea will depend on the type of pathology and its severity.
A common cause of pulmonary dyspnea is a violation of the normal patency of the bronchi as a result of their spasm, swelling or filling with liquid secretion secreted from the respiratory tract (sputum).
It has the following distinctive features:
- shortness of breath can have varying degrees of manifestation: on one day it may not exist, on another, on the contrary, it intensifies, up to a feeling of lack of air;
- has an expiratory form (difficulty in breathing is felt when exhaling);
- during exhalation, swollen veins protrude on the patient’s neck;
- “wet” cough, accompanied by sputum discharge;
- When you are nearby, you can hear dry wheezing and whistling as you exhale.
The main difference between pulmonary dyspnea and cardiac dyspnea is that the patient can tolerate being in a horizontal position without deteriorating well-being, the limbs remain warm, and there is no swelling in the legs.
Types of shortness of breath
Shortness of breath can be acute or chronic. Sudden difficulty breathing is caused by acute heart failure, which can develop with pulmonary embolism, myocardial infarction, or acute left ventricular failure. Most often, congestive heart failure leads to the development of chronic shortness of breath, the severity of which is determined by exercise tolerance.
The most common classification is the New York Heart Association classification:
| Class | Exercise tolerance |
| I | Regular physical activity does not cause shortness of breath |
| II | Normal activity causes shortness of breath |
| III | Little activity leads to shortness of breath |
| IV | Any physical activity causes difficulty breathing; shortness of breath at rest |
There is also the mMRC (modified Medical Research Council) dyspnea severity scale:
| 0 | Shortness of breath occurs only during heavy physical activity |
| 1 | Shortness of breath occurs when walking briskly on a level surface or with a slight rise |
| 2 | Due to shortness of breath, the patient walks slower than his peers; the patient must stop when walking on a level surface to catch his breath |
| 3 | The patient must stop to catch his breath after walking 100 m |
| 4 | Shortness of breath does not allow the patient to leave the house; it appears when dressing or undressing |
In addition, there are also:
- inspiratory dyspnea - difficulty breathing;
- expiratory shortness of breath - difficulty exhaling;
- mixed shortness of breath.
First aid for an attack
Providing emergency assistance should begin with calling an ambulance.
Before the doctors arrive, perform the following actions that can alleviate the patient’s condition:
- If the windows in the room are closed, then first open them to provide fresh air.
- Invite the patient to sit down, because in case of cardiac shortness of breath, a lying position will provoke an increase in symptoms and a deterioration in the general condition. The patient's feet should remain on the floor.
- Help loosen clothes, remove accessories that restrict the chest and abdomen (unfasten the top buttons, remove a belt, etc.).
- If the patient's hands and feet are cold, try warming them with a heating pad or any other container with hot water.
- Inhale using an oxygen cushion, if available (purchased at pharmacies and medical equipment stores). Disinfect the mouthpiece, make sure that the patient inhales the oxygen-air mixture through the mouth and exhales through the nose. The procedure is performed for 7-10 minutes, after which you can take a short break (10 minutes) and repeat the procedure again.
- Give the patient two tablets - Nitroglycerin (for resorption) and Furosemide. To normalize blood pressure, you can give an antihypertensive drug (Anaprylin, Carvedilol, Cardiofit).
When providing emergency care, it is important to be able to distinguish the symptoms of cardiac shortness of breath and cardiac cough from an attack of a pulmonary nature. The tactics for providing assistance in these two cases will be different.
With cardiac pathology, the patient begins to cough heavily and frequently, while experiencing pain on the right side under the rib. The nature of the cough is dry, suffocating, and during acute attacks it may be accompanied by bloody discharge and increased heartbeat. To relieve cough, mucolytics with a narcotic effect are prescribed - Codeine, Codipront, Hydrocodone or other antitussive drugs - Glaucin, Libexin, Sinekod.
The actions of emergency doctors are aimed at stopping an attack of cardiac shortness of breath with the help of medications, oxygen and the technique of applying venous tourniquets. Dopamine is administered to temporarily improve heart function.
The patient is also prescribed diuretics, their use reduces swelling and normalizes blood pressure. To prevent the development of pulmonary edema, medical workers apply venous tourniquets to the legs and right arm. Correct execution of this manipulation reduces the load on the heart, as it allows you to remove up to 2 liters of blood from the pulmonary circulation. In particularly difficult cases, oxygen inhalations are performed.
Shortness of breath with bronchitis (pulmonary)
A characteristic feature of pulmonary dyspnea is difficulty in exhaling, accompanied by whistling sounds in the chest area. Traditional methods practiced at home for this condition serve as an addition to the general treatment complex.
