What is cerebral gliosis
The natural process of replacing dead neurons, which is protective in nature, is called gliosis of the white matter of the brain. Normally, over 10 years in a healthy body, about 4% of all neurocytes are destroyed, so gliosis is one of the manifestations of aging.
With the development of pathological processes that cause the death of a large area of nervous tissue, gliocytes replace dead impulse cells, although they cannot generate and conduct nerve impulses. Thanks to this, the spread of the pathological process slows down, and the metabolism of the affected area is preserved in full.
What causes the development of gliosis of brain tissue, what it is and at what point the process becomes dangerous
The CNS includes three types of cells:
- Neurons are the main functional cells of the nervous system, forming and transmitting impulses from the brain to effectors (executive organs that provide a response to a specific stimulus).
- Ependymal cellular elements lining the ventricles of the brain and the central spinal canal.
- Cells of glial tissue with supporting and protective functions. They form a scar after the death of neurocytes for various reasons, including due to demyelinating diseases.
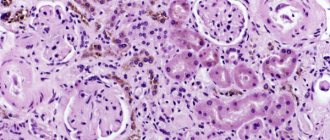
Glial tissue (neuroglia) is located between the functional elements and is the support for all cellular structures. Normally, it protects the brain from injury due to sudden movements, as well as from the development of infectious processes.
Making up about 40% of the volume of all tissues of the skull, glia creates the conditions for the normal functioning of the nervous system. In critical situations, it forms a kind of scar, which does not allow metabolic processes to stop and partially takes over the tasks of other cells. In addition, neuroglia participate in the formation of new nerve fibers that isolate the lesion and protect healthy tissue.
Diagnostic methods
This pathology is easily confused with other diseases and traumatic changes. It is very important to accurately establish the reasons that provoked the degeneration of brain tissue. For this purpose, instrumental methods are now widely used:
- EEG. It will help identify disturbances in the functioning of neurons. This study is prescribed if brain activity is impaired. The diagnostic procedure detects abnormal seizure activity, which helps prevent new seizures.
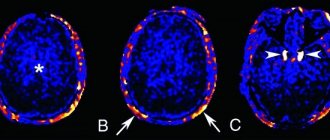
- Tomography (CT, MRI). It will visually show the state of the brain and help determine the extent and location of damage. Tomography can easily identify diseases of vascular origin. MRI records impaired metabolism, scars, tumors, etc. MRI can diagnose white matter gliosis in the frontal lobes. This process cannot be detected by other methods. It is MRI that makes it possible to detect periventricular gliosis, which affects areas near the ventricles of the brain. This method also helps to diagnose peripheral and perifocal lesions.
These methods also make it possible to identify the source that provoked the pathological changes.
Gliotic changes in the frontal lobes are often observed in old age. There are no associated pathologies.
Symptoms
Clinical signs of neurogliosis depend on the underlying disease that caused its development. Single small lesions do not cause specific symptoms and are detected during MRI for another disease. The following symptoms cause concern:
- headaches that develop for no apparent reason, are long-lasting, of high intensity and do not go away after taking antispasmodics;
- unstable blood pressure (sharp decrease or increase in blood pressure within a short time);
- periodic dizziness;
- increased fatigue and decreased performance;
- emerging changes in auditory and visual perception;
- memory and attention disorder;
- the occurrence of motor disorders (with large lesions, up to convulsive conditions).
There is a direct dependence of clinical manifestations on the location of the focus of gliosis
- Supratentorial gliosis is manifested mainly by visual disorders - distortion of the size, shape and outline of objects, hallucinations, loss of visual fields, inability to recognize an object by appearance.
- Damage to the temporal lobes is characterized by prolonged and frequent headaches. If the lesion is vascular in nature, then the pain syndrome is accompanied by sharp changes in blood pressure.
- Gliotic changes in white matter can cause dizziness, increased seizure activity and the development of epileptic seizures. More often, such symptoms develop as a result of traumatic brain injuries or as a complication of surgery.
- The localization of the lesion in the frontal lobes in most cases is an age-related change. If there were no diseases that could activate the proliferation of glial cells, the process refers to the primary pathology:
- developing in older people
- manifested by impaired memory and attention, slowed reactions, and imprecise fine motor skills.
In the absence of adequate treatment of the underlying disease, glial lesions increase in size. This leads to the progression of clinical manifestations and the development of complications.
