Cardiac pathologies are heterogeneous in nature. Many manifest themselves as early macroscopic changes in muscle fibers and other structures.
Most diseases of this profile have a high mortality rate. Sooner or later they lead to at least disability. Maximum - to the death of a person in a different perspective.
There is a group of processes that do not have early manifestations at all. Which complicates diagnosis and timely treatment.
Diffuse changes in the myocardium is a generalized name for microscopic abnormalities in cardiomyocytes, the cells of the muscle organ, over the entire area of the heart. In the vast majority of cases, the pathological process is of metabolic origin.
The movement of substances in and out is disrupted, the nutrition of the cardiac structures drops and becomes inadequately low. For this reason, defective cardiomyocytes grow throughout the muscular organ.
Another possible option is the formation of scar tissue in place of functionally active, dead tissue. In this case, diffuse changes are equal to sclerosis.
The mechanism of pathology development
The process of transformation of normal tissues into altered ones can be imagined in stages. An approximate diagram is as follows:
- Cardiac structures are affected by a negative factor of internal or external origin. There are many of them. Especially often, the onset of diffuse abnormalities is caused by gross metabolic disorders, endocrine conditions and other cardiac pathologies. Minor changes begin in the cells.
- Metabolism (metabolism) at the local level decreases. The heart does not receive enough nutrients. The contractility of the myocardium turns out to be minimal and becomes inadequately weak. Therefore, the muscular organ is unable to provide blood not only to distant systems, but also to itself. Here moderate changes appear in the myocardium.
- To compensate for the lack of work, the body tries to solve the problem by increasing the mass (hypertrophy) of the myocardium. Myocytes of this origin do not have much anatomical significance, since they are not able to fully contract. On the contrary, the condition is getting worse. The progression of the pathological process continues at an accelerated pace and provokes pronounced changes in the structure of the heart muscle.
Hence the generalized hemodynamic disturbances. Ischemia, atrophy, multiple organ failure and other consequences are a “bonus”.
Another possible variant of diffuse changes in the structure of the myocardium is cardiosclerosis. That is, the replacement of functionally active tissues with scar tissue.
This process occurs against the background of coronary insufficiency in most cases. It flows for years, gradually leading to transformation of the heart at the cellular level.
What does diffuse changes in the myocardium generally indicate? In essence, the term means the process of cellular transformation widespread throughout the entire area of cardiac structures.
This is not a diagnosis, but just an indication of a defect, and an extremely general one, which is more often used by doctors of functional diagnostics.
The rule of good manners in medicine is to clarify the character. As far as possible. Usually we are talking about myocardiosclerosis (replacement of functional tissues with scar tissue). Less often about myopathy (growth or stretching of the muscle layer).
Both phenomena are extremely unfavorable in terms of complete cure.
Types of changes in the myocardium
- Changes in the myocardium can spread to all cells, then these are diffuse anomalies. Or damage to individual areas of the heart muscle is possible - in this case we are talking about focal disorders.
- Modification of myocardiocytes can be irreversible when the cells are completely destroyed and replaced by connective tissue. This pathology is very dangerous; it can lead to heart failure or heart attack. With reversible transformations of the cellular structure, the destructive process can be stopped by completely restoring the damaged tissue.
- There are moderate (minor or nonspecific) and severe diffuse changes in the myocardium. The former exist asymptomatically and are detected only on an ECG. Often such disorders do not pose a danger to the body and may even be a variant of the norm (for example, in a child or an elderly person). They are always reversible and are not associated with heart pathologies. The latter need close attention, they require mandatory treatment, manifest themselves with tangible symptoms, and lead to serious consequences. They usually accompany various heart diseases. Both changes can lead to irreversible processes over time. Therefore, the cause of diffuse anomalies and the degree of their danger must be established.
Causes
Factors in the development of the defect vary in type and degree of danger.
As practice shows, many issues are subjective in nature and can be eliminated by the patient himself without any special difficulties in terms of physiology. Psychologically, life changes can be difficult.
Prolonged, excessively active sports activities
Or the physical nature of professional activity. Development follows a simple path. With inappropriately strong stimulation of cardiac structures, a disruption of normal blood flow is observed.
Fluid connective tissue can stagnate in the chambers, especially the left ventricle. If this does not happen, the heart is forced to intensify its work to provide the muscles with nutrition and oxygen.
Hence the proliferation of cardiomyocytes, an increase in the volume of the heart. It is also possible for the gradual death of functionally active tissues to be replaced by scars.
Both options end in pathological transformation of cardiac structures at the cellular level. This phenomenon is the basis for a complete abandonment of sports or a change in the nature of professional activity.
Momentary significant intoxication
For example, ethanol poisoning, if a person has had too much alcohol, damage from salts and vapors of heavy metals (especially mercury). Long-term poisoning of a less active nature also affects.
For example, with the improper use of antiarrhythmic drugs, anti-inflammatory drugs, corticosteroids or cardiac glycosides.
The latter are especially dangerous in terms of the likelihood of diffuse changes. The only way to stop a negative phenomenon is to eliminate the main factor.
Frequent viral diseases
This is popularly called a “complication of the heart.” In fact, this is how it is. The main danger is influenza; other agents are somewhat less threatening.
Ideally, avoid colds, lead a healthy lifestyle and keep your immune system in full combat readiness.