- Healing elixir
Article for you:
Treating allergies with folk remedies at home
Taking the following remedy can improve the condition even when severe dyspnea occurs, caused by bronchitis or other pulmonary pathology.
Wash 10 lemons, cut them and remove the seeds. Grind using a meat grinder. Remove the skins from 10 garlic heads. Turn them into a paste using a garlic press. In a glass jar combine the garlic and lemon mixture with a liter of honey.
After thorough kneading, keep for a week under a lid in the dark. Store in the refrigerator. Take 2 tbsp in the morning. l. elixir. You need to dissolve it slowly and then swallow it. Continue until all the healing paste is gone. The course is practiced twice a year.
- Horse chestnut tincture
You will need dried crushed horse chestnut inflorescences - 4 tsp. Transfer them to a glass vessel with 200 ml of vodka. The sealed container is kept in a dark cabinet for a week. After filtering, before breakfast and dinner, dissolve 30 drops of healing tincture in 150 ml of cooled boiling water and drink.
- Dill infusion
Dried, ground dill herb - 3 tbsp. l. steam with boiling water - 300 ml. Leave for 50-55 minutes under a linen napkin and strain using a sieve. Drink a glass of the healing drink every eight hours.
- Steam inhalation
Steam baths make breathing much easier. You will need to bring 2 liters of water to a boil. While stirring, add 4-5 drops of eucalyptus or peppermint ether. After five minutes, cover yourself with a blanket and carefully inhale the hot, beneficial vapors.
- Coltsfoot + marshmallow + oregano
Combine dry ground ingredients: oregano herb, coltsfoot foliage, marshmallow root in a ratio of 1:2:2. Soak a tablespoon of the mixture in 500 ml of boiling water for 20 minutes. After filtering, take 100 ml of healing liquid every eight hours.
Treatment methods
Treatment should be aimed primarily at eliminating the cause of shortness of breath, in this case it is heart failure.
Before prescribing a treatment regimen, the doctor must send the patient for a comprehensive examination, including: a blood test, electrocardiography, ultrasound examination of the cardiovascular system, and chest x-ray.
The results obtained should form the basis for choosing combination treatment tactics.
Drug therapy
Treatment of shortness of breath in heart failure with medications affects the cause that caused it. In addition, drug therapy is aimed at improving heart function and reducing the load on it.
Main groups of prescribed drugs:
- Cardiac glycosides - increase cardiac endurance, prevent the development of arrhythmia, improve exercise tolerance (Digoxin, Gitoxin, Adoniside).
- Beta-blockers - prevent the development of pathological changes in the heart, eliminate tachycardia, reduce electrical instability in the myocardium (Atenolol, Concor, Metoprolol).
- ACE inhibitors - prevent the development of CHF when used at the initial stage of the disease, dilate arteries and improve blood circulation (Captopril, Enalapril, Lisinopril).
- Diuretic drugs - help remove excess fluid from the body, reduce swelling and stagnation (Lasix, Furosemide, Britomar).
- Methylxanthines - as a prevention of repeated attacks of suffocation and increase the tone of the respiratory muscles (Euphylline, Theophylline, Euphyllong).
- Vasodilators - help relax the walls of blood vessels, have a pronounced vasodilating effect, improve tissue nutrition (Nitroglycerin, Molsidomin, Isosorbide mononitrate).
- Anticoagulants and antiplatelet agents - reduce blood viscosity, prevent the formation of blood clots (Curantil, Cardiomagnyl, Heparin, Fraxiparin, Warfarin, Aspirin).
Sprays and aerosols
For ischemic heart disease, acute heart failure or an attack of angina, aerosols for sublingual spraying are most effective, for example, Nitrospray, Nitromint, Izomint-spray.
These drugs belong to the medicinal group of nitrates. Their use in the form of an aerosol inhaler or spray significantly reduces the time for the onset of the therapeutic effect, and is only 30 seconds.
Nitrates improve coronary blood flow due to rapid dilation of blood vessels, reduce the load on the walls of the ventricles of the heart, and have a positive effect on the electrical capacity of the myocardium.
Carrying out the operation
Some conditions that cause heart failure can be treated with surgery.
The following methods are used for this:
- plastic and valve prosthetics;
- reconstructive operations on the left ventricle (geometric reconstruction, resection, cardiomyoplasty, etc.);
- installation of a pacemaker;
- elimination of congenital defects of the interventricular, interatrial septum and other congenital heart defects;
- As a last resort, a donor heart transplant is used.
