Causes of intraventricular hemorrhage
The factors that lead to this pathology are completely different in children and adults. For newborns this is the immaturity of the nervous system, at an older age it is the abnormal structure of blood vessels, and for older people a common cause is atherosclerosis.
In newborns
Penetration of blood into the ventricle or under the layer of tissue covering it from the inside (ependyma, lining) occurs in infants under the following conditions:
- premature birth;
- long waterless period;
- severe oxygen starvation at birth;
- damage during obstetric care (forceps);
- body weight below 1 kg.
It consists of immature nervous tissue and thin capillaries, the walls of which have only one layer. Such formations are located around the lateral ventricles of the brain and disappear over time, turning into mature neurons and vessels. If the baby is born prematurely, this structure can form a periventricular hematoma, from which blood enters the ventricles.
And here is more information about cerebellar stroke.
The causes of vascular rupture in childhood are blood clotting disorders - hemorrhagic diathesis, hemophilia, as well as various vascular anomalies:
- arteriovenous malformation;
- aneurysmal dilatation of the artery;
- inflammation of the vessel wall of infectious or autoimmune origin.
Arteriovenous malformation is one of the causes of intraventricular hemorrhage in children
In adults
For mature and elderly people, vascular diseases - atherosclerotic changes, arterial hypertension - come to the fore.
Often the cause of intraventricular hemorrhage is long-term use of blood thinners, cerebral amyloidosis, smoking, chronic alcoholism, tumor destruction of the arteries, and diabetes mellitus. These diseases lead to thinning of the walls of blood vessels, increased fragility and subsequent rupture.
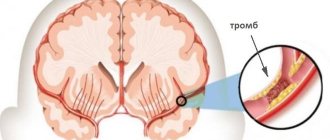
Atherosclerosis is the cause of intraventricular hemorrhage in adults
Classification of intracerebral intraventricular hemorrhage
There are three main types of disease based on the site of blood penetration:
- under the lining of the ventricles (subependymal);
- into the lateral ventricles;
- into the ventricles and brain matter.
Also, depending on the location, the hemorrhage can be in the lateral or third, fourth ventricles of the brain. If blood gets into the lateral cavities, then after they are filled it can move into the third, then into the fourth ventricle. Such massive bleeding leads to a significant increase in cerebral volume and has extremely unfavorable consequences; an isolated breakthrough into the lateral cavities is less dangerous.
Depending on the degree of blood filling, four stages of disease progression are distinguished:
- Blood is found only under the ependyma (lining).
- Half filled, no cavity expansion.
- More than 50% filling with lumen expansion.
- In addition to complete filling of the ventricle, there is damage to the surrounding nervous tissue (parenchymal bleeding).
Classification
The condition is divided according to three bases. The first criterion is the localization of the violation. The most common variants of the disorder are:
- Lateral.
- Lobar.
- Subcortical or subcortical.
- Thalamic.
- Cerebellar.
- Mixed.
- Stem.
Most likely, this terminology will mean nothing to a patient without special knowledge. The point is different. Depending on the location of the pathological change, the symptoms will be one or another. Plus, prognoses are determined by the essence of the disorder and its location. You need to clearly know where the hemorrhage occurred.
Another basis for classification is the type of lesion.
Highlight:
- Actually parenchymal process. When blood enters the brain tissue and permeates it. It is considered a very dangerous type of disorder. Potentially more lethal than the second one.
- Subarachnoid hemorrhage. Liquid connective tissue extends into the space between the cerebral membranes. The main pathological effect concerns compression of the brain, as a result of increased intracranial pressure.
However, the risks are less. Since there are not as many factors of damage as in the first case.
The third basis for classification is the severity of the pathological process.
These options are called:
- Mild degree. If the amount of bleeding into the brain is minimal. Happens quite often. In some cases, the patient does not understand at all what happened until neurological disorders increase. The outlook for recovery is good.
- Average degree. There is a pronounced clinical picture. Everything is noticeable from the very first second of the pathological process. Deviation requires urgent hospitalization and treatment in an intensive care unit. Even in this case, the chances of recovery are rather dim.
- Severe form. Doesn't bode well for the patient. In more than 80% of cases, a person dies from massive death of brain tissue. In 20% of situations he remains deeply disabled for the same reasons. There is almost no chance of restoring at least the basic functions of cerebral structures and ensuring adequate life activity.