History of tuberculosis
Mycobacterium or Koch's bacillus is extremely insidious. It can camouflage itself for a long time or destroy the lungs, without giving visible symptoms until the last moment, when it can no longer be helped radically.
The danger lies not only in the disease itself, but also in the treatment. Heavy drugs are used. First of all, fluoroquinolone antibiotics, which are highly active against pathogenic structures.
By themselves, they have a lot of side effects. Taking into account the fact that the drugs are prescribed in shock dosages, it becomes clear how it all ends.
Gastrointestinal pathologies
Especially those associated with minor bleeding of a prolonged nature. There is no direct connection between diffuse changes in the myocardium and gastrointestinal pathologies. It's indirect.
As a result of the constant loss of iron with liquid connective tissue, secondary anemia or depletion of hemoglobin occurs. Hence the disruption of cellular respiration, hypoxia, and the development of a degenerative process in the heart.
The longer the disease lasts, the more significant the organic changes. Recovery is carried out with shock doses of iron supplements.
Anemia is not always the result of a deficiency of Fe compounds. Other options are possible. For example, megaloblastic form.
It is associated with insufficient intake or absorption of vitamin B12. Treatment presents certain difficulties. Usually performed in a hospital.
If the condition is eliminated at an early stage, there is a chance that diffuse changes in the heart will not occur.
Kidney failure
In the phase of sub- or decompensation (to a special extent). The essence is a violation of liquid filtration.
The paired organ is not able to properly evacuate excess water, and oliguria occurs. That is, a decrease in daily diuresis down to a minimum of 200-300 ml.
This leads to an increase in the amount of blood circulating in the body. The load on the cardiac structures increases, first the chambers dilate (expand), and then the proliferation of cardiomyocytes occurs.
Liver failure
The mechanism of development of diffuse deviations is somewhat different. This organ is considered a biochemical laboratory and a filter at the same time.
If its work is disrupted, generalized intoxication of varying degrees of severity occurs. The heart degrades and severe tissue scarring occurs.
The epithelium is unable to contract. Therefore, there is a decrease in the functional activity of cardiac structures.
Atherosclerosis
Primarily coronary arteries, also atherosclerosis of the aorta. The essence of the disease is a violation of vascular patency.
There are two process options:
- The first is blockage of the lumen with a cholesterol plaque.
- The second is stenosis, that is, narrowing.
If lipid structures can be eliminated with medications, conduction disturbances for other reasons can only be stopped surgically, as necessary.
Coronary or aortic insufficiency leads to malnutrition of the heart and its pathological transformation in the medium term (3-5 years or less).
Severe arterial hypertension
Increased pressure. Leads to overload of cardiac structures and provokes vascular fragility.
Inflammation of the myocardium and surrounding tissues
Usually of infectious origin (eg myocarditis). The variety is extremely aggressive and causes destruction of the atria. The autoimmune type is also possible.
It is less active, but much more difficult to cure; a good result is a transfer into remission, but you should not expect a complete recovery. Both options in the acute phase are treated in the hospital.
Metabolic diseases
Including diabetes and other conditions. They cannot be completely cured due to generalized deviations from the endocrine system.
Alcohol abuse, long-term smoking and drug addiction also have an impact. Patients aged 55+ are especially at risk; men are more susceptible to diffuse changes.
There is a possible connection between the described condition and family history.
Genetic defects and disorders of the perinatal period of a spontaneous nature provoke congenital abnormalities. They are no less dangerous and difficult to diagnose.
Main causes of diffuse changes
These reasons include:
- myocarditis;
- myocardial dystrophy;
- myocardiosclerosis.
Myocarditis
Myocarditis is caused by an inflammatory process in the area of the heart muscle. Infectious diseases can provoke it: diphtheria, measles, influenza, pneumonia, tuberculosis, scarlet fever, typhoid, herpes, hepatitis. There are also myocarditis of allergic, autoimmune (rheumatism, lupus erythematosus), endocrine (thyrotoxicosis) and toxic origin. The cause of myocardial inflammation may be foci of chronic infections in the body (tonsillitis, caries, sinusitis). The affected cells die, and patches of connective tissue form in their place, which eventually leads to cardiosclerosis. Consequences: disruption of the conductivity of the electrical signal, inconsistency of contractions of the heart chambers.
Myocardial dystrophy
This name refers to metabolic processes occurring abnormally in the cells of the heart muscle. As a result of such disorders, energy production in myocardiocytes decreases, contractile activity worsens, and heart rhythm disturbances occur. The cause of dystrophic changes in myocardial tissue must be sought in external factors not related to pathologies of the organ itself:
- past illnesses;
- chronic diseases;
- malnutrition;
- lack of vitamins;
- hormonal disorders;
- the influence of alcohol, tobacco tar, narcotic substances;
- water and electrolyte imbalance;
- metabolic disorders in the body;
- frequent stress;
- physical overexertion (“sports” heart);
- overweight;
- prolonged exposure to low or high temperatures;
- chronic insomnia;
- side effects of certain medications.
At first, diffuse transformations are reversible and easily treatable. But the advanced stage leads to the death of heart cells and the development of sclerotic phenomena.