Causes
White matter gliosis develops as a result of ischemia, physical damage, and inflammation. Possible causes of the disorder include:
- Meningitis. Infectious tissue damage.
- Encephalitis. Another option, only the pathogen is completely different. But the results are approximately identical. Without treatment - severe degeneration and disability. And perhaps death from complications.
- Intoxication. Poisoning by poisons. Vapors of non-metals and other compounds.
- Ischemia. As a result of a stroke or encephalopathy.
- Injuries.
- Features of heredity. Patient genetics.
The cause can be determined quickly enough to begin treatment. But it will not be possible to eliminate degeneration that has already occurred.
Causes of gliosis
Gliosis is not an independent disease; it is a morphological manifestation of a number of pathologies. The reasons that caused the accelerated proliferation of neuroglial cells may be:
Genetically determined diseases
- lysosomal storage disease (Tay Sachs disease), characterized by the death of a large number of neurons in children from six months of age;
- tuberous sclerosis, manifested by the formation of multiple benign tumors in various organs;
- multiple sclerosis – demyelination (destruction of the covering myelin sheath) of nerve fibers of various parts of the central nervous system.
Congenital and intrauterine pathologies
The cause of the appearance of foci of gliosis in the white matter of the child’s brain in this case is:
- oxygen starvation (hypoxia) during fetal development or childbirth;
- birth injuries of varying severity;
- increased levels of carbon dioxide in the blood (hypercapnia);
- infectious diseases transmitted in utero.
Causes of the disease
Even the most common diseases can cause glial changes in the brain. The more destruction affects the nerve fibers, the more extensive the gliosis focus will be formed.
Cause the formation of gliosis:
- Episyndrome.
- Hypertonic disease.
- Multiple sclerosis.
- Diabetes.
- Hypoxia.
- Circulatory disorders.
- Anemia.
- Encephalopathy.
- Brain swelling.
The causes of gliosis may also lie in:
- Heredity.
- Birth injuries.
- Old age.
- Excessive consumption of light carbohydrates and fatty foods.
Gliotic foci can be isolated in the case of neuronal death that occurs during the aging process. In this case, specialists, using medications, try to help the patient not to lose the vital functions of the nervous system. There is an opinion that it is the glia, which fill the interneuron spaces and are responsible for protective, metabolic and transport functions, that at a certain point begin to secrete a substance that destroys neurons. Such changes in the body become the main cause of aging.
In addition, scientists believe that gliosis can develop as a result of brain injury, excessive consumption of large doses of alcohol, or taking drugs that contribute to the gradual death of neurons.
Forms and degrees of development
According to morphological characteristics:
- isomorphic form of gliosis – characterized by ordered proliferation of neuroglia;
- anisomorphic type of disease – characterized by a predominance of cellular structure and chaotic growth;
- fibrous form – signs of a predominant fibrous structure are clearly expressed.
Based on the nature of the process and its prevalence, they speak of:
- The focal type of the course is a limited area of gliosis (usually in the parietal or temporal lobes), the cause of which was trauma, an infectious or inflammatory process.
- Diffuse type of course – multiple lesions of various sizes and locations. Cystic-gliotic formations of vascular origin are often found.
Depending on the location of the foci, gliosis is divided into:
- Periventricular gliosis - glial proliferations are localized in the area of the ventricles of the brain.
- Perivascular location of foci (vascular gliosis) is the most common type of course. It is distinguished by the presence of glial growths along atherosclerotic vessels. Diagnosed as microangiopathy with the presence of single or multiple foci of gliosis. The variety is the subtentorial type (a few lesions appear as a result of birth injuries or age-related changes, and multiple lesions arise as a consequence of circulatory disorders).
- Subependymal - single lesions localized on the inner lining of the ventricles.
- Marginal - foci of glial degeneration are located in the intrathecal region.
- Marginal - areas of replacement glial tissue are located on the surface of the brain.
Classification
The pathological process can be divided according to 4 criteria. The first and least understandable to the average patient is the structure of the cells that replace neurons.
According to cell structure
Glia, as already mentioned, are very heterogeneous. You can find different types of cells. The most numerous are the so-called astrocytes. They got their name for their resemblance to a star.
These cytological units differ in structure and, partly, in functionality.
- There are fibrous cells. Which have very long shoots.
- There is a protoplasmic variety. Large and meaty.
Accordingly, based on which structures mainly predominate in the affected area, the following are distinguished:
- Anisomorphic gliosis. Most of the local cells are protoplasmic astrocytes. At the same time, tissue growth is very unsystematic and chaotic.