These classifications are actively used in medical practice to describe the pathological process, its essence and dynamics.
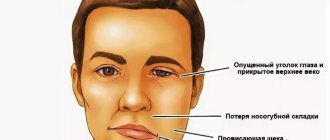
Symptoms of spontaneous massive cerebral hemorrhage
Ventricular (ventricular) hemorrhage in more than half of the cases ends in the death of the patient during the first two days. With a gradual outpouring of blood and a small amount, consciousness can be preserved.
Characteristic signs of the disease are:
- heavy sweating;
- trembling of the muscles of the whole body, as with chills;
- pale skin followed by redness;
- drop in body temperature with a sharp increase to 40 degrees;
- increased muscle tone in the form of a convulsive syndrome or a typical posture - the body is arched, the head is thrown back, and the forearms are turned inward.
Further progression of the disease is accompanied by increased pressure inside the skull and increased swelling of brain tissue. At the same time, the respiratory and vasomotor centers are compressed, which leads to disruption of the rhythm of heart contractions and a lack of oxygen supply to the body.
In the terminal stage, the depth of brain damage increases, convulsions, involuntary movements disappear, tendon reflexes are no longer detectable, muscle tone decreases, heartbeat and breathing stop.
Watch the video about cerebral hemorrhage and its consequences:
Types of hemorrhagic stroke
Hemorrhagic stroke is classified according to the nature of its occurrence (primary or secondary) and the location of the lesion.
| Primary | There is a sharp jump in pressure caused by a hypertensive crisis, causing the weakened walls of the brain vessels to rupture. It can be triggered by physical and nervous stress. |
| Secondary | Develops as a consequence of congenital or acquired vascular pathologies. The cause is rupture of an aneurysm (expansion of a section of an artery that is filled with blood), hemangiomas (a tumor of benign origin), etc. |
Based on localization, four types of stroke are identified:
| Subarachnoid | Blood flows between the pia mater and the arachnoid mater. This type of hemorrhagic stroke is caused by tumors, aneurysms, or head injuries. People aged 20 - 40 years are susceptible. It is registered even in infants with birth injuries. |
| Ventricular | Hemorrhage in one of the ventricles of the brain has extremely dangerous consequences. Occurs frequently, in almost 50% of cases. |
| Parenchymatous | Severe bleeding deep into the brain tissue, which is difficult to stop. Symptoms include loss of consciousness, even coma. |
| Subcortical | Hemorrhage in the temples or parietal area of the skull, under the cerebral cortex. Occurs in 15% of victims. The prerequisites are a prolonged increase in pressure. |
Interesting: Stroke in diabetes mellitus and its consequences
The severity of the consequences of a stroke depends on how extensive and deep the lesion has become.
Diagnostic methods
To make a diagnosis, typical symptoms are taken into account, as well as the presence of blood diseases, cerebral vessels, a previous stroke, and the use of medications. For newborns, the main signs are a complicated obstetric history and premature birth. Patients are examined in an inpatient setting. This may include:
- brain tomography (MRI, CT) is the most reliable method, you can determine the location of the hematoma and the degree of damage to the brain substance;
- Ultrasound – displacement of the structural parts of cerebral tissue;
- diagnostic puncture of the spinal cord, carried out to exclude ischemic stroke (blood is detected in the cerebrospinal fluid due to a hematoma);
- blood tests to determine platelets, coagulation profile, electrolytes, gas composition and acid-base status.
Treatment of patients with intraventricular hemorrhage and cerebral edema
The main condition determining the success of therapy is its earliest possible start.
At the stage of resuscitation, treatment is aimed at maintaining cardiac activity, restoring breathing and stabilizing basic blood parameters. If necessary, medications are administered for:
- stopping seizures (Diazepam, Phenorelaxan);
- blood pressure reduction (Magnesium sulfate);
- reducing swelling (Mannitol, glucose 40%, Lysine escinate, Lasix);
- stopping vomiting (Cerucal).
In the first six hours, the issue of carrying out the operation is decided. It can take place in the form of drainage of the cerebral ventricle or removal of contents during puncture. This treatment helps reduce tissue compression and intracranial hypertension. If emergency measures are successfully carried out, patients are prescribed therapy aimed at restoring brain tissue.