Treatment of cardiac dyspnea
Dyspnea is a symptom of heart failure that disappears or improves with adequate drug therapy. How to treat shortness of breath in heart failure? Treatment of chronic heart failure has the following goals:
- Elimination of clinical manifestations of the disease;
- Slowing disease progression by protecting the heart and other target organs;
- Improved quality of life and prognosis;
- Reducing the frequency of hospitalizations.
Non-drug treatment helps to increase the effectiveness of drug therapy. Patients limit salt and liquid intake. Doctors recommend that patients who have shortness of breath and palpitations stop drinking alcohol and smoking, control their body weight, and weigh themselves daily. In case of slight shortness of breath and palpitations, rehabilitation specialists select a set of aerobic exercises that correspond to the functional abilities of the patients (until the heart rate reaches 70% of the submaximal one). If the symptoms of heart failure increase, stop training until the patient’s condition stabilizes.
How to get rid of shortness of breath in heart failure with the help of medications? The mainstay of treatment for heart failure is ACE inhibitors. Their use improves survival of patients with severe chronic heart failure and slows progression in earlier stages of the disease. For cardiac dyspnea, treatment with ACE inhibitor tablets begins with low doses, followed by a gradual increase in dose to the optimal one.
Angiotensin II receptor blockers are used for intolerance to ACE inhibitors. Diuretic therapy begins with loop diuretics. To avoid a dangerous decrease in potassium levels, doctors monitor its concentration in the blood. Potassium-sparing diuretics, when prescribed alone for heart failure, are too weak to relieve congestion and shortness of breath. In case of exacerbation of decompensation of chronic heart failure, spironolactone is used in high doses until compensation is achieved. After this, the dose of the drug is reduced. In patients receiving spironolactone and ACE inhibitors, doctors at the Yusupov Hospital must determine the concentration of potassium ions in the blood plasma.
Doctors begin treatment with cardiac glycosides (digoxin) in patients with clinically significant chronic heart failure after making sure that kidney function is not impaired and the electrolyte balance is normal. Use of this medicine for shortness of breath and rapid heartbeat reduces the severity of symptoms of heart failure. Patients who suffer from heart failure with rapid heartbeat and shortness of breath and who, according to echocardiography, have blood clots in the left ventricle, patients over 65 years of age with atrial fibrillation are given anticoagulant therapy with Varvarin. Acetylsalicylic acid preparations are prescribed to patients with coronary heart disease regardless of ejection fraction.
Inotropic agents transiently improve hemodynamics (increase contractility and cardiac output) and the clinical condition of patients with exacerbation of decompensation. With long-term follow-up, they increase the risk of death in patients with chronic heart failure. To increase low cardiac output, cardiologists use dopamine through intravenous infusions. If a patient has shortness of breath due to heart failure, aerosol medications do not help.
Cardiologists for chronic heart failure prescribe a new drug with metabolic action from the group of cytoprotectors - vasonate. It helps restore the energy balance of cardiomyocytes and reduce the accumulation of free fatty acids. Vasonate enhances myocardial contractility and increases resistance to physical stress.
For diastolic chronic heart failure, doctors prescribe diuretics, β-blockers, nitrates, ACE inhibitors and angiotensin II receptor blockers. In patients with diastolic heart failure, which developed against the background of hypertrophic cardiomyopathy, a reduction in symptoms (palpitations, shortness of breath) is achieved by prescribing verapamil.
If heart failure pills and drug infusions do not relieve shortness of breath, palpitations, and other symptoms of heart failure, the patient is offered surgery. Depending on the cause of the disease, cardiac surgeons at partner clinics perform the following operations:
- Elimination of valve defects;
- Placement of a pacemaker or cardioverter-defibrillator;
- Transplantation of artificial ventricles;
- Enveloping the heart with an elastic mesh frame;
- Heart transplantation.
To avoid the need for complex surgical interventions, if you have shortness of breath or rapid heartbeat, call the contact center or make an appointment with a cardiologist online. Doctors at the Yusupov Hospital, after a comprehensive examination, will individually select the best medicine for cardiac dyspnea and conduct complex therapy with modern drugs. Cardiologists will prescribe the best medications for shortness of breath and palpitations due to heart failure.
Author
What can you do at home?
It is quite possible to combat shortness of breath on your own at home if you approach this issue systematically and purposefully.
It is important to follow a diet, normalize weight, and limit the amount of fluid and salt consumed.
If you feel better during drug treatment, you must maintain moderate physical activity, do breathing exercises and physical therapy.