No clear distribution pattern can be identified. Therefore, scattered foci of gliosis are possible. This is not good because different parts of the brain will be involved.
This means that the symptoms of neurological deficits and disorders will be more complex and multifaceted.
- Fibrous form. Occurs more often. Growth has clear boundaries and is understandable in terms of distribution. As the name suggests, the basis of the lesion is made up of such astrocytes. The clinical picture concerns mainly one area. Unless a huge area will be affected.
By number of outbreaks
The second classification criterion is the number of lesions. Accordingly, they distinguish:
- Diffuse form. As the name suggests, there are several points of attack. The pathological process can affect both the brain and the spinal cord. Often, this occurs against the background of an inflammatory process, severe toxic damage, or ischemia. It is necessary to examine the situation and the patient in detail.
- Focal variety. One area of the brain is affected. For example, part of a share. Sizes may vary. The point is that the cells are destroyed along one perimeter. On an MRI, such areas appear as white spots. Images are enhanced after administration of gadolinium.
Since there is only one point, there are fewer symptoms. Usually. There are exceptions. The outbreak can be huge. If it affects several areas of cerebral structures at once, the clinic will be appropriate.
By localization
The third basis for classification is the localization of the pathological process.
- Subependymal location. The focus is located in the region of the ventricles of the nerve tissue.
- Regional localization. The changes are located under the outer shell of the cerebral structures.
- Perivascular location. Found around a modified vessel. Most often, the pathological process develops after suffering from vasculitis, other damage to large main arteries (or small ones, it also happens that capillary networks are also targeted).
The supratentorial foci of gliosis stand apart, that is, located near the cerebellum; the pathological process develops after bruises, injuries and produces pronounced disturbances in the functioning of the extrapyramidal system: dizziness, coordination disorders, nausea, and others.
By severity
Finally, the condition can be subdivided according to the overall severity of the pathological process. This is not a generally accepted option, but it is widely used in one variation or another.
In total, we can name 4 forms of violation on this basis:
- Zero. First stage. The changes are minimal, there are almost none. Therefore, there are practically no symptoms.
- First. The clinical picture is already present, but weakly expressed. In the form of isolated signs of a pathological process.
- Second. The violations are noticeable. The disorder is accompanied by a clear group of focal symptoms.
- Third. Final degree. Due to the size of the changed area or the severity of the pathological process, a well-defined clinic is present. Plus, a neurological deficit that disables the patient. Fortunately, this option is relatively rare.
Foci of gliosis in the brain are the result of ischemia, dystrophy, mechanical damage, intoxication and other processes.
These classifications do not take into account the origin of the disorder. Therefore, when choosing a treatment strategy, you must also keep in mind the etiology of the problem.
According to the structure of the hearth itself
There are other reasons for classification. For example, according to the structure of the outbreak.
Highlight:
- Cystic-glial changes in the brain, which are accompanied by both the proliferation of glia and the formation of fluid-filled sacs.
- Solid areas. Homogeneous in structure, consist only of healthy tissues.
All classifications are used to more accurately describe the problem.
Foci of gliosis
Areas of neuroglial proliferation are a kind of scars at the site of dead neurons; they can be single, include up to 3 glial foci (few lesions) or multiple. The size of the growths can be calculated using the formula: the number of functioning neurocytes to the number of glial cells / per unit volume of tissue. Normally, this figure does not exceed 1:8/10.
With an increase in the number of gliocytes, the functioning of the central nervous system is disrupted, up to a convulsive syndrome. Neurologists believe that such a disruption of the central nervous system is often caused by subtentorial foci of gliosis of vascular origin or subcortical (subcortical) foci.
Single outbreaks
Small foci of gliosis do not cause symptomatic manifestations.
In a child, they are formed as a result of trauma received during childbirth, and the tissue of any lobe of the brain can be damaged.
But more often, single areas of glial changes are localized in the left or right parietal lobe.
In adults, the development of single foci of gliosis is caused by age-related changes or diseases of the central nervous system. Such areas practically do not change over time, therefore, in most cases, they cannot be identified without special examinations.
Multiple lesions
Multiple focal changes in brain tissue, as a rule, develop as a result of acute or chronic circulatory disorders. Forming foci of gliosis enhance the clinical picture of the disease that caused them.