Myocardiosclerosis
During this disease, connective tissue is formed in the myocardium, instead of muscle cells. Deformation of cardiomyocytes and their death occur for various reasons (heart attack, inflammatory processes, degenerative changes). Scars that appear at the site of necrotic areas may be a consequence of atherosclerosis of the coronary arteries. Vasoconstriction leads to hypoxia, causing cell dysfunction and death. Dead myocardiocytes cannot be restored; dead muscle areas cause the following consequences:
- atrial fibrillation;
- heart failure;
- development of aneurysm;
- ischemic disease;
- myocardial infarction.
With diffuse sclerotic changes, scar tissue evenly spreads over the entire area of the myocardium, its size begins to grow. First, left ventricular hypertrophy is observed. After some time, dilatation of the cavities of the heart is recorded, blood flow inside the organ worsens, and full contractions become impossible.
Symptoms
The problem is that moderate diffuse changes in the myocardium and even advanced stages do not always provide a typical clinical picture sufficient to visit a doctor or make a diagnosis on the spot at an appointment with a cardiologist.
Signs appear as the pathological process progresses.
The average version looks like this:
- Moderate or mild pain in the chest. Indicate a disruption in the normal functioning of cardiac structures. In the vast majority of cases, they are associated with angina pectoris.
The discomfort is not constant and occurs after physical exertion (angina pectoris) or at complete rest (angina pectoris at rest).
Lasts no more than 30 minutes. If longer, there is reason to suspect a heart attack (read about the first signs here).
- Arrhythmias. Depends on the form of the condition. Many variants of diffuse disorders are manifested by tachycardia, that is, an acceleration of the contraction frequency. The reverse type is possible.
In addition to heart rate deviations from the norm, extrasystoles and fibrillation (atrial or ventricular) are noted.
Attention:
The parallel course of processes entails life-threatening consequences. Cases of cardiac arrest are common.
- Dyspnea. First, against the background of intense physical activity. The threshold for the onset of a symptom may be so high that the patient does not see or feel the development of the defect.
As you progress, the bar drops. It ends with the sign being observed in absolute rest.
Against the background of tachycardia, this condition is defined by patients as extremely painful. It is impossible to perform household duties, professional fulfillment is difficult.
- Fast fatiguability. Fatigue also occurs after physical activity. Emotional to a lesser extent. Muscle activity requires more nutrition, which the heart is not able to provide.
- During attacks - cyanosis of the nasolabial triangle, pallor of the skin and increased sweating. Hyperhidrosis generally becomes a constant companion of a person. Minimal physical activity leads to the fact that the patient can literally be squeezed out.
- Swelling of the lower extremities. Especially in the morning and evening.
Attention:
Since diffuse changes in the heart are not a diagnosis, they are signs of concomitant pathologies.
Depending on the underlying cause of the condition, other symptoms are possible. For example, increased body temperature, changes in appearance due to hyperthyroidism, decreased vision, prolonged wound healing due to diabetes mellitus, and others.
Clinical manifestations
Subjective (or patient complaints) and objective symptoms of this condition are distinguished. To resolve a question regarding normality or pathology, the doctor takes into account all the information obtained during the interview of the person, as well as data from the results of additional studies.
Complaints
In most cases, patients with diffuse myocardial changes do not complain. During a routine medical examination, this condition is detected by chance on an electrocardiogram. At such moments, only dynamic observation by a therapist is required.
With pronounced diffuse changes, when the functioning of cardiomyocytes is significantly impaired, the following symptoms appear:
- fatigue increases;
- unreasonable weakness;
- shortness of breath when walking for a long time or when climbing stairs;
- a feeling of interruptions in the work of the heart;
- pain behind the sternum with usual exercise;
- increased nervousness.
In some cases, a survey can identify the disease that resulted in the transformation of the myocardium.
Any changes in the myocardium always require dynamic monitoring. In some situations, additional examination and subsequent treatment by a cardiologist may be required.
Objective symptoms
Most often, diffuse changes in the myocardium are detected on the electrocardiogram. Only a specialist can see and correctly interpret the current state.
Changes in the myocardium on the ECG against the background of dystrophic processes are manifested by the following signs:
- Rhythm disturbances (cause – pathology of impulse conduction). Atrioventricular blockades are more often recorded, and tachyatrymia (atrial fibrillation) is less common.
- ST segment displacement (depression or elevation). Concavity of this area is extremely rare.
- Inversion and broadening of the T wave. The amplitude remains the same.
There are many more methods for establishing diffuse changes, but the signs listed above are among the main ones and are leading in making a diagnosis.
If you plunge into practice, the ECG curve always looks individual. Only one of the listed signs may be recorded. But there is still a problem in the heart. Such features forced me to make mistakes more than once when studying cardiograms, especially at the beginning of my working life.
To recognize changes in the myocardium, a method such as cardiac ultrasound (Echo-CG) is also used. It shows sclerotic transformation of muscle tissue and contractility disorders. This is a more effective way to detect abnormalities in the heart muscle.
Diagnostics
The examination is indicated under the supervision of a cardiologist, less often a specialized surgeon.
Scheme of events:
- Oral questioning of the patient regarding complaints, their duration and nature. An approximate clinical picture gives an idea of the pathological process, but not always.
- Anamnesis collection. Lifestyle, previous diseases and other information.
