Types of WPW syndrome
A type WPW
- the spatial vector of the electrical axis of the heart is directed to the right
- maximum QRS complex in leads II, III, aVF
- in leads I, aVL the delta wave can be negative
- in leads V1, V2 there are signs of hypertrophy or blockade of the right bundle branch
B type WPW
- the electrical axis of the heart is directed to the left
- maximum QRS complex in leads I, aVL
- in leads II, III, aVF QS complex (QRS type)
- maximum QRS complex with a positive delta wave in leads V5, V6
AB type WPW
- According to standard leads, the axis is deviated to the left
- along the chest leads - right bundle branch block
All these types may change from time to time.
Fig.1. Delta wave formation in WPW syndrome
Antidromic tachycardia
This rhythm disorder has been poorly studied to date, which is due to the low incidence of the disease. Only in 8% of patients diagnosed with WPW syndrome, antidromic tachycardia is additionally detected. Whether this condition is dangerous can be said for sure after a complete examination of the patient.
Antidromic tachycardia is much less common than orthodromic tachycardia. Its occurrence is mainly associated with Wolff-Parkinson-White syndrome (WPW syndrome), a congenital anomaly characterized by the presence of an additional conduction pathway. It is this pathway that underlies the occurrence of antidromic tachycardia.
In the absence of WPW syndrome, such supraventricular tachycardias are diagnosed in almost 90% of cases. such as atrioventricular-nodal reciprocal tachycardia and orthodromic tachycardia, combined with a hidden additional conduction pathway.
WPW (Wolff-Parkinson-White Syndrome) Animation Video
Description of antidromic tachycardia
Paroxysmal atrial tachycardia, which includes the antidromic form of rhythm disturbance, is associated in its appearance with the re-entry mechanism - the re-entry of the excitation wave.
The circulation of the impulse mainly passes through a closed circuit located inside the atrioventricular node or sinus node.
Secondary channels for conducting the excitation wave, called bundles of Kent, which are normally absent, can also form between the atria and ventricles.
Additional pathways for conducting impulses can be hidden, and then the resulting tachycardia is designated as orthodromic. It is also possible that additional pathways may be clearly manifested, that is, easily diagnosed by ECG. Such formation is characteristic of WPW syndrome, in which both orthodromic and antidromic tachycardia occur.
The circulation of the excitation wave during antidromic tachycardia passes along the contour of the atrium - an additional conduction path - the ventricles - the atrioventricular node - the atria.
The relatively rare occurrence of antidromic tachycardia is associated with the fact that the excitation wave passes through the atrioventricular node much more slowly in the orthodromic direction. This creates favorable conditions for launching the re-entry mechanism.
The presence of several bundles of Kent contributes to the occurrence of orthodromic and antidromic tachycardia simultaneously in one patient.
In WPW syndrome, several additional pathways may be detected that form the basis for the formation of preexcited tachycardia.
With this form of rhythm disturbance, anterograde and retrograde conduction of impulses is observed.
Often, preexcited and antidromic tachycardia are considered the same disease, since there are no obvious differences in ECG signs and the treatment tactics are almost the same.
Symptoms of antidromic tachycardia
The occurrence of the disease is not associated with age, so it can be detected even in newborns. A frequent trigger for the development of pathology is any disorder of atrioventricular conduction. These may be blockades or extrasystoles.
During paroxysms of tachycardia, especially when they occur frequently, hemodynamics inside the heart are disrupted. This disorder negatively affects the condition of the heart chambers, which expand and begin to contract with insufficient force.
The clinical picture of tachycardia depends on a number of factors: the duration of the rhythm disturbance, the frequency of its occurrence, and the presence of additional cardiac pathologies. In itself, antidromic tachycardia in WPW syndrome is not dangerous, but with a significant disturbance of hemodynamics, life-threatening tachyarrhythmias can develop against its background - fibrillation, ventricular/atrial flutter.
Causes of antidromic tachycardia
The main cause of the development of antidromic tachycardia is WPW syndrome, which is a hereditary heart pathology. Moreover, the severity of the syndrome often depends on the presence and number of additional pathways called bundles of Kent. A wave of excitation passes through them, bypassing the atrioventricular node.
The Kent bundle is an abnormal formation of myocardial conductive fibers found between the ventricles and atria. It was discovered by the English physiologist Kent.
From a biochemical point of view, the development of WPW syndrome, and in particular antidromic tachycardia, is associated with gene mutations.
Diagnosis of antidromic tachycardia
The electrocardiogram reveals wide, deformed ventricular complexes, as opposed to the narrow QRS, which are formed during orthodromic tachycardia. In this case, P waves behind the wide ventricular complexes are practically not detected.