Forecast for adults and children
The prognosis of the disease is determined by the location and volume of hemorrhage. Small hematomas can resolve on their own or during treatment. Massive intraventricular hemorrhages, especially if the brain matter is affected, are extremely life-threatening. Even if it is possible to restore vital functions, a persistent neurological defect, as a rule, leads to lifelong disability.
The causes of death in patients are cerebral edema or recurrent hemorrhage. Severe complications of the disease include:
- blockage of the cerebrospinal fluid outflow tract with hydrocephalus (dropsy of the brain);
- destruction of the cortex, formation of a cyst, softening of the medulla;
- mental and motor dysfunction.
Preventive measures
It is possible to prevent cerebral hemorrhage in newborns by monitoring and treating a woman with a threat of miscarriage throughout the entire period of pregnancy, ensuring that she maintains complete physical and emotional rest. Also, if there are diseases that can cause premature birth, their complex therapy is required during pregnancy planning.
For adult patients, important conditions for the prevention of ventricular hemorrhage are:
- monitoring blood pressure, taking medications to normalize it;
- treatment of vascular diseases;
- avoiding smoking and alcohol abuse;
- use of drugs only on the recommendation of a specialist;
- timely diagnosis of decreased blood clotting and its correction.
And here is more information about stroke in young people.
Hemorrhage into the ventricles of the brain occurs in childhood and adulthood. In premature newborns it is caused by residual immature tissue, in later life the cause of hemorrhage is congenital defects in the structure of blood vessels, and in elderly patients low blood clotting ability, atherosclerosis, hypertension and diabetes come to the fore.
As a rule, the course of this pathology is severe, with increasing signs of cerebral edema and impairment of vital functions, which ends in the death of the patient. Treatment is carried out with medications and surgical removal of the hematoma.
Unfortunately, coma after a stroke is not uncommon. Doctors give a cautious prognosis, since it differs in the elderly and young, after hemorrhagic and ischemic. Recovery from a deep coma can occur in a few years, or in a couple of hours. How do you get out of a deep coma? How long can the maximum number of people stay in it without consequences?
A rather dangerous hemorrhagic stroke can develop even from heat stroke. The reasons for the extensive left hemisphere lie in stable arterial hypertension. Coma can happen instantly, with increasing symptoms. Treatment may not be effective.
Only timely recognition of subarachnoid hemorrhage will save lives. The symptoms of traumatic and non-traumatic cerebral hemorrhage are clearly defined. Diagnosis involves CT scanning, and treatment involves surgery. With a stroke, the consequences are worse.
Cerebral aneurysms occur, fortunately, rarely. Symptoms can be confused with other diseases, so MRI is performed as a diagnostic method. Rupture is one of the life-threatening consequences. Requires surgery and rehabilitation. The prognosis depends on the speed of visiting a doctor.
A real threat to life is a brainstem stroke. It can be hemorrhagic or ischemic. The symptoms resemble a heart attack and are also similar to other diseases. Treatment for a long-term, complete recovery after a brain stem stroke is almost impossible.
An intracerebral hematoma can occur both under the influence of external factors (traumatic) and for unexplained reasons (spontaneous). But the classification also takes into account size, location and other reasons. Treatment consists of surgical removal. The prognosis is not always favorable.
If a young person has a stroke, there is little chance of a full recovery. The causes of the pathology are often hereditary diseases and unhealthy lifestyle. Symptoms include loss of consciousness, convulsions and others. Why does ischemic stroke occur? What treatment is provided?
The reasons why a cerebellar stroke may occur are quite varied. Stroke can be ischemic, hemorrhagic, or stem. The treatment is long, recovery requires long-term rehabilitation. The consequences are problems with speech and movement.
Drug treatment for stroke is prescribed to relieve severe manifestations of the disease. In case of hemorrhagic or ischemic brain damage, they will also help prevent the progression and increase of symptoms.
Treatment of hemorrhagic stroke and recovery after it
Hemorrhagic stroke is characterized by a predominance of mortality and disability in victims after the stroke. Only isolated cases can be treated; with great difficulty it is possible to return a person to a full life. Minimizing the consequences of a stroke is carried out in two directions - medical and social.
It is better for patients to undergo treatment, recovery and rehabilitation after a hemorrhagic stroke in neurological clinics; home care will require a lot of effort and time from relatives.
Drug therapy
Intensive therapy after a hemorrhagic stroke comes down to correction of breathing and hemodynamics.