Multiple foci of subtentorial gliosis of the brain appear as a result of traumatic brain injuries and hemorrhages in the tissue under the cerebellar tent. This zone is vulnerable due to the surrounding incompressible spaces filled with cerebrospinal fluid.
Multiple focal changes in the brain substance of a dystrophic nature develop with insufficient blood supply, chronic diseases of the central nervous system, and also as a result of age-related changes.
Treatment of gliosis
There are no specific medications, vaccines, diets, or any other treatments that provide successful treatment for cerebral gliosis. Neuroglial cells appear as a result of the development of another disease that affects the brain. Therefore, it is important to find it and eliminate it.
If the main cause of death of nervous tissue is the aging process, then it is necessary to carry out a number of preventive measures to inhibit the further development of brain gliosis. Medicines used:
- Medicines that improve brain function.
- Means that normalize the blood circulation process.
- B vitamins.
For hypertension, medications are prescribed to lower blood pressure.
Which doctor should I contact?
If you suspect the presence of gliosis, you should consult a neurologist. After the studies have been carried out, consultation with specialists may be required to confirm the diagnosis and determine treatment tactics:
- cardiologist - if gliosis of vascular origin is suspected;
- general practitioner or family doctor - to determine chronic diseases;
- endocrinologist – for diabetes mellitus;
- neurosurgeon - if surgical treatment is necessary.
In children, a neonatologist can suspect the development of glial changes during the first month after birth. Later, developmental changes are identified by a pediatrician who will refer the child to a consultation with a pediatric neurologist.
Traditional medicine
A person can live for a long time without realizing that he is developing such a disease. However, it is dangerous to let the development of gliosis formations take their course. Severe degrees of the disease are difficult to cope with. There is no medicine that removes the accumulation of neuroglia. Gliosis is treated based on the correction of the underlying pathology; such management of the patient will show the doctor the effectiveness of his actions.
To improve the human condition, traditional medicine goes in three directions:
- Preventive.
- Medication.
- Surgery.
Preventive
An adult organism at an early stage of pathology itself struggles with pathological changes. You must follow your doctor's recommendations.
Medication
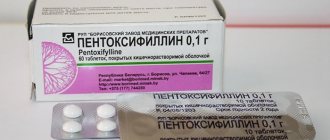
The attending physician will prescribe medications against the disease that causes the growth of glial tissue. These are drugs aimed at strengthening the walls of arteries, drugs that increase brain activity. Medicines to improve conduction along nerve fibers. The vascular etiology of gliosis requires the use of medications that improve the elasticity of the vascular walls.
Drugs used in drug treatment:
- improve blood circulation, nourish brain tissue - Actovegin, Vinpocetine, Cavinton, Cinnarizine;
- prevent platelet aggregation, strengthen arterial walls - vitamin complexes, medications with aspirin;
- increase the resistance of nerves to external influences of nootropics - Piracetam, Phezam;
- lipid-lowering drugs - these are statins, fibrates, they stop the growth of glial tissue; analgesics – relieve headaches.
Surgery
Applicable in exceptional cases. Indications for neurosurgical intervention are convulsive and epileptic seizures, serious disorders of the functioning of internal organs that depend on nerve conduction. Neoplasms and excess cerebrospinal fluid formed by glial disorders are surgically removed. During the operation, the neurosurgeon determines the need for vascular bypass.
Attention! The presence of multiple lesions is a contraindication to surgical intervention; such patients take medications prescribed by doctors for life.
Diagnostics
Cystic-glial changes in brain tissue can only be detected through special studies. Methods for instrumental diagnosis of gliosis include:
- EEG - severe gliosis can provoke the appearance of epileptic seizures. Therefore, if there are changes in brain activity, an electroencephalogram is performed.
- Computed tomography with contrast – using angiography, deviations in the functioning and structure of cerebral vessels are determined.
- Magnetic resonance imaging is the most accurate method for diagnosing various types of disease. Thanks to the results of MRI, it is possible to determine the presence of foci of demyelination, volume, location and cause of glial changes.
- To determine gliosis in the fetus up to 20 weeks, amniocentesis is performed.
Definition of pathology
Organic lesions of brain tissue are often accompanied by cystic changes. Pathological processes occurring in brain tissue lead to changes in its structure. Transformation of the structure is manifested by a decrease in the number of fibers, damage to myelin, a change in the volume of intercellular space, and the replacement of neurons with glial cells.