The occurrence of tachyarrhythmia in normal cases is preceded by atrial extrasystole.
A feature of antidromic tachycardia is the detection of a pronounced delta wave on the ECG. There are also other signs reminiscent of ventricular tachycardia. Such characteristics are due to the fact that the ventricles are excited by the passage of an impulse along additional pathways.
Treatment and prevention of antidromic tachycardia
For this pathology, drug therapy is primarily prescribed, which includes the following drugs:
- sotalol;
- procainamide;
- quinidine;
- digoxin;
- mexiletine;
- adenosine;
- verapamil.
It is not recommended to use drugs from the following groups of arrhythmics in the treatment of antidromic tachycardia: cardiac glycosides, beta-blockers, calcium channel blockers. This is due to the fact that they can increase the refractory period and thereby worsen the patient's condition by increasing the heart rate.
The ineffectiveness of drug treatment is an indication for catheter ablation, during which additional pathways are crossed.
Prevention consists of preventing the development of attacks of tachycardia, for which the same medications or more radical surgical treatment methods are used.
Source: https://arrhythmia.center/antidromnaya-tahikardiya/
Clinical forms of WPW syndrome
- The manifesting form - the accessory pathway can function both anterograde and retrograde. The Kent beam works most often.
- Intermittent form - characterized by periodic signs of pre-excitation.
- Hidden variant of WPW - accessory pathways are retrogradely conductive, due to longer refractory conduction in them. But sometimes retrograde pathways can be slow retrograde conductors instead of fast ones.
- Latent form of WPW - occurs during electrical stimulation of the atria.
Causes
Reciprocal tachycardia occurs against the background of improper formation of the AV node during fetal development. Normally, a single connection is formed, but due to genetic abnormalities, two channels are formed through which electrical impulses pass. As a rule, impulses travel along the fast path, but under the influence of certain factors, impulse conduction occurs through the slow path.
As a result, the ventricular fibers have time to receive only impulses passing through the fast channel, and slowly passing impulses return to the atrium. Thus, a reciprocal reaction (return) occurs, which provokes an increase in heart rate.
Other causes and predisposing factors include:
- various heart rhythm disturbances (atrial extrasystole, sinus tachycardia);
- sinoatrial blockade (referred to as weak joint syndrome);
- frequent stress, nervous strain, conflict situations, depression;
- smoking cigarettes, drinking alcohol, taking drugs;
- heavy physical activity (often associated with professional activities);
- male gender (paroxysmal attacks are several times more common in men).
Classification of additional paths
- AV connection (right, left, bilateral), bundle of Kent
- Nodoventricular junction (connects the distal part of the AV node with the interventricular septum), Macheim fibers.
- Fasciculoventricular connection - the trunk of the His bundle with the contractile myocardium, Maheim and Lev fibers.
- The atriofascicular tract is the connection of the right atrium with the trunk of the His bundle. Brashen-Moshe tract.
- The atrionodal tract is the posterior internodal tract of James. Connects the sinus node with the distal part of the AV node with the NH zone.
At nodoventricular junction
- PR interval - normal (0.12-0.20 sec)
- there is no delta wave or there is only a hint of it
- QRS complex normal
Fasciculoventricular variant of ventricular preexcitation
- PR interval - normal
- delta wave maybe
- The QRS complex is slightly widened
Short PR interval syndrome
- the atrionodal and atriofascicular tracts function
- PR interval ≤0.11 sec
- no delta wave
- There are no secondary repolarization processes
Fig.2. ECG for WPW syndrome.
SVC syndrome on the electrocardiogram
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day.
Wolff-Parkinson-White syndrome is a commonly diagnosed condition characterized by premature excitation of the ventricles of the heart muscle. The mechanism of development of the disease is associated with the presence of an additional muscle bundle in the heart, which is called the bundle of Kent. Because of this, an additional path for electrical impulses appears in the organ. The course of the pathology is similar to the manifestations of various heart diseases. In men, SVC syndrome is diagnosed more often than in women.
Our readers successfully use ReCardio to treat hypertension. Seeing how popular this product is, we decided to bring it to your attention. Read more here...
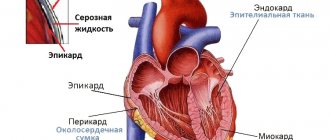
Development mechanism
The human heart has the ability to contract independently after a certain period of time. This is ensured by the passage of electrical signals through the organ. In a healthy person, electrical impulses pass through the components of the conduction system of the heart. Normally, these are the sinoatrial node, the His bundle, the atrioventricular node and Purkinje fibers.