Subsequent treatment of the patient involves restoring blood circulation to the brain and normalizing blood pressure.
Therefore, local drugs that stimulate metabolic processes are used. Antibiotics are also prescribed to prevent the development of pneumonia and pulmonary edema.
Operation
During surgery, blood clots are removed, but care is taken not to damage brain tissue.
Surgery is performed in no more than 25% of cases when the hematoma is localized close to the surface of the skull and additional damage to brain tissue is not expected. That is, there will be no additional damage to health.
Open surgery is used for life-saving reasons for patients in serious condition.
Less traumatic punctures are usually used. The hematoma is aspirated through the burr hole of the skull.
Modern electromagnetic, ultrasound, and CT systems help to accurately get to the location.
Rehabilitation of patients
Rehabilitation of patients after a hemorrhagic stroke is a long, labor-intensive process that requires patience, moral and physical strength and can last for years. Much depends on the age, condition, mood of the victim and the efforts of his loved ones.
If the hemorrhage was local, not extensive, and assistance was provided on time and correctly, there is a chance of a 100% return to health. In addition to medications, the complex of rehabilitation measures includes:
- physiotherapy;
- acupuncture;
- exercise therapy;
- visiting the swimming pool;
- massage;
- vitamin therapy, etc.
The ability to speak coherently when damaged as a result of hemorrhagic hemorrhage is lost completely or partially. To resume communication skills, you will need the help of a speech therapist and psychotherapist.
This is required due to the depressed state from the blow suffered.
Much attention is paid to memory rehabilitation. Therapeutic exercise helps restore motor activity.
It is necessary to adhere to a healthy diet. Alcohol, smoking, stress, and serious physical activity are excluded.
Breakthrough of blood into the ventricles of the brain
Intraventricular hemorrhage is a subtype of acute cerebrovascular accident (stroke). Most often it occurs in people with arterial hypertension, whose age is from 45 to 60 years. Hemorrhage into the ventricles of the brain can also occur in a young person suffering from cocaine addiction. The clinical picture develops acutely and suddenly. Hemorrhagic stroke is usually preceded by physical stress or emotional stress.
Hypertension or persistent arterial hypertension is the most common cause of hemorrhage in the ventricles of the brain. People suffering from atherosclerosis, blood diseases, and inflammation of the blood vessels in the brain are also susceptible to stroke.
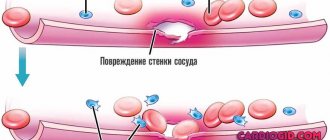
Hemorrhage (blood leakage outside the vessels) is based on functional and organic changes in brain circulation. When blood pressure is constantly elevated or a hypertensive crisis occurs (a sudden and strong increase in blood pressure to 200/100), disorders associated with vascular tone occur. The walls of blood vessels are disorganized: penetration for solid elements of blood and plasma increases. Diapedesis occurs - the formation of formed elements outside the arteries.
The pathology is complicated by the fact that, as a rule, not just one vessel is damaged, but the entire brain network, which is why massive focal hemorrhages in the ventricles occur. Here a vicious circle is activated: a protective mechanism is triggered, in which the vessels dilate and lose their ability to spasm. The dilation of the arteries further enhances the permeability of plasma and red blood cells, which increases the amount of blood released.
In addition, when diapedetic hemorrhage occurs, blood clotting mechanisms are disrupted. In a normal wound, platelets and coagulation mechanisms are automatically sent to the site of bleeding, where they “patch” the wound. However, with hemorrhage into the ventricles, this process is switched off.
Symptoms and consequences
The clinical picture begins with a gradual impairment of consciousness: from a state of stunning to coma. The latter develops when blood has filled all the ventricles. Impaired consciousness is proportional to the filling of the ventricles with blood. Body temperature rises abruptly. At first it can rise to 40 C, suddenly drop to 37 and rise again, but to 42 C.
The second option for the onset of hemorrhage in the ventricles is the appearance of convulsions in the extremities, which occur spontaneously. In this case, the head is thrown back, the arms are bent, and the fingers are clenched.
The phenomena of cerebral edema are increasing. The pathology clinic is always the same for all patients. Edema is formed due to the presence of blood in the brain tissue, which increases intracranial pressure. This is manifested by a bursting headache, nausea and vomiting. The swelling provokes a displacement of the structures of the brain stem and brain, a dislocation syndrome occurs: breathing and heartbeat are upset, unconditioned reflexes are inhibited, the pupil does not respond to light.
