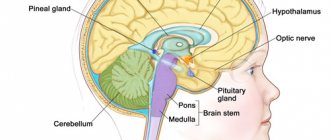
Vagotonia is one of the types of vegetative-vascular dystonia. This is a condition of the body that is caused by excessive tone of the vagus nerve. It is he who regulates the activity of blood vessels, endocrine glands and various internal organs. Therefore, any violation of its functions immediately affects the human condition.
Diagnosis of VSD of the vagotonic type is difficult because it has a large number of symptoms that also apply to other diseases. Diagnosis is also complicated by the fact that the signs of vagotonia are in many ways similar to serious diseases of the lungs, cardiovascular and endocrine systems. If the patient is not monitored in a timely manner and regular examinations are not carried out, somatic disorders and mental disorders may develop.
Autonomic nervous system disorders
Disorders and diseases of the autonomic nervous system can occur at any age, some of which are hereditary (diagnosed in newborns or adolescents). In older age, they are often part of neurodegenerative diseases such as Parkinson's disease or metabolic diseases, in particular diabetes. In general, they can be divided into several schemes.
In terms of origin:
- Primary disorders. Includes various types of dysautonomia, Shy-Dragger syndrome or multiple system atrophy, autonomic degeneration associated with Parkinson's disease.
- Secondary disorders. Caused by autoimmune inflammation in Guillain-Barré syndrome, metabolic disease, chronic renal failure, trauma, etc.
In terms of breadth:
- Localized disorders such as Horner's syndrome, sweating disorders on the upper half of the body in diabetes, swallowing disorders in diabetics, alcoholics, and Parkinson's disease.
- Generalized disorders, for example, fainting with a temporary decrease in sympathetic activity in young girls, in a hot environment, etc.
Nervous system dysfunction can arise from different mechanisms, at different levels. RVNS are divided into several groups depending on the dominant problem.
Reasons for development
VSD of mixed type - let's look at what it is. This type of disease is a combination of vegetative-vascular dystonia of the hypertensive, hypotonic and cardiac type.
It is still unknown exactly why VSD appears. According to experts, the risk of pathology remains high for the following reasons:
- genetic predisposition;
- emotional instability;
- frequent stressful conditions;
- wrong lifestyle.
Important: Maternal anxiety during pregnancy leads to children subsequently suffering from VSD. The pathology usually appears in adolescence
There may be several reasons:
Usually the pathology manifests itself in adolescence. There may be several reasons:
- hormonal changes;
- frequent conflicts;
- mental instability;
- being overly busy at school;
- lack of physical activity.
VSD of mixed type also manifests itself in adults. The risk group includes people with an unstable nervous system. The disease makes itself felt at this age for the following reasons:
- frequent stressful situations;
- unstable work schedule, excessive workload;
- constant lack of sleep.
Vegetative-vascular dystonia is most often diagnosed in people whose work involves mental stress. They usually lead a sedentary lifestyle.
Women are also more likely to suffer from the disease. The reasons for this are as follows:
- Birth of a child. Often this event brings with it postpartum stress, chronic lack of sleep and constant fatigue.
- Average age. Hormonal changes in connection with menopause and a tendency to depression.
Often VSD of mixed type manifests itself against the background of other diseases. During diagnosis, it is necessary to exclude pathologies that have symptoms similar to dystonia. Most often, the disorder has a psychological cause, but there are a number of factors that contribute to the development of the syndrome:
- heredity;
- bad habits (smoking, alcoholism);
- instability of the nervous system (strong impressionability, hysteria, inability to withstand stress);
- hormonal imbalances (puberty, menopause);
- physiological problems (infections, injuries);
- difficult working conditions;
- unfavorable environmental conditions (climate, ecology).
According to doctors, autonomic disorder most often manifests itself in adolescence, pregnancy and menopause.
The main types of neurocirculatory dystonia:
- Cardiac (cardialgia, arrhythmia, high blood pressure).
- Hypotonic (low blood pressure, fainting).
- Hypertensive (high blood pressure, headaches).
- Visceral (dyspepsia, abdominal pain).
- Tachycardial (rapid heartbeat, high blood pressure).
- Asthenic (fatigue, hand tremors, moderate hyperthermia).
- Respiratory (respiratory dysfunction, difficulty breathing, cough).
With VSD of a mixed type, symptoms can be very diverse and combine several types of disease. In rare cases, manifestations of all disease syndromes may be observed. Patients with a mixed type of VSD exhibit severe anxiety, fear, and panic attacks.