Read also: Running with tachycardia
With SVC syndrome, a person has an additional pathway for the conduction of electrical impulses - the Kent bundle. With this pathology, excitation occurs, as in healthy people, in the region of the sinus node, but spreads along the above-mentioned bundle of Kent. As a result, ventricular excitation occurs faster and earlier than when impulses pass through normal pathways. This process in medical practice is called premature excitation of the ventricles. Following this, the rest of the ventricle is excited by impulses that have passed through normal pathways.
Why is this happening
SVC syndrome is a congenital disease. It is believed that genetic predisposition is one of the main reasons for the development of the disease. In many patients, in combination with SVC, other pathologies of cardiac muscle development are diagnosed. This may be mitral valve prolapse, cardiac tissue dysplasia or Marfan syndrome, congenital defect Tetralogy of Fallot and some other diseases.
The causes of disruption of the intrauterine formation of the fetal heart include factors that negatively affect the course of pregnancy. This includes bad habits, drug use, stress, poor diet, etc.
SVC syndrome on ECG
SVC syndrome is reflected on the ECG as an additional wave of depolarization (delta wave). The cardiogram shows that the PQ interval has a shorter distance, and the QRS complex interval, on the contrary, lengthens. When a premature impulse collides with a signal that has passed to the ventricle along the normal path, a QRS complex is recorded on the cardiogram; it becomes deformed and becomes wider. In addition, there is a change in the polarity of the T wave and a displacement of the RS-T segment.
What is the difference between the phenomenon and the syndrome of SVC
According to the classification of the World Health Organization, it is customary to distinguish between the syndrome and the phenomenon of SVC. The phenomenon is a pathology during which the electrical impulses of the heart spread to the ventricles, but this is not accompanied by any clinical manifestations in the patient. The syndrome is considered to be a state of premature excitation of the ventricles through the accessory node of Kent in combination with symptoms characteristic of the pathology. In the first case, no specific treatment is required. All a person needs to do is register with a hospital and undergo regular preventive examinations. If SVC syndrome is diagnosed, the patient may require drug therapy.
Classification
Depending on the location of the additional muscle node, the following forms of pathology are distinguished:
- type A. Here the bundle is localized between the left ventricle and the left atrium. Contraction of the left ventricle occurs earlier than when electronic impulses pass through the normal conduction path;
- type B. The bundle is located in the region of the right atrium and right ventricle, respectively, premature excitation is observed in the right part of the organ.
Sometimes a mixed type occurs, when there is a right and left accessory pathway in the heart.
According to the nature of the course, the disease has the following variations:
- manifesting type - characterized by the constant presence of a delta wave on the ECG, a sinus heart rate, frequent attacks of increased heart rate;
- intermittent - here there is verified tachycardia, sinus heart rhythm, delta waves with a transient nature;
- retrograde - the syndrome does not manifest itself in any way on the ECG, the patient has a slight tachycardia.
SVC syndrome is especially dangerous if a person has a predisposition to atrial flutter or fibrillation.
How does pathology manifest itself?
Despite the fact that SVC syndrome is a congenital disease, it can be diagnosed at any age. Most often, the disease is detected between the ages of 10 and 20 years; in elderly patients, cases of detection of the syndrome are extremely rare. Pathology can be latent for a long time without manifesting itself. The most common symptom of the disease is paroxysmal arrhythmia. This symptom is more common in men with SVC at the age of 20 years and in women during pregnancy.
In young children, SVC syndrome often provokes attacks of paroxysmal tachycardia, which is accompanied by a sudden increase in heart rate. The heart rate reaches more than 100 beats. The attack disappears as suddenly as it appeared. When tachycardia occurs, the baby becomes anxious, cries, and sometimes has difficulty breathing. Teenagers tolerate this symptom more easily. At school age, children experience attacks of tachycardia with a heart rate above 200 beats per minute. The reason for this is physical activity and strong emotional experiences.
More often, an attack of tachycardia lasts 2–3 minutes, but often its duration is several hours. In this case, the patient experiences the following symptoms:
- nagging pain in the heart area;
- prostration;
- dizziness, headache;
- tinnitus and lack of air;
- cold sweat and cyanosis of the dermis;
- drop in pressure, cyanosis of the fingers and nasolabial triangle.
Read also: Tachycardia after eating causes
Tachycardia, as a rule, goes away on its own, but in some cases it may be necessary to take stabilizing medications.
Important! In severe cases of SVC syndrome, the patient is assigned disability group II.
Degrees of the disease
Premature ventricular contraction syndrome can occur in various forms. The following options are available:
- latent course without any manifestations – observed in 40% of all patients;
- mild form - the disease rarely makes itself felt, attacks of tachycardia are short-lived and go away on their own without medical intervention;
- moderate severity - here attacks of cardiac arrhythmia last up to 3 hours, the patient requires medication;
- severe course - attacks of tachycardia are prolonged, it is quite difficult to stop them with medication, the patient requires hospitalization.