Neurological symptoms occur due to damage and blood saturation of the medulla. Thus, the clinical picture shows hemiparesis (loss of muscle strength) on the opposite side. If all the ventricles are filled, muscle strength is weakened in all limbs.
- redness of the facial skin;
- heavy sweating;
- blue color of peripheral areas: fingers and toes;
- the patient is depressed, he has a fear of death;
- disorientation.
The consequences of a stroke are unfavorable: in most cases, patients fall into a coma, and then death occurs.
First signs and symptoms
The first signs and symptoms of a hemorrhagic stroke are a severe headache. It occurs unexpectedly, immediately after rupture of blood vessels, from compression of the brain space, which is filled with blood. Along with this, swelling increases, which is called dropsy or hydrocephalus.
The intracranial space is filled with fluid; it cannot circulate through the spinal canal. Therefore, victims often complain that their head seems to be bursting from the inside.
As a result of edema, coma begins, tissue necrosis occurs, and then death follows. The disease often progresses rapidly and the outcome becomes obvious within two to three hours.
It is very important to recognize the symptoms of a hemorrhagic stroke and provide emergency assistance to the patient.
Diagnosis and treatment
Computed tomography can determine the location of the hemorrhage. In addition, the method detects a hematoma in the brain and its volume. For chronic hemorrhages, magnetic resonance imaging is used. A spinal tap is also performed. Cerebrospinal fluid reflects changes in the cavities of the ventricles. During hemorrhage, plasma and formed elements are found in the fluid.
Resuscitation treatment is aimed at maintaining the vital functions of breathing and heartbeat. The activities are also aimed at restoring brain function and eliminating symptoms. The main points of resuscitation actions:
- Elimination of cerebral edema with diuretics.
- Artificial maintenance of respiration using oxygen therapy.
- Anticonvulsant therapy with sibazon.
- Improving blood clotting: aminocaproic acid.
- Correction of water-salt balance and acid-base state by administering intravenous saline solutions.
Prognosis, possible complications
After medical care is provided, there is no guarantee that everything will be fine. Much depends on the capabilities of the body. However, medicine has long determined the prognosis for cerebral hemorrhage and the consequences that can occur even years later.
Forecast
Statistics show that after a hemorrhage in parts of the brain, only 10% of people can return to normal life. Moreover, the majority require regular assistance from doctors and loved ones, and 25% remain permanently disabled.
If the patient can swallow independently and his muscles work, then the chance of saving life remains quite high. In other cases, it is very difficult to save a person. Much depends on the speed of medical care.
The sooner a patient gets to the hospital, the more likely he is to survive.
Complications
The problem for people who have suffered a hemorrhage is the fear of the consequences. Severe complications can develop at any time, which can lead to death. Moreover, the timing of their appearance is unknown. Perhaps they will not appear at all, will appear in the first days, or will make themselves felt after a few years. What can be the risk of such bleeding for patients:
- Blood entering the ventricular system;
- Breathing problems;
- Increased cerebral edema;
- Malfunctions of the circulatory system;
- Paralysis of the entire body or individual limbs;
- Lack of muscle sensitivity;
- Occlusive hydrocephalus;
- Speech, hearing and vision impairments;
- Congestive pneumonia;
- Urinary tract infections;
- Arrhythmia, heart attack;
- Sepsis;
- Blood clots in the veins of the legs;
- Cell death when their nutrition is blocked by the hematoma;
- Development of pulmonary embolism;
- Multiple organ failure from blood loss;
- Bedsores;
- Mental disorders.
The most dangerous complications are problems with the brain and infectious and inflammatory processes. They are the most common cause of death in patients who have suffered hemorrhage.
After treatment, a person requires high-quality care and maximum comfort, both physically and psychologically. Without this, rehabilitation is impossible, and the risk of complications is enormous.
Symptoms and causes of intracerebral hemorrhage
Intracerebral non-traumatic (spontaneous) hemorrhage is accompanied by the development of symptoms of acute cerebrovascular accident, which have a similar clinical picture with signs of focal brain damage (GM).
