Morgagni-Adams-Stokes syndrome (MAS syndrome) is a syncope that occurs when there is a sudden disturbance of the heart rhythm, and which entails cerebral ischemia and a sharp decrease in cardiac output.
Morgagni syndrome occurs due to cerebral ischemia, which occurs when cardiac output is sharply reduced. This occurs when the heart rhythm or heart rate is abnormal.
Often, Morgagni Adams Stokes attacks are caused by atrioventricular block. An attack occurs when a block occurs, followed by the development of sinus rhythm or supraventricular arrhythmia.
Development mechanism
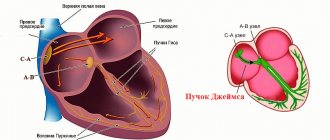
The essence of the pathological process is an acute blockade of nodes, bundle branches and other structures of the conduction system of the heart.
In 80% of cases, patients with even a single attack have AV block.
The atrioventricular node, responsible for conducting impulses to the ventricles, does not perform its function.
As a result of an acute disorder, the sinus node functions in vain. The ventricles do not contract. Compensatory activity begins in the chambers, each producing its own electrical impulse.
Chaotic movement leads to cerebral ischemia, blood circulation throughout the body is disrupted. This may result in the death of the patient. Depending on the intensity of the process.
Recovery is urgent, in a hospital setting. Mild episodes are treated on the spot with medication.
What are the possible consequences
Doctors do not always have to deal with only one complication. They develop right at the moment of the acute course of a Morgagni-Adams attack.
This presents particular difficulties when bringing a person out of a critical situation and significantly worsens the overall prognosis.
A critical decrease in blood flow in vital organs has fatal consequences. In terms of forecasting, the time factor is important. With prolonged cerebral hypoperfusion, clinical death occurs. This tragic complication occurs more often in older patients, but can also occur in younger patients.
The latter situation is explained by the fact that the brain is not adapted to such hemodynamic stress. In the elderly, on the contrary, chronic circulatory disorders occur in a variety of swimming pools.
Classification
Morgagni-Adams-Stokes syndrome is typified by the prevailing symptom, the type of rhythm disturbance.
- Bradyarrhythmia. Accompanied by a sharp drop in heart rate, less than 40 beats per minute. Critical levels give an unfavorable prognosis; urgent resuscitation is needed.
The patient almost immediately loses consciousness and remains in this state until correction; it is almost impossible to bring them out of this position. The brain does not receive enough nutrients and oxygen.
It is considered the most dangerous form, since it occurs suddenly and poses a particular threat to health and life.
- Tachysystole. Accompanied by acceleration of cardiac activity. Up to 150-200 beats per minute. It is not the heart rate that needs to be corrected, but the underlying pathological process. Before an acute condition develops, there are several minutes for the patient to react. Darkening in the eyes, shortness of breath, nausea, sweating and other “delights” of this situation accompany the person.
- Mixed variety. First tachycardia, then bradycardia. There are no fundamental differences in symptoms or clinical picture. Need urgent help.
All presented classifications are used after the fact to determine the etiology (root cause) of the process and develop treatment options.
At the first stage, emergency correction of the condition is needed. Only then can a diagnosis be prescribed. It’s better to go to the hospital in case the attack repeats.
How to make the correct diagnosis?
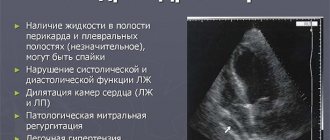
In the diagnosis of MAS syndrome, the main importance is given to electrocardiographic techniques - ECG at rest, 24-hour monitoring. To clarify the nature of the heart pathology, ultrasound examination and coronary angiography may be prescribed. Auscultation is of no small importance, when the doctor can listen to peculiar noises, intensification of the first tone, the so-called three-member rhythm, etc., but all auscultation signs must be correlated with electrocardiographic data.
Since Morgagni-Adams-Stokes syndrome is a consequence of various types of conduction disorders, it does not have electrocardiographic diagnostic criteria as such, and the phenomena on the ECG are associated with the type of arrhythmia that is provoked in a particular patient.
In case of conduction disturbance from the atrial node, the ECG evaluates, first of all, the duration of the PQ interval, which reflects the time of passage of the impulse through the conduction system from the sinus node to the ventricles of the heart.
With the first degree of blockade, this interval exceeds 0.2 seconds; with the second degree, the interval gradually lengthens or exceeds the norm in all cardiac complexes, while QRST periodically falls out, which indicates that the next impulse simply did not reach the ventricular myocardium. In the third, most severe degree of blockade, the atria and ventricles contract on their own, the number of ventricular complexes does not correspond to the P waves, that is, impulses from the sinus node do not reach their end point in the conductive fibers of the ventricles.
variety of arrhythmias causing MAS syndrome
Tachycardia and bradycardia are established based on counting the number of heart contractions, and ventricular fibrillation is accompanied by a complete absence of normal waves, intervals and ventricular complex on the ECG.