People with severe disease require surgical treatment. If radical measures are not taken in a timely manner, death occurs.
Diagnosis of SVC syndrome
To diagnose pathology, 12-lead electrocardiography is used. In addition, the patient's heart rate is measured. In some patients, the number of beats exceeds 220, sometimes the frequency reaches the upper limit - 360 beats per minute.
To obtain more accurate data, the patient is prescribed transesophageal cardiac pacing. The method involves inserting and attaching an electrode through the esophagus, which forces the heart muscle to contract in a certain rhythm. When the contraction frequency is 150 beats, cessation of the Kent beam is diagnosed. This proves the presence of additional cardiac conduction pathways.
To get an overall picture, the following methods are used:
- endocardial electrophysiological study - helps to identify the area and number of pathological pathways by inserting a catheter into the veins through the muscles;
- ultrasound examination of the heart with assessment of blood flow in the veins and vessels;
- daily monitoring – assessment of the functioning of the heart muscle throughout the day with a comparative analysis of the data obtained.
Treatment methods
Treatment of the disease depends on the severity, progression and clinical manifestations of a particular patient. It is imperative to take into account whether the symptom has caused a complication such as heart failure. If there are no symptoms, treatment is not carried out. Such patients are prescribed an annual examination. Among pilots, military personnel and representatives of other dangerous professions, heart examinations are performed more often.
Patients suffering from arrhythmia, hypotension, and increasing symptoms of heart failure are prescribed antiarrhythmic drugs. Medicines are taken throughout life. It is possible to use these drugs for prophylactic purposes. To relieve an attack of arrhythmia, vagal tests are used. Using these techniques, it is possible to stimulate the vagus nerve and relieve an attack of tachycardia. When a rhythm disturbance occurs, a person needs to perform the following actions:
- take a deep breath, hold your breath, exhale with slight straining (Valsalva maneuver);
- close your nostrils with your fingers and try to inhale through your nose (Müller test);
- wash with cool water, while holding your breath;
- massage the sinus node located in the neck.
In severe cases, atrial fibrillation is used, with the help of which the heart rhythm is restored. It is possible to completely get rid of SVC syndrome using radiofrequency ablation. The method involves the destruction of an additional pathway using cauterization. The operation is performed in patients with severe pathology, but sometimes the method is used among people who tolerate attacks of tachycardia well.
Another type of surgery is catheter ablation. This is a minimally invasive technique that rarely causes complications and allows you to get rid of pathology in more than 90% of cases. Re-development of tachycardia occurs when the Kent node is incompletely destroyed or if one node was eliminated, and the patient had two of them.
Prognosis and prevention for the patient
With an asymptomatic course of the pathology, the prognosis for the patient is usually favorable. Among people with frequent attacks of angina, it will depend entirely on the correctness and speed of stopping the attack. People with severe SVC syndrome are advised to undergo surgical intervention, which more often gives a positive result, allows them to get rid of the disease and lead a full life.
Prevention methods include creating favorable conditions for bearing a fetus, giving up bad habits, adequately assessing stress, and proper nutrition. Secondary prevention involves strict adherence to doctor’s recommendations, timely intake of medications, and regular visits to a specialist.
Read also: Heart disease tachycardia
Paroxysmal tachycardia due to WPW
- Paroxysmal reentrant AV tachycardia accounts for more than 80% of cases
- Atrial fibrillation 15%, flutter - 5%
- Combination of reentrant AV tachycardia and atrial fibrillation/flutter
- 0.2% sudden death
Paroxysmal reciprocal AV tachycardia with longitudinal division of the AV node into 2 electrophysiological channels - normal and unusual types.
Mechanism of development of AV nodal reciprocal tachycardia
Sloy Fast - the presence of tachycardia with narrow QRS complexes, supraventricular tachycardia, RR are the same, frequency is 150-180 or more pulses per minute.
Signs
- P wave behind the QRS complex
- RP' interval is short, 90 ms or less
- PR interval is long
- RP less than 50% of RR
Fig.3. Formation of delta waves in WPW syndrome.
Atypical reciprocal AV tachycardia
or fast-slow reciprocal AV tachycardia
- first the impulse goes along the B-path, then along the a-path
- RP>1/2 of RR
- RP>PR
- RP>90 ms
Causes and mechanisms of occurrence
Etiological factors are divided into two groups:
- congenital - these include Wolff-Parkinson-White syndrome;
- acquired - diseases suffered by the patient during his life and contributing to the development of reciprocal tachycardia (myocarditis, etc.).
The heartbeat increases in this case due to the presence in the atrioventricular node of two types of electrical impulse conduction, which are interconnected (the phenomenon of longitudinal dissociation of the AV connection). They are called the “fast” or beta path, and the “slow” - alpha path.