The clinical picture directly depends on the volume of blood shed and the location of the damage in the brain. Hemorrhagic hemorrhage into the brain parenchyma is characterized by the appearance of general cerebral symptoms: headaches, vomiting, nausea, sudden depression or loss of consciousness that persists for more than a day.
The clinical picture of parenchymal hemorrhage is caused by a dysfunction of the cerebral hemorrhage of vascular origin, which occurs when arteries rupture, which have undergone pathological changes against the background of high blood pressure (BP) or cerebral amyloid angiopathy. Damage to the walls of blood vessels causes hemorrhage into the cranial cavity and damage to the brain parenchyma with blood and its decay products. And this, in turn, causes swelling of the brain, compression and displacement of intracerebral structures.
In the human body, blood flows through vessels. Normally, the vascular wall is very elastic, which allows it to withstand severe loads. Over time, the walls of blood vessels become thinner and become so fragile that even habitual loads can cause damage (rupture).
The main cause of hemorrhagic strokes is the rupture of blood vessels due to exceeding their safety margin against the background of increased pressure on the walls. Let's look at what causes of brain bleeding are considered the most common. This group includes:
- chronic untreated hypertension
- GM injuries
- neoplasms in the brain
- cerebral vascular aneurysm
- diseases accompanied by increased bleeding
- long-term use of blood thinners
- increased physical activity
The formed hematoma puts pressure on the surrounding tissues of the brain, which leads to disruption of trophic nutrition of the damaged area and causes the development of gross motor, speech and visual disorders. Due to the fact that a vessel rupture can occur in any part of the brain, they are usually classified according to the area of localization.
What are the manifestations?
Symptoms of cerebral hemorrhage depend on the location of the vascular accident. Against the background of general manifestations, signs characteristic of a specific affected area develop. Based on them, we can guess which part of the brain is affected.
The main manifestations can be divided into groups:
- General cerebral symptoms. The reasons for its occurrence are cerebral edema and increased pressure in the cranial cavity. The occurrence of the latter is possible due to a violation of the outflow of cerebrospinal fluid (a consequence of hemorrhage into the ventricles), improper functioning of the blood-brain barrier with high blood pressure, and head trauma. Brain edema also occurs when its structures are compressed by an increasing hematoma or due to dislocation.
- Meningeal symptoms (stiff neck, Kernig's sign). This clinic develops if bleeding in the cranial cavity occurs in the space between the meninges.
Meningeal syndrome is a set of symptoms caused by irritation of the meninges
- Focal symptoms. Directly related to the localization of the vascular accident. Damage to the nerve centers responsible for controlling certain functions manifests itself in different ways: paralysis, numbness, visual and speech impairment.
Extensive intracerebral hemorrhage is usually accompanied by the development of edema, displacement of brain structures, and their compression, which is usually manifested by general symptoms (vomiting, headache, convulsions, coma), as well as signs of irritation of the meninges. Focal symptoms begin to come to the fore after the swelling begins to subside, or when certain nerve centers are involved in the process and their functions are impaired.
Signs indicating increased intracranial pressure
These include a group of general cerebral symptoms, which in one way or another accompanies any pathological processes in the cranial cavity, be it bleeding, inflammation, injury or exposure to toxic substances. The reasons for increased intracranial pressure are as follows:
- inflammation, one of the characteristic manifestations of which is swelling;
- impaired circulation of cerebrospinal fluid (hemorrhage into the ventricles with the development of hemotamponade of the latter) or circulatory disorders (hypervolemia);
- change in the normal arrangement of brain structures (trauma; compression by a hematoma, resulting in swelling).
Epidural hematoma manifests itself as hypertensive-dislocation syndrome
The cranial cavity is limited in volume, therefore the appearance of additional formations (tumor, and in the context of this topic - hematoma), an increase in brain structures in size due to edema is accompanied by an increase in intracranial pressure. The signs of this condition are as follows:
- Expanding headache.
- Nausea and vomiting.
- Convulsive syndrome.
- Visual impairment due to swelling of the optic discs.
- Depression of consciousness (stupor, stupor, coma).
Brain swelling leads to compression of its structures in the natural canals of the skull. Thus, the brainstem is pinched in the foramen magnum, which is accompanied by disruption of the functioning of the vital centers of the medulla oblongata and can cause death. With dislocation and compression of brain structures, focal symptoms are added to the general symptoms, since certain nerve centers are affected. Over time, these manifestations begin to predominate, and when the swelling decreases, they come to the fore.