Causes
Development factors are multiple. But they almost always have a cardiac origin.
- Severe tachycardia of paroxysmal type. Manifested by a heart rate of 180 or more. The higher it is, the greater the likelihood of an attack of MES. Urgent medical attention is required.
- The reverse process is bradycardia. A drop in contraction frequency to a level of 50 or less ends with a violation of contractility and a damping of the intensity of bioelectric impulse generation. It is possible that intra-atrial conduction may slow down as a possible deviation from the norm.
- Ventricular fibrillation. Generation of its own signal by chambers (ventricles). An abnormal source of activity occurs outside the sinus node. Usually this is the result of some organic pathology. Less often functional. An extremely life-threatening condition that can result in cardiac arrest even before the formation of a Morgagni-Adams-Stokes attack or as a logical addition to it.
- Total atrioventricular block (AV). Accompanied by the impossibility of signal movement from the sinus cluster to other structures.
- Previous heart attack, myocarditis and other conditions leading to the death of active heart tissues and their severe scarring (cardiosclerosis).
- Disruption of the central nervous system as a result of brain tumors, infectious processes and other conditions.
The reasons are assessed in the system. The exclusion is being carried out gradually. Primary phenomena are identified relatively simply, within the framework of minimal diagnostics using ECG, echocardiography and daily monitoring.
Treatment
Treatment consists of resorption and dehydration therapy (see), which eliminates or mitigates the symptoms of hypothalamic-pituitary pathology. For ovarian-menstrual cycle disorders and infertility, gonadotropins - FSH and LH - are prescribed. Doses are selected individually under the control of functional tests and diagnostics (on average, 75-150 units of FSH for 7-10 days before the appearance of signs of ovulation, and then 3000 units of LH for 3 days). Clomiphene citrate can be used.
Forecast
favorable for life. As a result of treatment, body weight is reduced, headaches and dizziness are reduced, menstruation is restored and pregnancy may occur.
Prevention
is to prevent infectious diseases, intoxications, and obesity.
Bibliography:
Bukhman A.I. X-ray diagnostics in endocrinology, p. 89, M., 1974; Latash L.P. Hypothalamus, adaptive activity and electroencephalogram, M., 1968; Makarchenko A.F. et al. Physiology and pathology of the transitional period of women, Kyiv, 1967; Suprun A.V. and Kagan I.E. X-ray picture of the skull bones in women with pathological menopause and dysregulation of intraocular pressure, Ophthalm, journal, No. 5, p. 353, 1975; Calame A. Le syndrome de Morgagni, Morel, P., 1951; H ens with h enD. Morgagni's Syndrom, Jena, 1937, bibliogr.; Moore S h. Hyperostosis cranii, Springfield, 1955; Morgagni GB De sedibus et causis morborum per anatomen indagatis libri quinque, v. 1-2, Venetiis, 1761; S i 1 in - ii ov aM £ 1 kova E. a B 1 azek O. Endokraniosa, Praha, 1958.
3. L. Lemeneva; Yu. G. Elashov (rent.).
Symptoms
Manifestations of Morgagni-Adams-Stokes syndrome are specific. The clinical picture develops according to the same pattern with minor differences.
Deploying the full list of features takes 1 to 3 minutes on average. Sometimes seconds count. All manifestations can be divided into preceding and accompanying ones.
Previous signs
- Dyspnea. Not associated with physical activity. The patient can sit peacefully in a chair or stand in line. Accompanied by an increase in the number of movements, tachypnea is caused by a sharp drop in the intensity of gas exchange. This is a compensatory mechanism aimed at restoring oxygen concentration in the blood.
- Darkening in the eyes. Prevents the onset of fainting. In addition to the visual impairment itself, there is a painful tinnitus, all surrounding sounds are irritating and painful. Weakness, drowsiness. The patient cannot stand on his feet, the muscles lose tone.
- Dizziness. Vertigo leads to the inability to navigate in space. The world is going round and round. If you do not sit down, you may fall and get injured.
- Severe bursting pain in the chest. It felt like sewing up a heavy stone. This is the result of a rhythm disturbance in cardiac structures. Specific sign.
- Acute cephalalgia. Pain in the eyes, forehead, crown. Can squeeze, pull, knock.
Next comes the attack of MES (MAS): accompanied by cardiac symptoms, but the patient no longer feels anything. After 30-60 seconds, loss of consciousness occurs. Next, objective moments are recorded.
Associated symptoms
- Pale skin all over the body. The result of narrowing of peripheral vessels, insufficient blood circulation at a generalized level. The color of the mucous membranes of the gums also changes.