Mixed type vegetative-vascular dystonia can occur in women during pregnancy. Often, patients already have a history of VSD of the cardiac, hypotonic or hypertensive type.
After childbirth, the disease may become milder. In a child of school age and adolescence, against the background of stressful situations, psychogenic disorders, as well as overwork, neurocirculatory dystonia can also acquire a mixed type.
Somatoform autonomic dysfunction
Somatoform dysfunction of the autonomic nervous system is a disorder in which a person experiences symptoms similar to those of systemic or organ diseases. Signs are largely or entirely under autonomic innervation and control.
The circulatory system (cardiac neurosis), respiratory tract (psychogenic hyperventilation and hiccups), and gastrointestinal tract (gastric neurosis, nervous diarrhea) are most often affected.
Symptoms of somatoform dysfunction of the autonomic nervous system are usually of two types, neither of which indicate physical impairment of the organ or system involved:
- In the first type of disorder, there are complaints of objective symptoms of autonomic irritation, such as heartbeat, sweating, redness, and trembling.
- The second type of disorder is characterized by more unusual and atypical signs of physical illness, such as pain, burning, heaviness, and bloating.
Symptoms are not under the person's conscious control. This is not a simulation. We could talk about it if his actions were purposefully aimed at obtaining some kind of benefit or profit. But here it is an unconscious process.
Treatment
Recommendations for the effective treatment of somatoform dysfunction of the autonomic nervous system:
- stable treatment with one psychiatrist and one therapist;
- recognition of the truth of the patient's symptoms;
- regular doctor visits;
- use of alternative and instrumental methods and means;
- psychotherapeutic assistance to switch the patient’s attention from symptoms to personal problems, tracking family history in this direction;
- attempts to interpret signs as ways of emotional communication rather than as a new disease.
Diagnosis of VSD in children
Since the symptoms of vegetative vascular dystonia in children are quite nonspecific, diagnosis often presents quite difficulties. To make a diagnosis of VSD, it is necessary to exclude all possible causes of pathological symptoms.
If a child has complaints of nausea, abdominal pain, stool disorders, or loss of appetite, possible diseases of the gastrointestinal tract (peptic ulcer of the stomach and duodenum, gastritis, chronic pancreatitis or cholecystitis, irritable bowel syndrome) should be excluded.
In a child with cardiac syndrome with vegetative-vascular dystonia, diseases of the cardiovascular system (including congenital and acquired heart defects, arterial hypertension, rheumatism, endocarditis) should be excluded.
In the presence of severe shortness of breath, bronchial asthma should be excluded.
It is also necessary to exclude neuroses, depression and other mental disorders, thyroid diseases, and elevated cortisol levels.
For reference. To exclude all possible causes of VSD symptoms, the child should be examined by a pediatrician, cardiologist, gastroenterologist, neurologist and endocrinologist.
A comprehensive examination is also mandatory, including:
- general blood and urine tests;
- electrocardiogram and ultrasound of the heart;
- electroencephalogram;
- fibrogastroduodenoscopy;
- Holter monitoring;
- blood pressure control;
- Ultrasound of the adrenal glands, gastrointestinal tract and thyroid gland;
- hormonal profile study;
- blood chemistry.
Adi syndrome
Adi syndrome is a disease of the nervous system that has numerous manifestations. It's not very common. Adi syndrome is rarely congenital and usually occurs during life.
Causes
The cause of Adi syndrome is not fully understood; it is believed that infection (bacterial or viral) leads to damage to the nervous system, especially its autonomic component.
Manifestations
Destruction of the nerve fibers of the pupil leads to disruption of its reaction (pupilotonia). In a normal person, the pupil dilates in the dark and contracts in the light. The diseased pupil reacts slowly and ineffectively to light changes - it can narrow in the dark (rarely) or expand in the light (more often). Usually only one eye is affected. A person may experience blurred visual acuity, an inability to focus visual attention as well as healthy people.
In addition to visual impairment, the patient experiences increased sweating, also associated with dysfunction of the autonomic nervous system. Last but not least, abnormal tendon reflexes are also present in Adi syndrome. The most common disorder is the Achilles tendon. Patients suffer from unpleasant attacks of sudden drop in blood pressure and have a higher tendency to collapse.