Cystic-glial transformation, which occurs in the brain, is a process during which neuroglial proliferation occurs, which is usually associated with damage and death of neurons. The mechanism of compensatory replacement of damaged nervous tissue is a protective reaction of the body, which tries to restore lost areas of the brain matter and their functions.
Cystic-glial growths also play the role of a protective barrier that separates healthy tissue from the pathological focus - tumor, abscess, necrosis. The formation of cystic areas interferes with normal blood flow, which can provoke ischemic and atrophic processes in nearby tissues.
Treatment
There is no specific therapy for gliosis. Treatment methods depend on the underlying disease that caused the death of neurons. Main goals of therapy:
- slow down the progression of the process;
- ensure normal trophism of central nervous system tissues;
- eliminate oxygen starvation;
- normalize metabolic processes.
Traditional medicine
To eliminate the symptoms of brain changes, the following groups of drugs are prescribed:
- Vasoactive - drugs that activate cellular metabolism and improve tissue trophism (Cavinton, Vinpocetine).
- Antiplatelet agents are drugs that slow down platelet sedimentation (all derivatives of acetylsalicylic acid).
- Agents that improve the condition of the walls of small and large arteries (Ascorutin, vitamins).
- Nootropic substances - they increase the resistance of the central nervous system to the effects of negative factors (Piracetam, Nootropil).
- Statins – have lipid-lowering properties, preventing the development of atherosclerosis (Fenofibrate, Atorvastatin).
- Painkillers and antispasmodics to relieve headache attacks.
Surgery
Surgery for gliosis is prescribed extremely rarely.
Only for single large lesions. After surgery, treatment of the underlying disease that caused the death of neurons must be continued to avoid the development of relapses.
Indications for surgical intervention for a large single lesion are:
- violation of the outflow of fluid (CSF);
- convulsive seizures caused by a large area of gliosis;
- diagnosed neoplasm;
- changes in the functioning of internal organs.
With multifocal gliosis, only constant conservative treatment has a positive effect.
Complementary and alternative methods at home
Traditional medicine methods can be used only after consultation with a neurologist. Homeopathic remedies are prescribed as concomitants against the background of conservative therapy.
Decoctions and infusions of medicinal plants and fruits improve the functioning of the cardiovascular system and stimulate metabolism.
Diet for gliosis changes
The diet for gliosis is aimed at:
- Improving brain function and relieving vascular spasms. To achieve this result, you need to eat foods rich in magnesium: buckwheat, pearl barley, corn cereals, nuts, pumpkin seeds, lentils, cabbage of all varieties, figs.
- Relieving edema, improving heart function - foods with a high potassium content are introduced into the diet: citrus fruits, green vegetables and fruits, dried fruits, mushroom and potato dishes.
- Weight loss - to control body weight, remove baked goods, canned food, carbonated sweet drinks, smoked foods, fatty meats, fast food and semi-finished products from the daily diet.
The daily diet consists of fish, lean meat, cereals, fermented milk products, hard cheese, vegetables, nuts and fruits. It is better to steam, boil or bake foods.
Treatment methods
Treatment of gliosis is aimed at eliminating the causes of the pathology - first of all, treatment is carried out for the primary disease that affects the structures of the brain. There is no specific treatment for gliosis changes. Depending on the indications, medications are prescribed, and surgery is performed less frequently.
The diet involves reducing the amount of animal fats, salt, and refined sweets in the diet. Among the foods that nourish nerve cells, it is worth noting seeds, nuts, sea and river fish, vegetables, and fruits. Nutrition for cerebral gliosis should be complete and balanced.
It is important that the diet contains foods rich in polyunsaturated fatty acids, plant fiber, vitamins, especially group B, and microelements. Multiple foci of gliosis detected during the study of brain structures, regardless of size, require dynamic monitoring. The frequency of control studies is prescribed by the attending physician.
Drug therapy
The attending physician will tell you how to treat cerebral gliosis, based on the results of a diagnostic examination, taking into account the primary pathology, the patient’s age and symptoms. Essential medicines:
- Nootropic. Protect neurons from damage, stimulate metabolic processes in nerve cells.
- Regulating cerebral blood flow. Drugs that normalize the activity of the circulatory system that feeds the brain.
- Antioxidant. Drugs that prevent oxidative reactions in nervous tissue.
- Antihypertensive. Medicines that normalize blood pressure.
In parallel, depending on the type of primary disease and symptoms, medications are prescribed to eliminate neurological symptoms. This group includes anticonvulsants, antiepileptics, painkillers, and antiemetics.