Signs of intracranial hemorrhage are caused by increased intracranial pressure, irritation of the membranes, as well as damage to specific nerve centers.
Features of the clinical picture of hemorrhage with damage to certain brain structures
The hemispheres of the brain have different specializations
When the left hemisphere suffers, movement and sensitivity disorders on the right, speech disorders, and memory problems become frequent manifestations. The right hemisphere is responsible for the perception of non-verbal information, imaginative thinking, and the ability to perform several tasks simultaneously. When hemorrhaging in this area, in addition to paralysis and sensitivity disorders, mental disorders (aggression, anxiety, depression) occur.
Bleeding into the ventricles is dangerous due to the possibility of hemotamponade (blockage) and disruption of the outflow of cerebrospinal fluid. This situation leads to increased intracranial pressure and serious consequences (compression of vital centers, coma, death). No less serious disorders occur when the brain stem is damaged, since this is where the respiratory and vasomotor centers are located. Cerebral hemorrhage with damage to the cerebellum is accompanied by impaired coordination of movements, the occipital lobe - visual disturbances, and the frontal lobe - convulsive syndrome.
Clinical picture
The severity of symptoms of hemorrhage in the brain depends on:
- localization
- volume of blood shed
Intracerebral hemorrhage is characterized by an acute onset. The clinical picture directly depends on the location of the hemorrhage.
Neurological symptoms appear unexpectedly and are characterized by increasing symptoms.
The occurrence of bleeding is indicated by sharp, sudden occurrences of:
- headache,
- nausea, vomiting,
- loss of consciousness and partial or generalized convulsions.
Extensive hemorrhages in the hemispheres are characterized by the appearance of hemiparesis, and with damage to the posterior fossa, the appearance of symptoms of damage to the brainstem or cerebellum, manifested by gaze paresis, ophthalmoplegia, stertorous breathing, pinpoint pupils. With transmural hemorrhage, the development of a precomatose state and coma is possible. Such hemorrhages most often end in death . In those who survive, as the escaping blood is reabsorbed, there is a gradual return of consciousness and regression of the neurological deficit.
Intracerebral bleeding in infants
The birth of a baby is a responsible and complex process in all respects, which is completely unpredictable. Sometimes the birth of a baby is very difficult and is accompanied by the development of birth injuries to the central nervous system.
Why do brain hemorrhages occur in infants?
Intracerebral hemorrhage occurs when the wall of a blood vessel in the brain ruptures. This bleeding in infants can be caused by prolonged oxygen deprivation or damage to the skull during childbirth.
Causes of hemorrhage in newborns:
- discrepancy between the size of the birth canal and the baby's head
- rapid or protracted labor
- postmaturity or prematurity of the fetus
- incorrect intervention by the obstetrician
- pregnancy complicated by hypoxia or infection
Types and symptoms of cerebral hemorrhages in newborns
Symptoms of hemorrhage in newborns, as in adults, depend on the area of localization. Depending on the zone of rupture, cerebral bleeding is divided into:
- epidural hemorrhages in newborns: occur when the blood vessels located between the dura mater and the bones of the skull are damaged; accompanied by dilation of the pupil on the affected side, slow heart rate, decreased blood pressure, suffocation, disturbance of breathing rhythm, convulsions
- subdural hemorrhage: observed when the vessels located between the dura and pia mater are damaged; most often occurs during rapid or protracted labor; the development of neurological disorders or a significant increase in bilirubin in the child’s blood is characteristic
- subarachnoid hemorrhage: the most common type of brain bleed in infants; occurs in premature babies when the vessels located between the substance of the brain and the arachnoid membrane rupture; accompanied by inflammation of the meninges caused by the breakdown products of spilled blood
Symptoms
Signs of a cerebral hemorrhage are directly related to the location where the blood enters. So, the symptoms of a hematoma in the frontal part of the organ are:
- decreased mental abilities;
- impaired speech function - the patient’s speech is unintelligible;
- a person's inability to maintain balance.
An outpouring of blood in the temporal lobe is characterized by:
- decreased visual acuity or absence thereof in one of the visual fields;
- a person does not understand what is said to him, although he hears everything perfectly;
- attacks of convulsions of the upper and lower extremities, less often - of the whole body.