Treatment
Treatment options are limited. Possible visual impairments can be corrected with glasses; Sometimes special drops containing pilocarpine are used. Pilocarpine is a compound that has the ability to temporarily constrict the pupil. There are practically no other therapeutic methods for RVNS.
Vegetative vascular dystonia in adolescents
Symptoms of vegetative-vascular dystonia in adolescents are practically no different from the manifestations of VSD in children under 10 years of age. However, in adolescents, symptoms of VSD are often more intense and occur more frequently. Also, so-called vegetative-vascular crises are more often recorded in them (in children under 10 years of age, vegetative-vascular crises are recorded in isolated cases).
Exacerbation of symptoms of vegetative-vascular dystonia in adolescents is due to hormonal and metabolic changes in the body.
For reference. Most often, vegetative vascular dystonia in adolescents is manifested by irritability, weakness, drowsiness, increased blood pressure (less often decreased blood pressure), tachycardia and impaired thermoregulation. Quite often there is increased sweating and insomnia.
Also, shortness of breath, decreased tolerance to physical activity, rapid fatigue, memory loss, impaired attention, and fainting are often recorded in adolescents (especially in girls with hypotonic VSD).
Autonomic dysreflexia
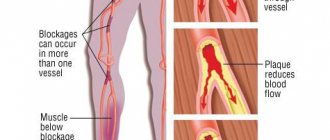
Autonomic dysreflexia is a serious complication affecting more than 50% of patients with spinal cord injury above the 6th thoracic region. In a disorder of the autonomic nervous system, irritation below the level of the spinal cord lesion is the source of severe vasoconstriction, causing paroxysmal hypertension.
Manifestations
An exacerbation of blood pressure may present with one or more of the following symptoms:
- A sudden and significant increase in systolic and diastolic blood pressure above the patient's normal level, usually associated with bradycardia.
- Throbbing headache.
- Significant sweating above the level of the lesion, especially on the face, neck and shoulders (rarely below the level of the lesion).
- Goose bumps above and below the level of the lesion.
- Blurred vision, spots in the field of vision.
- Hyperemia and swelling of the nasal mucosa, a feeling of nasal congestion.
- Bad feeling, fear, anxiety due to an impending insurmountable physical problem.
- Minimal or no symptoms of hypertension despite increased blood pressure.
- Cardiovascular signs (arrhythmias, extrasystoles).
Symptoms may be minimal or even absent despite the hypertensive state.
Causes
Autonomic dysreflexia has many potential causes. To eliminate an attack, it is necessary to conduct a diagnosis aimed at identifying a specific causative factor. The most common reasons:
- urinary tract infections;
- cystoscopy, urodynamic study, incorrect catheterization;
- inflammation of the testicles or their depression;
- expansion of the full colon during constipation;
- intestinal obstruction;
- gallstones;
- stomach ulcers or inflammation of the stomach lining;
- haemorrhoids;
- appendicitis or other abdominal pathology, trauma;
- menstruation;
- pregnancy, especially childbirth;
- vaginitis;
- sexual intercourse, orgasm;
- ejaculation;
- deep thrombosis;
- pulmonary embolism;
- frostbite;
- tight clothes, shoes;
- burns (including sunburn);
- fracture or other injury;
- surgical or diagnostic procedures;
- pain;
- osteochondrosis;
- temperature fluctuations;
- any painful or irritating sensations below the level of injury;
- drugs, large amounts of alcohol, etc.
Treatment
The procedure for treating an episode of autonomic dysreflexia begins with repositioning the patient using orthostatic blood pressure lowering. The next important condition is to relax the tight parts of clothing and remove compression products. The goal is to relieve symptoms and prevent complications associated with uncontrolled hypertension.
Pharmacological treatment:
- Nifedipine (Cordipine) is a calcium channel blocker that selectively inhibits the penetration of calcium ions through the cell membrane of the heart muscle and through the membrane of vascular smooth muscle without changing the concentration of calcium in the blood serum.
- Nitrates (nitroglycerin, isosorbide dinitrate) are drugs that relax vascular smooth muscle, with a vasodilator effect on peripheral arteries and veins.
- Terazosin is a long-acting drug that selectively blocks alpha-1 adrenergic receptors. Selective alpha-1 blockade causes relaxation of vascular smooth muscle.
- Prazosin is a selective alpha-adrenergic receptor antagonist that reduces total peripheral resistance associated with sympathetic activity.