A specific start is the occurrence of spontaneous extrasystole (extraordinary contraction of the heart). In this case, the first of the paths should not be ready to receive the signal (refractory state). Thus, AV conduction will be carried out along the alpha beam. Along the “fast” tract that has emerged from rest, the excitation wave travels in the opposite direction and merges with the first one. Subsequently, they circulate in the AV junction, and the re-entry circuit (circular movement of the impulse) is closed.
Orthodromic tachycardia
Signs
- narrow QRS complex, RP interval is the same
- frequency 180-250 per minute
- Retrograde activation of the atria occurs, therefore:
- discrete negative P wave in leads II, III, aVF
—RP-P'R
— RP — 100 ms or more
— RP<50% RR
Accessory pathways are retrograde conducting.
When an extrasystole occurs, the extrasystolic impulse tries to travel through the accessory pathway and the AV junction. It is not possible to pass through the accessory pathway, so it is carried out through the AV node. As a result, a QRS complex occurs. Next, the extrasystolic impulse finds the accessory pathway functioning in the retrograde direction. Retrogradely excites the atria, so the P wave appears behind the QRS complex. The extrasystolic impulse returns to the AV node. And if the AV node has left the refractory period, then a circular rhythm occurs with anterograde conduction through the AV connection, retrograde along the accessory pathway.
Orthodromic reciprocal AV tachycardia occurs. Orthodromic means that it passes through the AV junction, reciprocal means that it passes through the accessory pathway. Tachycardia looks like Sloy-Fast.
Fig.4. Delta wave in WPW syndrome.
Reciprocal tachycardia involving additional pathways
annotation
The nature of anterograde conduction of excitation along the AV junction and accessory pathways in patients with WPW syndrome and orthodromic AV tachycardia was determined. The influence of types of AV conduction and other electrophysiological parameters on the possibility of initiation of tachycardia paroxysms and their stability is discussed.
Paroxysmal reciprocal atrioventricular tachycardias account for 75 to 85% of all paroxysmal supraventricular tachycardias [4] and include paroxysmal reciprocal atrioventricular (AV) nodal tachycardia PRUT) and paroxysmal reciprocal AV orthodromic tachycardia (PROAVT) with the participation of additional conductors ways (DPP).
Orthodromic tachycardias with narrow QRS complexes occur in cases where anterograde conduction of excitation is carried out through the AV junction, and retrograde conduction is carried out either through one of the channels of the AV node, or through abnormal pathways - in manifesting, latent or latent WPW syndromes [7]. In antidromic tachycardias with wide QRS complexes, anterograde conduction of excitation occurs through the AP, and retrograde conduction occurs through the AV junction or paraseptal AP.
The successes achieved in recent years in the diagnosis and treatment of PRVT are due to the introduction into practice of invasive and noninvasive methods of electrophysiological studies (EPS). We have previously shown [6] that using the non-invasive method of transesophageal electrophysiological study (TE EPS) it is possible to study the characteristics of anterograde AV conduction of excitation in patients with PRUT. The AV conduction curves in most cases corresponded to the curves detected using invasive EPI.
The objective of the study was to study the capabilities of programmed transesophageal electrocardiostimulation (TEC pacing) to determine the characteristics of anterograde conduction of excitation along the AV junction and AP in patients with varying degrees of resistance to PROAVT.
Material and methods
274 patients aged 16 to 69 years with various diseases of the cardiovascular system and suffering from attacks of PROAVT were examined. The first group consisted of 147 patients with manifesting WPW syndrome (WPWm) and PROAVT. Among them there were 59 men and 88 women, whose average age was 39.3±19.2 years. IHD in this group was diagnosed in 12.9% of patients, myocardial cardiosclerosis - in 15.6%, hypertension - in 8.8%, degree II-III mitral valve prolapse - in 6.8%, rheumatic heart disease in 3 .4%, myocardial dystrophy of various etiologies - in 12.9%, vegetative-vascular dystonia - in 8.8%. In 21.8% of patients, in addition to heart rhythm disturbances caused by PVR abnormalities, no other diseases were found.
The duration of the arrhythmic history ranged from two months to 23 years. The frequency of paroxysms in patients in this group averaged 11.3±5.7 attacks per month, and their duration was 9.2±2.7 hours.
The second group consisted of 127 patients with retrograde conduction (hidden) WPW syndrome (WPWc) and PROAVT. Among them there were 52 men and 75 women, the average age was 44.1±21.6 years. IHD in this group was diagnosed in 10.2% of patients, myocarditis cardiosclerosis - in 15%, hypertension in 5.5%, degree II-III mitral valve prolapse - in 16.5%, rheumatic heart disease in 4.7% , myocardial dystrophy of various origins - in 15%, vegetative-vascular dystonia - in 11% and in 13.4% of patients, cardiac arrhythmias were regarded as idiopathic.