Surgical intervention
Surgical treatment is resorted to when it is impossible to maintain the patient’s well-being with medications. Surgical treatment of gliosis is indicated under certain conditions:
- Single, large lesions.
- The presence of severe neurological symptoms - convulsive syndrome, epileptic seizures, serious impairment of motor activity and mental activity.
- The patient's age is not older than 60 years.
- Mass effect (negative impact of education on surrounding healthy brain structures).
During the operation, areas of cystic glial tissue that cause symptoms and disorders are removed. Treatment must be comprehensive and timely.
Folk remedies
Treatment of gliosis affecting the brain with folk remedies is ineffective. Traditional methods include taking decoctions, infusions, and tinctures prepared from medicinal plants that have antihypertensive and anti-inflammatory properties. Homemade preparations are shown that improve blood supply to the brain, prepared on the basis of hemlock, clover, and dioscorea.
Among the useful medicinal plants that eliminate inflammatory processes, strengthen the immune system, and improve metabolism, it is worth noting black cumin, hare cabbage, mantle, chinwort, yarrow, wheatgrass, and soapwort. Traditional healers recommend a tincture prepared from valerian root, mint, peony and motherwort, and hawthorn berries as a general tonic, sedative, and immunostimulating agent.
Complications and consequences
The presence of extensive areas of replacement of neurons with gliocytes threatens with dangerous consequences:
- persistent headaches that cannot be controlled by medications;
- mental disorders;
- permanent loss of speech, vision or hearing;
- convulsions and epileptic seizures;
- paralysis (partial or complete);
- mental disorders;
- impaired coordination of movements;
In extremely rare cases, gliosis of non-genetic origin causes death.
Kinds
At the site of necrosis, space begins to become free for the proliferation of neuroglia, forming islands of gliosis.
Types of gliosis depend on its form, nature and localization of distribution:
- Vascular gliosis, also called perivascular, is the most common type of gliosis. In this type, glia grow around vessels that are affected by atherosclerosis. It has a subtype - supratentorial gliosis.
- The marginal variant of gliosis is gliosis, with a clear location in the intrathecal region.
- Anisomorphic variety - foci of gliosis are located chaotically (unlike the previous type).
- Isomorphic type - with this type, the arrangement of glia fibers has a certain correct sequence.
- Subepindymal form - single islands of gliosis appearing on the inner surface of the ventricles.
- Marginal lesion - glial islands grow in the outer part of the brain.
- Diffuse gliosis is multiple lesions of the central nervous system.
- Fibrous gliosis – islands of gliosis in the form of fibers.
Foci of gliosis according to their number are divided into: single, few (no more than 3) and multiple.
Among the causes of a single lesion are trauma during childbirth or the patient’s advanced age (in this case the process is considered natural)
Single islets usually do not grow, which is why they are often an accidental finding during diagnosis using high-precision equipment.
Numerous foci of gliosis are often the result of acute (stroke) or chronic (atherosclerotic lesions, vascular compression, atrophy of central nervous system tissue) cerebrovascular accidents. This is how vascular gliosis is formed, which aggravates the clinical picture of the underlying diseases (attention is impaired, dizziness appears, the head begins to hurt, pressure surges occur, etc.). Consequently, the cause of perivascular gliosis is stroke and chronic cerebral vascular disease, which in turn also have reasons for their appearance.
A separate type of vascular gliosis is supratentorial gliosis - the proliferation of neuroglia near vessels affected by atherosclerosis. It is located under the cerebellar tent - a process of Dura mater, located between the cerebellum and the occipital lobe. This location and presence around incompressible spaces with cerebrospinal fluid determines the vulnerability of the occipital lobe both in case of traumatic brain injury and trauma during childbirth, and in relation to the proliferation of vascular gliosis.
Single islands of gliosis are often asymptomatic and discovered accidentally during diagnosis (MRI, angiography), but with the development of gliosis (proliferation of glial cells, the emergence of new foci, atrophy of brain tissue), it begins to manifest itself clinically.
There are the following symptoms of cerebral gliosis that should not be ignored:
- Unbearable constant headache. At the same time, antispasmodics do not bring relief.
- Changes and episodes of falling blood pressure.
- Frequent dizziness, decreased performance.
- Decreased hearing and vision.
- Deterioration of attention and memory.
- Movement violation.