- Captopril is a specific angiotensin-converting enzyme (ACE) inhibitor that blocks the renin-angiotensin-aldosterone system and causes a decrease in peripheral arterial resistance without changing cardiac output.
Symptoms of VSD in children under 10 years of age
Symptoms of vegetative-vascular dystonia in young children may appear:
- constant weakness, drowsiness, lethargy;
- tearfulness, moodiness and frequent mood swings;
- lability of blood pressure (blood pressure may drop below normal or increase significantly);
- anxiety, phobias, suspiciousness, increased sensitivity;
- attacks of dizziness and headaches;
- tachycardia (increased heart rate);
- decreased memory, deteriorated ability to concentrate, decreased ability to assimilate new information;
- increased sweating (increased with nervous tension).
Also, the child may experience an alternation of increased nervousness with depressive moods and periods of apathy.
For reference. Frequent and characteristic complaints with vegetative vascular dystonia are sensations of incomplete inspiration, lack of air and discomfort when trying to take a deeper breath.
Thermoregulatory disorders in children with vegetative-vascular dystonia are manifested by chilliness, attacks of chills, and poor tolerance to cold or heat.
Also, parents are often concerned about the child’s poor appetite and the fact that he is not gaining weight well (children with vegetative-vascular dystonia, as a rule, have an asthenic physique).
In cardiac syndrome, patients with vegetative-vascular dystonia are concerned about rapid heartbeat, weakness, increased or decreased blood pressure, sensations of “interruptions” in the heart’s function or a feeling of “fading” of the heart. Mild arrhythmias are also often observed; irregular extrasystoles are less often recorded.
For reference. Disturbances in the gastrointestinal tract can be manifested by nausea (especially in the morning), bloating, diarrhea or periodic constipation, cramping abdominal pain.
Quite often, children with VSD experience:
- increased skin greasiness;
- excessive skin sensitivity;
- the appearance of red dermographism (red marks on the skin after rubbing with a nail);
- frequent urination;
- tendency to fluid retention and edema.
Complex regional pain syndrome
Complex regional pain syndrome (CRPS) is a term used to describe a variety of regionally localized pain conditions that are primarily the result of trauma. They are characterized by clinical changes with a maximum distance from the primary affected area.
Manifestations
The process of SRPS is divided into 3 stages, each of which has its own clinical picture.
Acute stage (decreased sympathetic activity):
- increased blood circulation;
- temperature increase;
- sweating;
- acceleration of body hair and nail growth;
- local swelling;
- redness;
- decreased mobility.
Dystrophic stage (increased sympathetic activity):
- decreased blood circulation and skin temperature;
- slower hair growth, brittle nails;
- expansion of edema;
- more pronounced limitation of range of motion;
- spotted osteoporosis.
Atrophic phase (irreversible):
- deepening tissue changes;
- damage to all tissues, leading to irreversible disruption of the configuration and position of the joints;
- joint deformities with severe mobility impairment;
- necrosis.
Causes
This dysfunction of the nervous system has both external and internal causes.
External factors:
- injuries (skeleton, soft tissues, nerves);
- operations;
- burns;
- frostbite;
- overload of muscles and ligaments;
- inappropriate and painful treatment methods (tight cast, painful rehabilitation, incorrectly prescribed physical therapy), especially in a child.
Internal factors:
- inflammation (nonspecific, specific);
- heart attack;
- stroke;
- tumor hyperemia;
- barbiturate intoxication;
- anti-tuberculosis therapy.
Treatment
Treatment of SRPS should be comprehensive, including regimen measures, rehabilitation, physical therapy, pharmacotherapy and invasive means. Treatment of advanced disease always requires a specialized approach in the field of neurology. Only stages 1-2 of the disease have a good prognosis (hope for a positive functional result).
The basic principle is pain relief with analgesics and physical means. The affected segment should not be overloaded even during rehabilitation.
Today there are no generally accepted criteria for the treatment of this serious disease based on medical evidence. This reflects the fact that only a few randomized treatment trials have been published in this area to date.
Vegetative vascular dystonia in children - what is it?
Vegetative vascular dystonia in children is a complex of functional disorders in the work of various organs and systems associated with an imbalance between the work of the sympathetic and parasympathetic nervous systems.
For reference. Every parent must understand that his child suffers psycho-emotional overload when visiting a kindergarten, school or other places where people (children) are unfamiliar to him and the conditions of communication with them.