The duration of the arrhythmic history ranged from 4 months to 19 years. The frequency of paroxysms in patients in this group averaged 9.8±6.4 attacks per month, and their duration was 8.6±3.1 hours.
It seems that the examined groups of patients were sufficiently representative to analyze the electrophysiological parameters of the cardiac conduction system (CCS). All patients underwent a comprehensive clinical examination, a standard 12-lead ECG was recorded, and 24-hour ECG monitoring (DECG) was performed using the Cardiotechnika-4000 cardiac monitor complex (Inkart, St. Petersburg). A two-dimensional echocardiography study was also performed using a CFM-750 device from Sonatron (Germany).
PE EPI was carried out according to the standard protocol [1,5] using a universal electrocardio stimulator “Kordelektro-4” (Lithuania) and wire-electrodes PEDSP-2 (Kamenets-Podolsk, Ukraine). At the same time, a number of electrophysiological parameters were determined: time of recovery of sinus node function (VVFSU), corrected time of recovery of sinus node function (CVVFSU), Wenckebach point (TV), effective refractory periods (ERP) of the AV junction and AP, tachycardia zone (ZT).
By analogy with the results of invasive EPI [3], 4 types of curves were identified: type 1 - continuous AV conduction curves, characterized by the fact that on the AV conduction excitation curve, a single increase in time St2-R2 did not exceed 20 ms with a “step” of the testing stimulus at 10 ms. This type of curve is more often observed in patients with a “single” conduction pathway through the AV junction, but in some cases, it can also be recorded in patients with two conduction pathways.
Type 2 - intermittent curves of AV conduction of excitation, characterized by the fact that a decrease in the coupling interval of the testing stimulus by 10 ms leads to a “jumpy” increase in St2-R2 by 80-160 ms. This type of curve is more often observed in patients with two or more AV pathways (dissociation of the AV node into alpha and beta channels). Types 3 and 4, in fact, are variants of continuous and intermittent types of AV conduction of excitation in the presence of the Gap phenomenon [3].
In the group of patients with PROAVT and WPW(m) syndrome, continuous types of curves predominated (95%). The predominance of continuous curves of anterograde conduction of excitation can be explained by the unique mechanism of the occurrence of PROAVT. This variant of PRVT is due to the circular motion of the impulse, in which the anterograde link of the re-entry is the AV junction, and the retrograde link is the AP.
In patients with WPW(m) in sinus rhythm (SR), anterograde conduction of excitation to the ventricles occurs simultaneously through the AV junction and the AP, that is, the QRS complex is “confluent.” The conduction of excitation through the AP in WPW syndrome differs from the conduction through the AV node, since, as a rule, it is subject to the “all or nothing” law, which means that the impulse is either conducted along an abnormal path or is blocked. Features of the DPP are presented in Fig. 1.
Patient R., 19 years old. Since childhood, changes have been recorded on the ECG in the form of WPWm. Once or twice a year she noted short attacks of palpitations that went away on their own. Recently I have noticed an increase in frequency and prolongation of paroxysms of tachycardia. On a standard ECG - SR with heart rate = 86 beats/min. PQ - 80 ms. due to the delta wave, QRS = 130 ms. (A).
When carrying out increasing stimulation (St1 -St1 = 410 ms), a sudden “normalization” of the QRS complex was noted due to blockade of the delta wave. As the stimulation frequency increased, a progressive slowing of conduction along the AV junction was recorded (b). Changes in conduction along the AP in this case are explained by the fact that frequent atrial impulses were conducted without delay in the AP (the value of the ST-delta wave interval did not change) up to the critical frequency;
In a number of cases, the presence of decremental conduction in the AP (increase in the P interval - delta wave) was noted as a result of a programmed and increasing frequency of the pacemaker. One of these cases is shown in Fig. 2
#image.jpg
Patient G., 30 years old. About 10 years ago, during a medical examination, the WPW phenomenon was identified. Palpitations did not bother me. At the age of 25 years, during childbirth, a paroxysm of tachycardia occurred, which was stopped by intravenous administration of novocainamide. Subsequently, attacks of palpitations occurred rarely, but were protracted and were stopped by intravenous administration of novocainamide.
Over the past year, I have noticed an increase in heart attacks; I did not take AAP. On a series of DECGs, WPW(m) syndrome, frequent monotopic atrial extrasystole, was recorded. ECG: SC - 800 ms, delta wave (), PQ - 90 ms, QRS - 130 ms (a). Emergency EFI: VVFSU - 1150 ms, KVVFSU - 350 ms. When conducting ECS PPP with coupling intervals from 500 to 420 ms, a constant value of St-delta wave was recorded (b).