- Measurement of blood pressure, heart rate. Usually both indicators are elevated.
- Auscultation. Listening to sound. Against the background of many defects, specific noises are noted.
- Electrocardiography. The main method for identifying functional disorders by type of arrhythmias. Gives a chance to identify some defects in cardiac structures.
- Echocardiography. Visualization method. It can be used to assess the presence of defects and organic defects. It is considered the main way to identify the described condition.
- MRI. A more accurate alternative to ECHO. It has a relatively high price, but produces high-quality, detailed images.
- General blood test, biochemical. Also for hormones.
It is possible to carry out daily monitoring when registering rhythmic disturbances of the heart.
Reasons for changes
Congenital defects can lead to pathological enlargement of the left ventricular myocardium, for example:
- Mutations affecting genes on which protein production depends.
- Coarctation of the aorta is a narrowed lumen in one of the sections of the vessel.
- Anomaly of overlap between the ventricles.
- The pulmonary artery is absent or its passage is completely closed.
- The narrowness of the aortic valve, which allows blood to flow from the heart into the artery.
- Abnormal structure or dysfunction of the mitral valve, which provokes partial return of blood to the atrium. Because of this, excessive filling of the ventricle occurs during diastole.
Myocardial hypertrophy also develops during life under the influence of certain factors:
- Intense physical training leads to athlete's heart syndrome.
- Addiction to bad habits.
- Sedentary lifestyle.
- Lack of proper rest.
- High load on the heart and nervous system under the influence of constant stress.
- Hypertonic disease. This cause of left ventricular myocardial hypertrophy is the most common. High blood pressure can change muscle tissue.
- Overweight.
- Having a history of diabetes mellitus.
- Cardiac ischemia.
- Atherosclerotic plaques in the aorta that create a barrier to normal blood circulation.
Treatment
Therapy is predominantly conservative. Surgical techniques are prescribed in extreme cases.
Medicines:
- Antiarrhythmic. Amiodarone as the main one.
- Antihypertensives as needed.
- Cardiac glycosides. Restore myocardial contractility. Digoxin and lily of the valley tincture. Others with great caution.
- Vitamin and mineral complexes.
- Products based on potassium (Asparkam), also magnesium.
- Supporters - Mildronate and others.
- Diuretics for impaired renal function. Just not to a pronounced degree, otherwise it can make things worse.
Attention:
All medications are prescribed by a doctor. It will not be possible to choose a safe combination without special knowledge. Harming yourself is okay.
The dosage and specific route to eliminate the condition depend on the stage. Thus, moderate changes in the myocardium are treated routinely, using a group of medications.
Surgical techniques are used relatively rarely, only when indicated. Usually it is enough to fight the root cause of the condition; the symptoms themselves are minimal.
Etiotropic treatment is supplemented in case of pronounced diffuse changes. Cardiac glycosides, antiarrhythmics and others are used.
Surgery is a last resort. But in some cases you cannot do without it. Options include defects of the aorta, coronary arteries, congenital anatomical defects, destruction of the atria and other conditions.
It consists of prosthetics, stenting or ballooning, depending on the nature of the lesion.
A big role is given to lifestyle changes. At a minimum, you need to give up smoking, alcohol, drugs, and normalize physical activity (only walks, no sports, no heavy lifting).
Other measures, including diet, do not have much clinical significance. The diet is adjusted at the discretion of the specialist.
Classification
The classification of hypertrophic changes in the left ventricular myocardium is based on the following signs:
- Area of distribution of pathology.
- The ability to influence the movement of blood through vessels.
- Myocardial thickness.
The increase in the muscle layer often extends throughout the entire cardiac chamber. Then these are diffuse changes in the myocardium of the left ventricle. Also, the lesion may cover individual areas. In this case, it is customary to talk about focal disorders. Most often, hypertrophy is observed in the area of the ventricular septum, in the area of the opening leading to the aorta, at the junction of the atrium and the left ventricle.
Concentric hypertrophic changes
In another way, they are called symmetrical, because the compaction of the muscular layer of the left ventricle develops evenly (symmetrically) along the entire perimeter of this area. At the same time, the chamber cavity becomes smaller. The growth of myocardial cells occurs in order to strengthen the contractility of the ventricle when the movement of blood is difficult due to a narrowed aortic valve or vasospasm.
Eccentric hypertrophy
Its location is the septum separating the ventricles, sometimes its apex or side wall. The development of such changes occurs when the chamber is overloaded with a large amount of blood. In this case, stretching of its cavity is more often observed, which is sometimes accompanied by an increase in the thickness of the myocardium. In this case, the heart muscle is not able to fully pump all the blood into the main artery. Eccentric hypertrophy occurs when the aortic and mitral valves do not function well, or in people who are obese due to poor nutrition.
Based on their ability to influence blood flow, they are divided into:
- disorders accompanied by obstructive phenomena;
- myocardial changes without obstruction (obstruction is an obstacle).
The first case is not typical for hypertrophy of the diffuse concentric type. In this situation, it is possible to detect a bulging of the thick muscle layer into the ventricle, the cavity of the cardiac region narrows and, as it were, splits in two. If such a pathology is found in the place where the aortic mouth is located, pushing blood through the valve becomes even more difficult. Thus, with obstruction, each contraction of the left ventricle is accompanied by compression of the aortic opening.