This is obvious - it transfers. And what other ones! An adult with an established psyche and life experience, coming to a new team, feels psycho-emotional overload. But an adult partly knows how to “control himself.” But a child with a developing psyche is unlikely to be able to control himself (read: his nervous system).
Vegetative vascular dystonia in a child can manifest itself in the form of a complex of cardiac, respiratory and neurotic syndromes, impaired thermoregulation and vegetative vascular crises.
According to official medical statistics, symptoms of vegetative-vascular dystonia are recorded in almost 80% of children and adolescents. The first symptoms of VSD in children most often appear at the age of 6-8 years and in adolescence.
In girls, symptoms of vegetative-vascular dystonia are more common than in boys.
Let us recall that in pediatrics (and not only) the diagnosis of VSD is not considered as an independent nosological unit (specific disease). When receiving this diagnosis, you must contact a specialist: pediatric cardiologist, pediatric endocrinologist, pediatric gastroenterologist, etc.
Pay attention to the fact that pediatric and adult doctors are different professions in terms of applied aspects (different approaches to diagnosis and treatment).
Children under 5 years old
The category “under 5 years” also includes infants, for whom the diagnosis of VSD is made by exclusion. Otherwise, it is a diagnosis of exclusion.
Naturally, the baby is in no way able to convey his complaints about his health. Therefore, the pediatrician examines the child to rule out possible causes of the current condition. Which may lead to the idea that there are violations of the regulatory system.
From the age of possible start of attending kindergarten, the risks of psycho-emotional overload increase:
- a stranger (the teacher) begins to establish his own routine, which is unusual for the child,
- unfamiliar children lay claim to their favorite toy,
- daytime rest (sleep) at a strictly defined time.
For reference. A child with an unstable psyche finds himself in new conditions, some of the rules of which he does not like. This is psycho-emotional overload in its purest form. What is the reaction of the child’s nervous system? An attempt at adaptation. And this attempt is not always successful.
As a result:
- appetite decreases, which leads to weight loss,
- irritability and moodiness develop,
- sleep deteriorates, and, consequently, recovery and the child experiences fatigue,
- Colds become more frequent.
These are not all possible results, but they occur very often. These are not symptoms of the disease. This is precisely vegetative-vascular dystonia, which can result in any disease.
VSD in children under 10 years of age
In this age category, children can already partially formulate their health problems. The diagnosis of VSD in children of this category most often falls within the period of 7 years. Before this, everything was already settled with the kindergarten. The child got used to it and there were fewer stressful situations.
But from the age of seven, neurologists note two periods of risk for the development of VSD:
- admission to school,
- restructuring of the endocrine system.
In any case, psycho-emotional overloads arise due to the complexity of the curriculum, joining a new team, changing the daily routine, and overwork.
For reference. Limitation of physical activity also plays a depressing role. Sitting in class (at least 30 minutes). Sitting at the computer for a long time is also mixed in. This is exactly the age of mastering the Internet space.
As a result:
- insomnia,
- headaches with dizziness,
- increased fatigue,
- memory loss,
- spontaneous shortness of breath,
- periodic increases in body temperature.
Horner's syndrome
Horner's syndrome is a neurotic syndrome, a combination of 3 symptoms that arise from disorders of the sympathetic nervous system in the neck area. The sympathetic nervous system is a set of nerves and nerve ganglia that regulate certain functions of the body that do not depend on the will of a person. The cervical sympathetic system also controls the eyes.
Causes
There are many causes of cervical sympathetic nerve damage. In addition to neck injuries, some locally growing tumors are involved in the genesis, such as thyroid and lung cancer growing in the upper lobe of the lung (Pancoast tumor). Symptoms consistent with Horner syndrome may also occur with disorders such as:
- multiple sclerosis;
- spinal cord damage due to syringomyelia;
- thrombosis of the cavernous canal;
- migraine (temporary).
Manifestations
The most common signs of sympathetic damage:
- constriction of the pupil (miosis);
- drooping eyelid (ptosis);
- visible slight recession of the eye into the orbital fossa (enophthalmos).
The most noticeable constriction of one pupil. There may also be facial redness on the affected side. This phenomenon is caused by the dilation of subcutaneous blood vessels in this area of the skin.
Treatment
A patient with Horner's syndrome should be examined by a neurologist; As part of the diagnosis, it is important to exclude brain disease (CT or MRI), compression of the nerve structures in the neck (ultrasound, CT).