In this case, an anterograde slowdown of conduction along the AP (St-delta wave) was recorded during the PPP of the pacemaker. This phenomenon persisted during the control emergency EPI, which casts doubt on the intraatrial conduction delay between the stimulation zone and the AP as the cause of discrete conduction. Most likely, in the above case, the abnormal pathway had the electrophysiological properties of the AV node (“accessory” AV node).
Quite rarely, second-degree blockade of the Samoilov-Wenckebach type is observed in the AP in response to stimulation. In Fig. Figure 3 shows this variant of the occurrence of a blockade in the APP: conducting an emergency pacemaker with a constant frequency (570 ms) led to the fact that one stimulus is conducted through the APP and the AV connection, and the next stimulus is conducted only through the AV connection.
#image.jpg
a) the anterograde ERP of the AP should exceed the ERP of the AV junction;
b) retrograde ERP of the APP should end by the time the ventricles are activated anterogradely through the AV junction.
The last condition can be met only if the atrial premature impulse, catching the AP in a state of refractoriness, is conducted anterogradely along the AV junction and the ventricles slowly enough so that the conduction of excitation in the AP is restored.
Atypical orthodromic reentrant AV tachycardia
It occurs due to the fact that the accessory tracts are slowly retrogradely conductive with attenuated (precremental) ventriculo-arterial conduction; in children it has a chronic course.
It passes anterogradely through the AV junction, then slowly retrogradely along the accessory pathway, is taken up by the atrial myocardium and returns to the AV node.
Signs
- RP>PR
- RP>50% of RR (similar to Fast-Lay)
Against the background of WPW syndrome, there is alternation of the QRS complex, there is involvement of the accessory pathway against the background of tachycardia.
Against the background of orthodromic AV tachycardia, blockade of the right and left bundle branches may occur.
-If there is a blockade of the right leg, then this accessory pathway is retrograde conductive.
— orthodromic tachycardia + left bundle branch block
Diagnostics
Diagnostics includes a number of studies that allow us to judge both the general condition of the body and specifically the activity of the heart. However, the main research method showing rhythm disturbances is an electrocardiogram (ECG).
ECG signs
An ECG is an instrumental diagnostic study, during which special electrodes are applied to the body and limbs, transmitting information to an ECG film. This method allows you to judge the electrical activity of the heart.
The main ECG signs of orthodromic tachycardia are:
- The QRS complexes are narrow and follow each other;
- The distance RR is shortened but remains the same;
- The atrial P wave appears in different places (both before and after the ventricular complexes),
- Layers on the ST interval and T wave;
- Extended RP interval.
The antidromic form of tachycardia on the ECG is diagnosed using the following signs:
- Ventricular complexes (QRS) are wide, similar in shape to bundle branch block, and the distance between them is the same;
- A delta wave is observed, which causes a shortening of the PQ interval;
- The P wave overlaps the QRS complex and may be located after it.
In some cases, with tachycardia against the background of VPU syndrome, T wave inversion is observed - its negative displacement relative to the isoline.
Comprehensive diagnostics
In addition to the ECG, other clinical and additional studies are prescribed.
Clinical diagnosis is carried out by the attending physician. It uses the following methods:
- Collection of complaints - the most disturbing symptoms of tachycardia are diagnosed;
- Taking an anamnesis - determining the presence of risk factors, the likelihood of aggravated heredity,
- Concomitant and background diseases; provoking factors, the nature and duration of paroxysms play a major role in diagnosis;
- Physical examination – the condition of the skin and the activity of the main body systems are assessed;
- Measurement of hemodynamic parameters - measurement of blood pressure and heart rate;
- Auscultation of the heart - assessment of heart rhythm, the nature of heart sounds.
After collecting basic information, additional studies are prescribed:
- Various blood tests (general and biochemical examination, analysis of hormone levels) - prescribed to identify background pathologies;
- Daily ECG monitoring – recording a cardiogram during the day with simultaneous keeping of a diary, which records emotional and physical stress, time of wakefulness and sleep;
- Prescribed for diagnosing the provoking factors of paroxysms, as well as their characteristics;
- Echocardiography is an ultrasound of the heart, which allows one to judge the presence of structural changes in the organ;
- Electrophysiological study - the method involves applying weak doses of current to the heart to assess its response and detect hidden pathologies of the conduction system.
Conducting a large number of studies is necessary to obtain complete information, make an accurate diagnosis and determine treatment tactics.
Antidromic reciprocal AV tachycardia in WPW syndrome
The accessory pathway has a normal effective refractory period. With antidromic reciprocal AV tachycardia, the impulse propagates anterogradely along the accessory pathway and retrogradely through the AV junction.