Breathing exercises and other exercises
Breathing exercises are a set of exercises aimed at increasing lung volume and improving gas exchange in tissues. Regular implementation can prevent the progression of respiratory disorders and improve blood supply to the heart muscle.
The ability to breathe correctly is an important part of preventing the development of attacks of shortness of breath.
Examples of some breathing exercises:
- Exhale deeply through your mouth, take a deep breath through your nose. Exhale deeply through your mouth again and draw in your stomach while holding your breath. Count to yourself to 10. After this, inhale through your mouth so that the air fills the abdominal cavity. Without exhaling the air from your stomach, draw it in and count to 10 again.
- Starting position - sitting or standing, bend your elbows, turn your palms up. Clench your fists 8-10 times and at the same time take short, intense breaths. Extend your arms and lower them down for 5-10 seconds. Repeat the exercise 15-20 times.
The muscles of the neck, shoulders and abdominal muscles actively participate in breathing movements.
The study of these zones can also normalize the processes of ventilation of the lungs and improve the supply of oxygen to the tissues of internal organs.
To do this, you can use the following exercises:
- Take a comfortable sitting position, making sure that your legs and arms are completely relaxed. Take a short breath and lift your shoulders up, tensing your upper torso muscles as much as possible. Hold your breath for a couple of seconds, as you exhale, lower your shoulders down and relax them. Complete 10 reps.
- Starting position - lying on the floor, legs bent at the knees, feet on the floor. As you exhale, tighten your abdominal muscles and lift your pelvis so that your back lifts slightly off the floor. As you inhale, return to the starting position. The number of repetitions is 5-15 times, depending on how you feel.
Folk remedies
Traditional medicine methods are often used to prevent attacks of cardiac dyspnea. They can really make the patient's breathing easier for a while.
Their strength is that folk remedies have virtually no side effects or contraindications, since they contain natural ingredients.
Lemon and garlic
A recipe for homemade medicine made from lemons and garlic is very popular.
To prepare it, you need to chop 7-10 lemons and the same number of heads of garlic, mix the resulting pulp with a kilogram of honey. The resulting product should be infused for 2-3 days, after which take it 30 minutes before the main meal, several teaspoons.
Aloe tincture
One of the simple and affordable remedies that effectively prevent attacks of cardiac cough with shortness of breath is an infusion of aloe leaves with vodka. The product should be infused for at least 10 days in a dark place, after which you can take one teaspoon along with honey. 10-15 minutes after administration, it is recommended to drink a mug of hot tea.
Lily of the valley tincture
An infusion of lily of the valley along with valerian, dill seeds and mint calms not only the nervous system, but is also an effective remedy for myocardial disorders. To prepare it, you need to mix a teaspoon of lily of the valley flowers, two teaspoons of dill and mint seeds, and three teaspoons of valerian. Pour the resulting mixture with a liter of boiling water, cover with a lid, and let it brew for an hour. After the infusion has cooled, strain it and take 50 grams at least 3 times a day.
Other herbs that help get rid of the disease include motherwort, cranberry leaves, licorice root, and yarrow.
Diet
The general principles of nutrition for patients with heart failure are to control the amount of table salt and liquid consumed. Recommended daily salt intake is up to 2 grams, liquid – up to 500 ml. Salt can be replaced with spices that have a beneficial effect on the heart - cardamom, nutmeg.
Nutrition should be varied and balanced. The daily menu should include lean meat, sea fish, vegetables, fruits and dried fruits.
Fatty, salty, smoked, semi-finished products, alcohol, sweet and flour products are prohibited.
Smoking is a habit that all patients suffering from any cardiovascular disease should eliminate first.
Beta blockers
Tablets from the beta blocker group are often used to relieve signs of heart failure, as well as arterial hypertension, tachycardia and arrhythmia.
They help reduce the myocardium's need for oxygen, causing it to contract less frequently. This eases the load on the muscle and helps normalize the functioning of the organ. In addition, medications lower blood pressure levels.
List of prescribed tablets
There are several drugs that are effective and help alleviate the disease:
- Anaprilin is a propranolol-based tablet that has a pronounced antiarrhythmic effect. Prescribed in courses of 1-3 weeks, you need to take 1 tablet 2-3 times a day, depending on the severity of the condition. The drug is not used for myocardial infarction, bronchial asthma, allergies. Cost – from 30 rubles.
- Betaloc is a beta-blocker based on metaprolol. It has antianginal, antiarrhythmic and hypotensive effects. Not prescribed for hypotension and bradycardia, in the acute period of myocardial infarction. The daily norm is 2-3 tablets, they must be taken for 2-4 weeks. The price of the product is from 140 rubles.