When pathological processes have affected the septum between the ventricles, it is customary to talk about asymmetric hypertrophy. It may occur with or without obstruction.
The thickness of the altered myocardium can be different:
- Moderate is characterized by sizes from 11 to 21 mm.
- The average thickness is 21-25 mm.
- An anomaly is considered pronounced when the muscle layer of the left ventricle reaches more than 25 mm during cardiac output.
Myocardial hypertrophy creates the prerequisites for the development of systolic and diastolic dysfunction of the left ventricle. In the first case, the contractility of the heart decreases, the stroke volume decreases, and in the second, the filling of the chamber cavity with blood during relaxation worsens. The result of such disorders is inhibition of blood flow within the organ itself, which negatively affects the blood supply to the entire body.
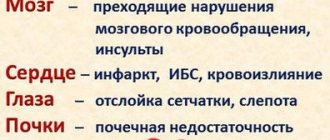
Cardiac ischemia, stroke, heart attack or heart failure are all consequences of hypertrophic changes.
Forecast
Depends on the root cause of the pathology. Diffuse-dystrophic changes in the myocardium are a consequence of metabolic, destructive, inflammatory and infectious conditions.
A minimally favorable outcome is observed against the background of long-term arterial hypertension and severe coronary dysfunction.
When heart failure occurs, the prognosis also worsens and becomes negative. The possibility of surgical treatment significantly improves the chances of survival.
In numerical terms, the average duration of biological existence with minimal deviations or the possibility of full compensation does not differ from that of healthy people.
All violations make the prognosis negative. The term varies from 3 to 15 years or a little more. It is possible to say something specific only after a certain period of observation.
Types of pathological changes
Changes in the structure of the heart muscle are divided into several types depending on the factor that influenced their development.
- Dystrophic changes are detected when the function of energy consumption and supply to the heart muscle is impaired. She begins to lack nutrients, which is why muscle tissue is gradually depleted. The clinical picture is predominantly mild. At an advanced stage, a person may experience increased fatigue and shortness of breath when receiving physical activity.
- Metabolic (dismetabolic) changes occur due to failures of metabolic processes in cardiomyocytes (heart cells). They are mainly caused by heart diseases. Violations are manifested by myocardial hypoxia and disruptions in its functioning. If pathological abnormalities are identified immediately, there is a possibility of reversing the process. In the absence of timely assistance, it is impossible to completely eliminate the damage. The heart muscle will not have time to recover, as a result of which the changes will become irreversible.
- Scar changes occur after experiencing cardiac pathologies in the form of dead areas. Due to myocarditis (cardiosclerosis), they are predominantly diffuse, and a heart attack is characterized by focal damage to the heart. In the first case, the problem concerns the entire organ, and in the second, only a certain part of it. The resulting scar after a heart attack can be small or large. It is localized on one lower, posterior or lateral wall of the ventricle, or on several at once.
- Moderate nonspecific changes in the ventricular myocardium generally do not appear due to diseases of the cardiovascular system and do not actually create discomfort. Experts associate them with failures in the repolarization phase, that is, at the moment of restoration of cardiomyocytes after the passage of an electrical impulse. Emerging stress and endocrine disruptions can affect this process. In mild cases, such changes are reversible and do not harm health. More advanced stages are extremely rare. Due to their nature of occurrence, nonspecific abnormalities are often classified as metabolic.
- Inflammatory changes are predominantly diffuse in nature and can severely damage the heart muscle, which will affect its function. They are detected on the ECG by reduced waves and arrhythmias.
The genesis (reason for development) and localization of the listed types of deviations are different. Based on size, they are divided into diffuse and focal changes in the myocardium. The first type is diagnosed most often. It is characterized by damage to all parts of the heart. Focal deviations are single areas. In both cases, the changed areas are gradually replaced by connective tissue that does not allow electrical impulses to pass through. It will be impossible to reverse the process at this stage.
Provoking factors and symptoms
Any disturbances in the functioning of the heart can be manifested by the following factors:
- frequent shortness of breath after light exertion;
- lack of air;
- constant fatigue, drowsiness;
- decreased performance;
- flickering in the eyes;
- excessive pallor of the skin;
- dark circles under the eyes.
If such conditions are noted, then it is necessary to urgently go to an appointment with a cardiologist. Diagnosis is simple and is often limited only to a cardiogram. This is enough to make a correct diagnosis.
Usually a person feels with left ventricular hypertrophy:
- dizziness;
- weakness;
- shortness of breath;
- swelling;
- chest pain;
- interruptions in the heart.
Symptoms usually increase after exercise and stress. They also intensify during pregnancy.
Treatment for focal and diffuse disorders
In the treatment of myocardial pathologies, various groups of drugs are used:
- Corticosteroid hormones – as an antiallergic agent;
- Cardiac glycosides - for the treatment of diffuse changes in the myocardium, manifestations of heart failure (ATP, Cocarboxylase);
- Diuretics - to prevent edema;
- Means for improving metabolism (Panangin, Magnerot, Asparkam);
- Antioxidants (Mexidol, Actovegin) - to eliminate the negative effects of lipid oxidation products;
- Antibiotics – for anti-inflammatory therapy;
- Drugs for the treatment of concomitant diseases;
- Vitamin preparations.