Treatment of the syndrome depends on the underlying disease. If the disease is treatable and the nerve damage is not irreversible, the condition can be corrected through strengthening techniques and medications.
Treatment
If you suspect SVD, you should contact a neurologist. After confirming the diagnosis, this doctor prescribes a treatment regimen, which has the following tasks:
- preventing crises;
- relief of the main symptoms of SVD;
- treatment of concomitant diseases;
- normalization of the patient’s psycho-emotional state.
To achieve these goals, the patient must follow a number of simple rules relating to all areas of his life. The list of recommendations looks like this:
- walk in the fresh air more often;
- harden the body;
- have a good rest;
- stop smoking, eliminate alcohol;
- sleep at least 7-8 hours a day;
- engage in team sports, swimming;
- eliminate sources of stress by normalizing family and household relationships;
- eat small meals, limit the consumption of salty and spicy foods.
Physiotherapeutic procedures
Treatment of autonomic dysfunction syndrome is not always associated with taking medications. If the course of the disease is smooth, without pronounced crises, then the patient is prescribed only physiotherapy and traditional medicine. The indication for taking medications is the paroxysmal course of SVD with severe exacerbations. In this case, physiotherapy is used in combination with medications. To normalize the activity of the autonomic nervous system, the following procedures are useful:
- Aquatic. This includes medicinal baths, including mineral waters, which soothe the body. Another procedure is Charcot's shower. It consists of massaging the body with a stream of water. Regular swimming in the pool also has a calming and tonic effect.
- Electrosleep therapy is the effect on the brain of a low-frequency pulsed current. Improves blood circulation, reduces pain sensitivity, increases minute breathing volume.
- Acupuncture. Relieves stress, promotes relaxation, and improves overall vitality.
- General massage. Relieves muscle tension, normalizes heart rate, eliminates headaches, gives a powerful boost of energy, copes with fatigue and overwork.
Drug therapy
If physiotherapy and restorative treatment methods do not bring a positive result, then the patient is prescribed medication. Depending on the symptoms, the following groups of drugs can be used:
- Neuroleptics: Sonapax, Frenolone. They reduce the speed of transmission of brain impulses, thereby helping to eliminate fear. Indicated for mental disorders.
- Antidepressants: Azafen, Trimipramine. They eliminate signs of depression, therefore they are used to treat anxiety and panic disorders, neuroses, bulimia, and enuresis.
- Strengthening vessels: Trental, Cavinton. Improve cerebral metabolism and blood circulation, reduce blood vessel resistance. In neurology they are used for neurological and mental disorders.
- Hypotonics: Anaprilin, Tenormin, Egilok. Helps reduce blood pressure in hypotonic types of autonomic dysfunction.
- Nootropic: Piracetam, Pantogam. They trigger metabolic processes in the central nervous system, improve regional blood circulation, and facilitate the learning process. Prescribed for vegetative-vascular dystonia, neurogenic urination disorder, neurotic disorders.
- Sleeping pills: Flurazepam, Temazepam. Indicated for early or night awakenings, disruption of the process of falling asleep. In addition to sleeping pills, they have a sedative effect.
- Cardiac: Digitoxin, Korglykon. They have antiarrhythmic and cardiotonic effects. Indicated for migraine attacks, high heart rate, chronic heart failure.
- Tranquilizers: Phenazepam, Seduxen, Relanium. Used for vegetative crises, convulsive reactions, and depressive states. They have a hypnotic and sedative effect.
Folk remedies
In case of permanent autonomic dysfunction syndrome, treatment with folk remedies is allowed. After consultation with a doctor, they can also be used by pregnant women, since synthetic drugs are contraindicated during pregnancy. In general, the following remedies are recommended for patients with autonomic dysfunction:
- Mix 25 g of raisins, figs, nuts and 200 g of dried apricots. Grind all ingredients using a meat grinder or blender. Eat 1 tbsp daily on an empty stomach. l. remedies, washed down with kefir or yogurt. Repeat for a month. Next, take a week's break and undergo another treatment course.
- Brew 3 tbsp with a glass of boiling water. l. motherwort herbs, leave for 1.5 hours. Drink 1 tbsp each time before meals. l. Take until the condition improves.
- For 5 medium cloves of garlic, take the juice of 5 lemons and a glass of honey. Mix everything and leave for a week. Next, take 1 tsp. products up to 3 times throughout the day. Time of administration: before meals. The course of therapy should last 2 months.