It is worth saying that the symptoms and signs of gliosis greatly depend on the location of the lesion:
Gliosis of the frontal lobes often occurs in old age, because is a consequence of the aging of the body. In this case, gliosis is a primary disease if there were no factors that could provoke it. Gliosis may explain memory loss, imprecise movements and slow reactions in older people.
Post-traumatic gliosis causes very intense, frequent headaches. Such pain in combination with pressure surges can also occur with gliosis of vascular origin.
The occurrence of epileptic seizures and increased convulsive readiness of the brain can occur with severe damage to the white substance of the brain by gliosis. Dizziness and seizures can often occur as a result of TBI and surgery.
Supratentorial gliosis causes visual impairment (impossibility of recognizing objects, loss of parts of the visual fields, the contours and sizes of objects are distorted, visual hallucinations occur).
Prevention
In order to prevent the spread of outbreaks, you must follow a few simple rules:
- lead a healthy lifestyle with feasible physical activity;
- adhere to the diet chosen by the nutritionist;
- to refuse from bad habits;
- observe the work and rest schedule;
- follow all doctor's orders.
The replacement of dead neurons with gliocytes is a physiological compensatory process that ensures the functionality of the brain in case of non-critical damage. However, the appearance of areas of gliosis indicates the presence of other diseases that threaten the health of the central nervous system, which must be treated promptly and in full.
Etiology of the disease
Gliosis is the accumulation of glial cells in some parts of the central nervous system or eye. Proliferation of glial cells is observed in areas that have been damaged by disease or injury.
Epiretinal gliosis takes a special form here: collagen cells accumulate in the border zone between the retina and the vitreous body. Most of them originate from Müller cells in the retina. Because of its anatomical location, epiretinal gliosis is the only visible form of the disease.
Glial cells constitute a non-neuronal component of the CNS, outnumbering neurons. According to the anatomical classification, differentiation is made into two main groups: macrogliosis and microgliosis.
Astrocytes are glial cells that are primarily responsible for tissue responses to injury. Macrogliosis involves the proliferation and hypertrophy of astrocytes through complex molecular and cellular pathways.
What does cerebral gliosis look like?
Microgliosis mainly occurs if the stroke is caused by an infectious disease - encephalitis, for example. Microglial cells that are not of neuroepithelial origin are likely to be derived from monocyte or macrophage precursors.
ethnoscience
At an early stage of development of gliosis, folk remedies can be used. Here, herbal infusions are used that activate blood circulation and brain function, which, along with taking medications, folk remedies provide additional support to the body to improve human well-being.
The initial degree of gliosis with small lesions requires the use of herbs that stabilize metabolic processes and blood supply to brain tissue. If a person also suffers from obesity, he must spend days of fasting and fasting. They cleanse the body of harmful substances that lead to dysfunction.
Important! There will be no long-term effect from taking medications and folk remedies if the causes of gliosis are not eliminated.
To inhibit sclerosis:
- Cahors tincture . Directions for use: 400 g of crushed 5-year-old aloe leaves are mixed with 650 mg of honey and 650 g of red Cahors. Infuses in the dark for 5 days. Directions for use: drink 1 tsp. 3 times a day before meals. Course – 2–4 weeks.
- Infusion of dill seeds with valerian. Method of preparation: 2 tbsp. l. dill seeds are mixed with a glass of crushed valerian root, 1 liter of boiling water is poured. Let it sit for a day and strain. Add 1.5-2 cups of honey. Directions for use: drink 1 tbsp before meals. l. 4–6 weeks.
- Hawthorn infusion. Hawthorn berries are poured into a 1 liter thermos, 15-20 fruits; are poured with boiling water. Let it sit overnight and strain. Directions for use: drink infusion 1 tbsp. l. ½ hour before meals, 1.5 months.
Remedies can be made from clover and hemlock grass. Or purchase ready-made pharmacy preparations. Medicinal plants will not get rid of pathology, but will soften its manifestations.
Causes of occurrence.
Provoking factors include:
- Diseases of the brain of an infectious nature.
- TBI.
- Surgical interventions.
- Inflammation in the brain.
- Vascular disorders accompanied by deterioration of blood circulation.
- Strokes and heart attacks.
- Chronic alcoholism.
- Diseases leading to atrophic changes (eg, multiple sclerosis).
- Heredity - deviations in lipid metabolism are fraught with disturbances in the functioning of the central nervous system.
There are cases of intrauterine development of pathology.