If conservative treatment does not lead to significant improvements in the condition of a patient with myocardial diseases, he undergoes surgery to implant a myocardial pacemaker.
Basic principles of dietary nutrition:
- The consumption of salt and excess liquid is limited to a minimum;
- Spicy and fatty foods are not recommended;
- The menu should include vegetables, fruits, lean fish and meat, and dairy products.
Myocardial changes detected on the ECG require additional laboratory and instrumental examination . If necessary, the cardiologist will prescribe treatment in a hospital or on an outpatient basis. Timely measures taken will help avoid serious complications.
Source: oserdce.com
Diagnostic and treatment methods
The cardiologist prepares treatment only on the basis of the examination results. If the patient does not have a dangerous heart pathology, then the doctor may advise taking vitamin complexes, especially in autumn and winter, monitoring blood pressure levels and adjusting lifestyle. If there is a suspicion of the secondary nature of changes in the myocardium, that is, development under the influence of other diseases, the following diagnostic methods will be prescribed:
- Donating blood to determine the amount of hemoglobin, checking the level of white blood cells and the erythrocyte sedimentation rate.
- Study of the composition of urine to assess the condition of the kidneys.
- Carrying out a biochemical blood test to determine the level of protein, sugar and cholesterol.
- Conducting 24-hour ECG monitoring with and without exercise to assess the condition of the heart.
- Performing an ultrasound examination of internal organs to check for abnormalities in their structure.
- Study of the heart muscle using an echocardiograph to visualize its parts and determine the cause of myocardial changes.
- The use of electrocardiography (ECG) to detect any abnormalities in the heart's rhythm, as well as in its conductivity and structure.
Having received all the necessary data, the doctor will assess the patient’s condition. If the cause is not only in the heart, then he will advise you to consult with other specialists (endocrinologist, gastroenterologist, hematologist) to develop a comprehensive treatment. An important advantage of a timely course of therapy is the high chance of eliminating pathological changes. In fact, in 90% of cases, myocardial cells are able to recover completely.
If even modern diagnostic methods could not help identify the cause of the problem, then treatment is aimed at achieving the following goals:
- stop the clinical picture of heart failure;
- protect cardiomyocytes and restore their functions;
- normalize metabolic processes in the heart.
The following groups of drugs are commonly used in the treatment of heart failure:
- Cardiac glycosides (Strofanthin, Digitoxin) increase vascular tone, eliminate arrhythmias, reduce the duration of the contraction phase of the heart muscle and improve its nutrition.
- Antiarrhythmic drugs (Amiodarone, Dofetilide) block beta and alpha adrenergic receptors, improve myocardial nutrition and have a coronary dilation effect.
- Diuretics (Lasix, Britomar) reduce venous return to the heart and remove excess moisture from the body, lowering blood pressure.
To stimulate metabolic processes, doctors prescribe the following drugs based on beneficial substances:
- "Cocarboxylase" (coenzyme);
- “Doppelgerts Active”, “Asparkam” (magnesium, potassium);
- “B-Complex”, “Neurobion” (B vitamins);
- "Preductal", "Mexidol" (antioxidants);
- "Riboxin" (metabolic agent).
The following drugs may be required as an addition to the main treatment regimen:
- hypotensive;
- sedatives;
- hormonal (for endocrine disruptions);
- antiallergic;
- antibacterial.
Folk remedies are often included in the treatment regimen for myocardial changes, as they saturate the body with necessary substances and calm the nervous system. The most relevant decoctions of the following herbs:
- hawthorn;
- Melissa;
- motherwort;
- peppermint;
- cranberry;
- peony;
- rose hip.
Maintaining a healthy lifestyle
Comprehensive treatment of any pathology consists not only of taking medications, but also of a properly selected diet. In the presence of moderate changes in the myocardium, it is recommended to adhere to the following rules:
- It is not recommended to overeat or starve;
- the daily amount of salt consumed should not exceed 5 g;
- It is imperative to add vegetables and fruits to your diet;
- the daily menu should contain only low-fat varieties of fish and meat;
- You need to eat 4-5 times a day, and take your last meal 3-4 hours before bedtime;
- It is advisable to completely avoid fatty foods;
- It is recommended to cook by steaming or boiling.
The rules of a healthy lifestyle, which are given below, will help normalize metabolic processes in cardiomyocytes:
- sleep at least 6-8 hours a day;
- to refuse from bad habits;
- try to avoid stressful situations;
- exercise at a moderate pace without overload.
Treatment for focal and diffuse disorders
In the treatment of myocardial pathologies, various groups of drugs are used:
- Corticosteroid hormones – as an antiallergic agent;
- Cardiac glycosides - for the treatment of diffuse changes in the myocardium, manifestations of heart failure (ATP, Cocarboxylase);
- Diuretics - to prevent edema;
- Means for improving metabolism (Panangin, Magnerot, Asparkam);
- Antioxidants (Mexidol, Actovegin) - to eliminate the negative effects of lipid oxidation products;
- Antibiotics – for anti-inflammatory therapy;
- Drugs for the treatment of concomitant diseases;
- Vitamin preparations.
If conservative treatment does not lead to significant improvements in the condition of a patient with myocardial diseases, he undergoes surgery to implant a myocardial pacemaker.