- Vasocardin - another remedy in the form of tablets based on metoprolol. The patient is prescribed 1 tablet 3 times a day for 3 weeks. The drug is contraindicated in case of allergies to its components, atrioventricular block, myocardial infarction. Its cost is approximately 60-80 rubles.
It is not recommended to take such medications without first consulting a doctor.
Possible complications
An attack of cardiac dyspnea is dangerous due to complications that arise if its development is not prevented in time.
A state of acute suffocation can provoke the following life-threatening disorders:
- stagnation of blood in the pulmonary circulation (cardiac asthma);
- blocking of the pulmonary artery or its branches by an embolus (pulmonary embolism);
- arrest of coronary blood flow (asthmatic form of myocardial infarction);
- disruption of the outflow of blood and lymph in the pulmonary circulation and their penetration into the pulmonary alveoli (pulmonary edema).
Reasons for development
The main factor in the development of cardiac dyspnea is a drop in systole intensity. This is a symptom of many pathologies. In heart failure, it is most often provoked by:
The effect of hypertension on human organs.
- hypertension;
- IHD from angina pectoris to myocardial infarction;
- valve defects, congenital or acquired;
- cardiomyopathy;
- myocarditis;
- dilatation;
- toxic effects, including alcohol;
- endocrine pathologies.
The appearance of shortness of breath always indicates the progression of cardiac disorders.
Forecast
The prognosis for treatment of shortness of breath will depend on the form of heart failure, its stage and the person’s age. Most often, its very appearance already signals that the body is working at the limit of its capabilities.
Heart failure is a difficult condition to treat; in its final stages, it can only be cured by heart transplantation.
It is quite difficult for elderly people to undergo such heart operations, so the prognosis is more favorable in cases of detection and treatment of pathology at a young age.
The prognosis for recovery after surgical treatment is influenced by a person’s lifestyle, compliance with the course of drug therapy, and timely completion of periodic examinations.
Author of the article: Yulia Dmitrieva (Sych) - In 2014, she graduated with honors from Saratov State Medical University named after V. I. Razumovsky. Currently working as a cardiologist at the 8th City Clinical Hospital in the 1st clinic.
Cardiac glycosides
Drugs in this group are used for arrhythmia and tachycardia, as well as any form of heart failure. They are prescribed in the post-infarction period for some patients, as well as for angina pectoris.
Medicines are in most cases of natural origin, since they contain extracts from medicinal plants. The drugs relieve acute symptoms of heart failure, as well as kidney disorders.
List of prescribed tablets
Several medications are used to treat heart failure:
| Name and composition | Peculiarities | Price |
| Digoxin (contains the active ingredient of the same name, which is an extract from foxglove woolly) | The tablets are taken in courses of 2-3 weeks; if necessary, the patient uses them on an ongoing basis. The daily dose is 1 tablet, which is best taken in the morning. Do not use the medication if you are allergic to its components, have severe bradycardia, or have atrioventricular block. | The price starts from 50 rubles. per package |
| Celanide (contains lanatoside) | The product is available in the form of tablets for oral administration, the daily dose is 1 tablet; they must be taken in courses of 2-4 weeks or on an ongoing basis, depending on the severity of the condition. Tablets are contraindicated in cases of intolerance to the components, severe hypotension and bradycardia. | The price is approximately 50-90 rubles. |
| Novodigal (contains digoxin) | The tablets have a cardiotonic effect. Not used for chronic hypotension and bradycardia, in the first few weeks after myocardial infarction. The dosage is determined individually; usually the patient is prescribed 1-2 tablets per day for 3 weeks. | The price starts from 60 rubles. per package |
Each medication is also available in the form of a solution for intramuscular administration, but the tablet form is more convenient for home use.
Shortness of breath during the heat
The appearance of a feeling of acute lack of weather while being under the hot sun leads to dyspnea. It is necessary to establish the cause of this phenomenon by contacting a doctor. You can use some remedies practiced in alternative treatment.
- Melissa + chamomile
Place dried crushed raw materials in a heat-resistant bowl: chamomile flower baskets and lemon balm herb - 2 tbsp. l. Brew with boiled water - 450 ml. Wrap tightly with a warm scarf. After 55-60 minutes, the infused liquid is filtered. Add fresh lemon juice - 3 tbsp. spoons. The resulting volume of the medicinal product is drunk per day in three doses.
Shortness of breath, causing a person to suddenly stop and rest, can occur for various reasons. Before resorting to effective folk methods, you should consult a doctor who will help clarify the factor that triggered the appearance of suffocation. Any herbal components are analyzed to identify any contraindications.