Hemorrhage in the parietal zone entails loss of sensitivity on one half of the body. The effusion of blood into the occipital region causes decreased visual function or blindness.
The formation of a hematoma between the brain and skull is manifested by:
- migraines that constantly torment the patient;
- increased sensitivity of the eyes to light;
- intoxication of the body;
- fainting.
If blood enters the cerebellum, characteristic symptoms will be observed:
- difficulty maintaining balance;
- muscle weakness;
- uncharacteristic movements of the pupils, from one side to the other, and very quickly;
- difficulty breathing;
- convulsions;
- loss of consciousness;
- redness of the skin of the entire body.
In the case of accumulation of blood in the ventricles of the brain, external signs characteristic of cerebellar hemorrhage will be observed, but they will be supplemented by an internal disruption of the supply of nutrients and oxygen to the brain, because the accumulated blood blocks the channel through which cerebrospinal fluid enters the brain.
Symptoms of vascular rupture in newborns:
- disturbance of the sucking reflex;
- the whites of the eyes take on a red color;
- the skull, compared to the size of the baby’s body, is greatly enlarged.
Signs of intracranial bleeding tend to increase in intensity, so at the slightest change in the patient’s behavior or consciousness, you should immediately call an ambulance.
Diagnosis and treatment of cerebral hemorrhage
Diagnostics
To accurately diagnose cerebral hemorrhage, it is recommended to use CT or MRI results. If it is not possible to conduct neuroimaging, diagnosis is carried out on the basis of a thorough study of the clinical picture, analysis of the composition of the cerebrospinal fluid and the results of X-ray examination and echoencephaloscopy.
In addition to the fact that medical care for cerebral hemorrhage must be timely, there is a standard of specialized care that allows you to quickly relieve the main symptoms and minimize all negative consequences. The timeliness of treatment is the main factor determining the prognosis of the disease. Differentiated complex therapy, taking into account the causes and nature of hemorrhage will allow you to select the most effective approach to treatment. Of particular importance among all therapeutic measures is the maintenance of vital functions of the body, especially when the lesion is localized in the brainstem trunk. This will ensure the most efficient use of time. Equally important is the timely and rapid hospitalization of the patient in a medical institution.
When treating cerebral hemorrhage, conservative therapy is aimed at:
- reducing and maintaining blood pressure at the required level
- preventing the development and reducing the manifestation of cerebral edema
- stop bleeding
- strengthening and reducing the permeability of vascular walls
In what cases is neurosurgical treatment indicated?
Surgical intervention for hemorrhage in the brain is advisable in all cases . This is primarily due to the fact that often pathological processes develop against the background of changes to which the shed blood undergoes.
Indications for surgical treatment are:
- localization of hemorrhage in an area of the brain accessible for surgery
- rupture of a vessel aneurysm, especially if there is an increase in focal symptoms
Price for treatment and rehabilitation after intracerebral hemorrhage at the Yusupov Hospital
ICH is a serious disease with a large number of complications, therefore, after undergoing basic treatment, the patient is referred to additional restorative procedures, the prices for which are as follows:
- medical consultation from 3600 rubles;
- massage of one anatomical area from 2200 rubles for 15 minutes;
- manual massage for up to 45 minutes costs 5,500 rubles;
- speech therapy correction - 3410 rubles.
Clients of the clinic are provided with a comprehensive program of procedures, which is estimated at 14 thousand rubles per day. It allows you to restore lost skills as much as possible in a short period of time.
Hemorrhage into the ventricles (cavities) of the brain occurs with high blood pressure, low coagulation activity, alcoholism and nicotine addiction. In premature newborns, the cause of this disease is the remains of embryonic tissue. The course of hemorrhage is most often severe; if diagnosed untimely and without treatment, it ends in death due to cerebral edema.
Read in this article
Consequences and prognosis
Of course, the life of a patient after intracerebral bleeding will be strikingly different from the one he led before the disease. Focal symptoms will disappear as the hematoma resolves. The prognosis of the disease primarily depends on the location of the hemorrhage, timely treatment and its correctness.
The attitude of the patient himself plays an important role in the outcome of the disease. Despite the fact that they have to re-learn to talk, walk and eat, thanks to a positive attitude, many patients managed to return to a full life after extensive hemorrhages in the brain. And in some cases, on the contrary, even a minor cerebral hemorrhage became the cause of disability for a pessimistic patient.