Basic principles of dietary nutrition:
- The consumption of salt and excess liquid is limited to a minimum;
- Spicy and fatty foods are not recommended;
- The menu should include vegetables, fruits, lean fish and meat, and dairy products.
Myocardial changes detected on the ECG require additional laboratory and instrumental examination . If necessary, the cardiologist will prescribe treatment in a hospital or on an outpatient basis. Timely measures taken will help avoid serious complications.
Source: oserdce.com
1) I am three months pregnant. I am 32 years old, this is my second birth. Doctors diagnosed changes in the myocardium of the posterior wall of the left ventricle. I don’t feel any changes myself. Will there be any difficulties later on during childbirth? Will this affect the child's development?
“Changes in the myocardium of the posterior wall of the left ventricle” is not a diagnosis, it is an ECG conclusion. You don't have a diagnosis yet. These changes may be associated with metabolic disorders in the heart, be a consequence of an infection, etc. You will first need to clarify the nature of these changes and the diagnosis before talking about the management of pregnancy and childbirth.
2) I am 12 weeks pregnant. Conclusion on cardiac ultrasound: “CHD: secondary ASD. The cavities of the heart are not dilated. There are no signs of pulmonary hypertension. MVP of the first (3 mm) degree with min. early scientist MR." I don’t know what it is, other than a congenital heart defect. For the first time in 32 years, I heard that I had such abnormalities in my heart. My mother is sure that I grew up to be a healthy child. The cardiologist said that there was “nothing wrong” and I didn’t need to take anything. I am very worried about how the pregnancy will progress in later stages and whether this will affect the child? And is it possible to only detect a heart defect at the age of 30? Maybe everything is not as scary as I pictured. Help me please clarify. The worst thing is not to know or understand something.
I can reassure you. If this is the case, then you have no reason to worry. Your heart defect (atrial septal defect) is one of the most favorable and has virtually no effect on either the course of pregnancy or your health. The only thing, let me remind you that during pregnancy you should not do work that involves lifting weights and get hypothermic. Wish you luck
3) How does the presence of mitral valve prolapse affect the management of pregnancy and childbirth?
4) I have very bad heredity for hypertension and strokes. I am 30 years old, I am 38 weeks pregnant. Before pregnancy, my blood pressure did not bother me, but in the third trimester my blood pressure began to rise frequently, protein was never found in my urine, all blood tests were good, and the baby’s condition was also good. What do you think about my condition? What is the likelihood of preeclampsia?
You really have very bad heredity, especially in terms of the state of the blood vessels in the brain. If blood pressure begins to increase at the end of pregnancy and even with medications it remains at the level of 140/90-150/100, this is not a very pleasant sign. As far as I can tell, you now need diuretics (as antihypertensives and as the prevention of eclampsia, and potassium-sparing ones - veroshpiron or spironolactone) and vasodilators (or ACE inhibitors - these are drugs such as enalapril or fosinopril). Limiting salt is mandatory; this, among other things, also prevents fluid retention in the body, i.e. also prevention of complications. The likelihood of a convulsive syndrome is quite high; monitoring the specific gravity of urine and the amount of protein in the urine, as well as the presence of edema, including hidden ones, is mandatory. But in general, according to the regulations, such a woman should be in the maternity hospital at this time in the pathology department, and in case of complications - immediately: anesthesia and cesarean section.
5) Please advise where to go. I am 26 weeks pregnant and have been diagnosed with mitral valve prolapse. I would like to receive qualified advice from an experienced cardiologist who works with pregnant women
First of all, you need to clarify what degree of prolapse (it comes in three degrees) and whether there is regurgitation (this is even more important). The general rule is this: MVP without regurgitation is considered a variant of the norm, with regurgitation of grade I it is considered clinically pronounced prolapse, with regurgitation of grades II and III - morphologically (i.e. anatomically) pronounced prolapse. So, only morphologically expressed prolapse can entail some significant features in management tactics. In other cases, most often you can limit yourself to advice to protect yourself from colds, reduce physical and nervous overload and avoid overtime work and night shifts.
How to keep your feet healthy if you're constantly on your feet?
Source: serdce-moe.ru
Diffuse changes in the myocardium: what is it and what are the possible causes of the condition
- Myocardial changes on ECG
- Types of myocardial lesions
Cardiovascular diseases top the list of causes of death in the world. Most deaths are due to coronary heart disease. To promptly recognize and prevent heart problems, various diagnostic methods are used, in particular an electrocardiogram (ECG) and ultrasound (echo-CG).
And for patients who have received an ECHO-CG or ECG result that says “diffuse changes in the myocardium,” the question arises: what is this?
The myocardium is the muscular middle layer of the heart containing contractile cells (cardiomyocytes). The coordinated contraction of cardiomyocytes causes the heart to contract and pump out blood. As a type of muscle tissue, the myocardium is unique among all other muscle tissues in the human body.
The thickness of the myocardium determines the strength of the heart's ability to pump blood.
The heart muscle is adapted to be highly resistant to fatigue, so if the patient complains of fatigue, this may indicate problems with the myocardium. Cardiomyocytes have a large number of mitochondria, which allows for continuous aerobic respiration. The heart muscle also has a large supply of blood relative to its size, which ensures a continuous flow of nutrients and oxygen to the heart while allowing for the timely removal of metabolic waste.