Signs
- QRS complexes - wide, duration 0.12 seconds or more
- The morphology of the QRS complex resembles ventricular tachycardia, namely left ventricular tachycardia. But according to the clinical picture, antidromic reciprocal AV tachycardia is not at all similar to ventricular tachycardia, the patient talks and generally behaves normally.
- RP-PR
- frequency 150-250 pulses per minute
Fig.5. The mechanism of occurrence of orthodromic and antidromic tachycardias in WPW syndrome
How are orthodromic and antidromic cardiac arrhythmias treated?
Orthodromic tachycardia is treated with vagus nerve stimulation and medication. In some patients, the attack resolves after stimulation of the gag reflex. To normalize heart rate, patients can be administered Trifosadenine, Verapamil. The effectiveness of these drugs reaches 95%. If relief does not occur, then radiofrequency ablation is indicated for patients.
Antidromic tachycardia is stopped using transesophageal pacemaker. Cardiac glucosoids should not be given to patients. If the pacemaker does not help, medications are started. The most effective drugs are Procainamide, Amiodarone, and Aymalin. If, as a result of tachycardia, the patient's hemodynamics are impaired, electrical pulse therapy is performed.
Atrial fibrillation in WPW syndrome
Atrial fibrillation occurs secondary to a previous attack of reciprocal AV tachycardia.
There is an unfavorable prognosis during the course of the disease. Dystrophic changes occur in the atria due to the fact that retrograde excitation of the atria occurs all the time. This contributes to the appearance of attacks of atrial fibrillation and atrial flutter.
Atrial fibrillation due to latent WPW syndrome
Atrial fibrillation due to latent WPW syndrome or due to a long effective refractory period in the accessory pathways.
Atrial fibrillation waves propagate into the ventricles through the AV junction. Added to this are functioning AV blocks. Next, fibrillation waves propagate to the ventricles through anterogradely functioning accessory pathways. This can lead to sudden death, the occurrence of tachyarrhythmias, which can transform into ventricular fibrillation.
When diagnosing atrial fibrillation against the background of WPW syndrome on an electrocardiogram, you need to choose the shortest RR interval:
- if the RR interval is 220 ms or less, then the risk of developing ventricular fibrillation is obvious
- RR interval 250-300 ms - possible risk of developing ventricular fibrillation
- RR interval >300 ms – negligible risk
Against the background of tachysystole, narrow QRS complexes appear. This is explained by the fact that as soon as the heart rate decreases, the impulse is conducted through the AV junction, a narrow QRS complex appears, which has a supraventricular appearance. There can also be a partial capture of complexes; it is neither narrow nor wide; such a complex is called confluent.
Both the narrow and confluent complex confirm atrial fibrillation in the setting of WPW.
Fig.6. ECG for WPW syndrome
Treatment
In this case, it is necessary to prescribe antiarrhythmics of class 1a or 1c - for example, ajmaline. Or perform defibrillation.
Strictly contraindicated:
- cardiac glycosides
- verapamil
These drugs are contraindicated because they increase the refractory period in the AV node and shorten the refractory period in the accessory pathways. Therefore the RR interval becomes even shorter!
Atrial fibrillation may occur due to WPW syndrome with a high ventricular rate.
Classification
Orthodromic tachycardia is divided into the following forms:
- Explicit form - premature contraction of the ventricles is diagnosed on the cardiogram. In addition, there is a shortening of the PQ interval and a narrowing of the QRS complex.
- Hidden form - characterized by the absence of changes on the cardiogram, sinus rhythm is preserved.
Under certain circumstances, orthodromic tachycardia can provoke atrial fibrillation, another form of rhythm disturbance in which the excitation wave quickly spreads and passes from the atria to the ventricles.
This condition can lead to ventricular fibrillation, followed by death.
How do these types of tachycardia manifest themselves?
The sensations during an attack of one of these ailments are very subjective. The severity of manifestations is influenced by a person’s physical and mental health. When the beat frequency increases to 140, patients feel almost nothing. When the heart rate reaches 160, which is characteristic of the orthodromic type of tachycardia, the patient experiences slight weakness and dizziness. Vegetative symptoms appear only in particularly sensitive people. Clinical manifestations of tachycardia are as follows:
- pain in the heart area;
- fainting;
- cardiovascular failure;
- shortness of breath with severe lack of blood circulation.
Read also: Tachycardia with hyperthyroidism
It is noteworthy that in two people with the same type of tachycardia, age and health status, the disease may manifest itself differently. In one patient the attacks will be short-lived. He only encounters them a couple of times a year. Another patient may experience prolonged antidromic tachycardia once in his life without any harm to health.