- Drink chamomile daily as tea by brewing 1 tbsp. l. herbs with a glass of boiling water.
Damage to the autonomic system due to poisoning
Autonomic disorder can be caused by organophosphates - substances that block the action of acetylcholisterase, an enzyme that breaks down acetylcholine. Thus, a large amount of acetylcholine accumulates in synapses, which, by binding to receptors, can cause long-term effects and various manifestations.
Organophosphates were originally developed as warfare gases under the names sarin, soman, and tabun. Today they are widely used as insecticides. The effects of organophosphates can be divided depending on the receptors on which they act:
- Nicotine. They arise due to the activation of sympathetic and parasympathetic ganglia and are manifested by changes in blood pressure, cardiac activity, metabolic disorders, and convulsions due to the presence of nicotinic receptors on the neuromuscular disc.
- Muscarinic – peripheral-parasympathetic. Manifestations include salivation, lacrimation, diarrhea, increased motility, vomiting, and bronchospasm.
- Acetylcholine occurs as a neurotransmitter primarily with excitatory effects in the central nervous system. At first the effects are irritating, then fade away. They manifest themselves as headaches, dizziness, feelings of fear, miosis, and loss of consciousness.
Reasons for development
Often VSD of mixed type manifests itself against the background of other diseases. During diagnosis, it is necessary to exclude pathologies that have symptoms similar to dystonia. Most often, the disorder has a psychological cause, but there are a number of factors that contribute to the development of the syndrome:
- heredity;
- bad habits (smoking, alcoholism);
- instability of the nervous system (strong impressionability, hysteria, inability to withstand stress);
- hormonal imbalances (puberty, menopause);
- physiological problems (infections, injuries);
- difficult working conditions;
- unfavorable environmental conditions (climate, ecology).
According to doctors, autonomic disorder most often manifests itself in adolescence, pregnancy and menopause.
ANS disorders caused by trauma
The most serious damage in this regard is above the T6 segment. When the sympathetic is activated, for example by filling the bladder, due to vasoconstriction in the gastrointestinal tract, blood pressure increases significantly due to afferent fibers. Because the disorder blocks efferent innervation, high blood pressure persists because the vessels in the gastrointestinal tract cannot relax. In fact, this is a long-term “centralization of blood circulation”, which is also a reaction to stress.
In addition to affecting the ANS, spinal cord injury above T6 may also present with various forms of respiratory impairment. This serious disorder is a reason for young men to delay military service.
As a result of generalized vasodilation caused by a disorder of the spinal cord in the thoracic region, neurogenic shock occurs. The most commonly injured system due to impact is the sympathetic or thoracolumbar system, most commonly during injuries around T5; vascular tone is lost in the gastrointestinal tract. This reduces venous return and relatively reduces the volume of circulating blood. Tissues are hyperperfused, compensatory mechanisms are activated, but sympathetic mechanisms cannot be involved. Shock develops.
RVNS is a condition that requires a specialized treatment approach. Home treatment and traditional methods can only be used as an addition to therapy, exclusively with the permission of a doctor.
Causes of VSD of mixed type
The exact cause of the disease cannot be identified. The causes of this disease can be very diverse. Sometimes the cause can be any other disease (from pathologies of the cardiovascular system to ARVI). But most often, vegetative-vascular dystonia of the mixed type appears due to the following factors:
- heredity;
- stress, severe shock, emotional overstrain, impressionability;
- bad habits (alcohol, smoking);
- traumatic brain injuries;
- hormonal imbalances;
- unfavorable environment;
- poor working conditions.
Causes of the disease
What is VSD of mixed type? According to some experts, the disorder develops against the background of a hereditary tendency to inferior autonomic regulation of body functions. This happens due to trigger effects.
Examination for vegetative-vascular dystonia includes the entire range of laboratory tests. Making a diagnosis is very difficult. The examination also includes x-rays.
The development of vegetative-vascular dystonia is caused by the following factors:
- Genetic predisposition.
- Wrong lifestyle.
- Brain injury.
- Working under stress.
- Instability of the patient's nervous system.
- Unfavorable social or economic conditions.
- Central nervous system diseases, frequent dizziness, stroke.
- Hormonal imbalances.
- Abuse of alcohol and tobacco products.
- Incorrect diet.
- Disturbances of the endocrine system.
- Physical inactivity.