The term “diffuse changes” means that the processes occurring in the myocardium do not have features typical of a particular disease. Based on the conclusion alone about diffuse changes in the myocardium, the cardiologist will not be able to make an accurate diagnosis; he will need the results of a physical examination, questioning the patient about disturbing symptoms, as well as data from a blood test and other studies.
Possible causes of diffuse changes in the heart muscle:
- A variant of the norm, that is, the absence of cardiac pathology. For example, in children, diffuse changes without complaints of shortness of breath, heart pain and fatigue are considered normal.
- Hormonal or other types of metabolic disorders in the myocardium.
- Dysfunction of the endothelium (the lining of blood vessels that separates the bloodstream and the deeper layers of the vascular wall).
- Autoimmune neuropathy.
- Abnormal glucose levels.
- The result of exposure to certain drugs, including cardiac glycosides, streptomycin and aminazine.
- Inflammation of the myocardium, also called “myocarditis”.
- Disturbances in water-salt metabolism in the myocardium and in the body as a whole.
- Cardiosclerosis. With this pathology, myocardial muscle fibers are gradually replaced by connective tissue cells. This occurs due to the inflammatory process or metabolic disorders.
- Lack of nutrients (for example, proteins or carbohydrates), as well as vitamins and microelements. This can occur, for example, due to renal failure or chronic enterocolitis.
- Age-related changes in the myocardium. They are often insignificant and asymptomatic.
- Use of drugs and (or) alcohol.
Symptoms of diffuse changes in the myocardium are not specific. If the ECG showed mild diffuse changes, and the person does not complain of symptoms characteristic of heart disease, then they do not focus on these harmless changes.
The doctor does not use the term “diffuse changes in the myocardium” as the final diagnosis and name of a specific disease. For a cardiologist, this is just a diagnostic marker, which is a reason to prescribe additional studies.
Treatment of diffuse myocardial changes is aimed at eliminating the cause of this condition. It is important to restore the functioning of the heart muscle, and for this you should eat well, minimize negative experiences and take a complex of vitamins, which is recommended by the treating cardiologist.
An electrocardiogram is commonly used to detect abnormal heart rhythms and investigate the cause of chest pain. And it happens that after the test the doctor tells the patient that he has recorded myocardial changes on the ECG. What does this wording mean? This is a signal that the heart muscle is undergoing changes. And the doctor’s task is to find out their character. They can be caused by age (for example, myocardial changes are very common in children and the elderly), or by an inflammatory disease. Or perhaps it’s due to intense sports activities. Athletes experience thickening of the myocardial walls. This condition even received a special term - “athletic heart”.
Myocardial change
Electrocardiography is the simplest diagnostic method for studying the functioning of the heart. The essence of the examination is to record electrical impulses that accompany the contractile and restorative functions of the myocardium, called “depolarization” and “repolarization.”
Treatment and prevention of diffuse cardiac changes
There are no universal treatment methods. Treatment is prescribed only after a thorough examination has been carried out and all the causes of changes in the heart muscle have been identified. For each patient, the attending physician prescribes his own regimen depending on the results obtained on the ECG and ECHO-CG. The goal of the course of treatment is to localize and eliminate the causes that led to the disease.
Treatment and prevention regimens include:
- correction of diet and composition of food;
- correction of the patient’s daily routine;
The choice of treatment method depends on what exactly causes these changes in the heart muscle
- creating conditions for normalizing a person’s emotional state;
- correction of the intensity of physical activity;
- giving up alcohol and smoking;
- review of medications when the patient is simultaneously undergoing treatment for other diseases;
- prescribing a course of vitamins and potassium;
- taking medications that improve the conductivity of the heart muscle;
- prescribing medications to eliminate spasm of the vascular bed and prevent heart failure;
- regular examination and observation by a cardiologist.
One of the important components of treatment is proper nutrition of the patient. It must be regular. Fasting is not allowed. The diet should include: low-fat protein foods, seafood, vegetables rich in potassium, dried fruits. Boiled and steamed dishes are recommended. It is necessary to reduce salt intake.
Under no circumstances should you self-medicate or use treatment regimens prescribed to other patients as a basis, even if they have similar symptoms and research results. Negligence in treating a disease is also unacceptable. This can lead to worsening of the disease and the development of heart failure.
A healthy diet consisting of whole grains, vegetables and fruits, legumes, low-fat dairy products and fish
Diffuse changes in the myocardium are characteristic not only of older people. But this is not always a cause for serious concern. Often changes appear as a result of past illnesses or under the influence of third-party negative factors. In the early stages and with minor deviations, the process of diffuse change can not only be stopped, the heart muscle can be returned to its original healthy state.
Effective prevention of the disease is maintaining a healthy lifestyle. Regular walks and moderate physical activity promote better blood circulation and increased oxygen supply to all tissues. Maintaining an optimal weight, a balanced diet, including a complex of vitamins and microelements vital for the body, are necessary to reduce the load on the human body as a whole. Giving up unhealthy habits will prevent not only cardiovascular but also other diseases.
- For 1 liter of water take 6 tablespoons of dried fruits;
- bring to a boil and cook for 10 minutes over low heat;
- let the broth brew for about two hours;
- take 150 ml before meals.