- Cyanosis of the nasolabial triangle. The area around the mouth is framed by a bluish ring. The shade is typical for the corners of the lips.
- Consciousness is consistently absent. Deep fainting occurs. It will not be possible to bring the patient out of such a state either by calling out or using physical force. Ammonia will also have no effect. When providing first aid, this must be taken into account and not waste time on useless manipulations.
- Breathing becomes shallow. It is impossible to detect it without special tools. The chest hardly moves.
- When measuring vital signs, a drop in blood pressure to critical levels is detected. This is an unstable level. Then comes growth. Such “swings” are the result of the body’s convulsive attempts to restore its own state. It is necessary to bring blood pressure back to normal to prevent it from getting worse.
- No visible pulse. It cannot be felt or is detected with great difficulty. An assessment of the condition using instrumental methods is required. Stopping cardiac activity is the basis for urgent resuscitation measures.
- Cramps. The muscles of the arms and legs move. These are spontaneous contractions, an alarming symptom. It speaks of the transition of the condition to a more severe phase.
- Emptying the bladder and bowels. The same. The unequal system suffers.
Without qualified correction, the patient's death may occur. Only a doctor can prevent such an outcome. All possible assistance in normalization is required from others.
Causes of Morgagni-Adams-Stokes attack, correct actions of relatives and medical staff
A Morgagni-Adams-Stokes attack (MAS syndrome) develops when there is a sudden disturbance in the heart rhythm. This leads to a drop in blood output and a cessation of blood flow to the brain. A few seconds after the heart stops, the patient loses consciousness, there is no breathing and convulsions appear; a prolonged attack can be fatal.
Causes of development of Morgagni-Adams-Stokes syndrome
MAS syndrome occurs when there is no signal from the sinus node, disruption of its conduction from the atrium to the ventricles, or asynchronous contraction of the muscle fibers of the heart. The following pathological conditions can lead to this:
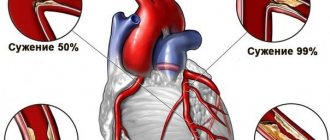
- Blockade of the atrioventricular pathway or transition from incomplete blockage to complete.
- An attack of tachycardia (more than 200 contractions per minute), flutter or ventricular fibrillation.
- Asystole or bradycardia below 30 beats in 60 seconds.
- Sinus node failure syndrome.
The mechanism of development of Morgagni-Adams-Stokes syndrome
Such disorders occur against the background of ischemic disease, accumulation of amyloid protein in the myocardium, cardiosclerosis after inflammatory or degenerative processes in the myocardium, poisoning with cardiac glycosides, Cordarone, Lidocaine, beta blockers or calcium antagonists. An attack of MAS can also occur with autoimmune diseases and damage to the nervous system.
We recommend reading about increased heart rate with normal blood pressure. You will learn about the mechanisms of arrhythmia, the causes of rapid heart rate, symptoms, possible complications, diagnosis and treatment. And here is more information about the treatment of atrioventricular block.
Forms of the syndrome
Depending on the heart rate against which this pathology developed, the following clinical forms are identified:
- Tachycardia - occurs during an attack of excessive heart rate (more than 200/min) of ventricular or supraventricular origin, atrial fibrillation or flutter, Wolff-Parkinson-White syndrome.
- Oligosystolic (with a pulse up to 30/min) when the production of a signal in the sinus node stops, its propagation to the atria or from them to the ventricles.
- Mixed - alternating a rapid pulse with periods of stopping contractions.
Variants of a Morgagni-Adams-Stokes attack on an ECG
Symptoms of a Morgagni-Adams-Stokes attack
Provoking factors include stressful situations, especially sudden fear, a sharp surge of emotions, and a rapid change in body position. The first signals of impending fainting can be in the form of tinnitus, headache, blurred vision, increased sweating, nausea, and uncoordinated movements. After a few seconds the patient loses consciousness.
The clinical picture is dominated by the following symptoms:
- pale skin, then the tips of the fingers and lips turn blue;
- blood pressure drops;
- twitching of the muscles of the face or body is observed;
- breathing becomes shallow;
- the pulse is weak, soft, the rhythm is disturbed;
- There may be involuntary discharge of urine and feces.
After an attack, patients usually do not remember what happened. When cardiac activity is restored, the condition becomes satisfactory.
Variants of MAS attacks
Depending on the duration and patency of the cerebral vessels, attacks occur:
- reduced – a brief episode of dizziness, darkening of the eyes;
- without loss of consciousness - in the absence of pathology of the cardiac and cerebral vessels, manifested by lethargy and unsteadiness of gait, general weakness;
- rapid loss of consciousness - dilated pupils, cyanosis of the skin, bubbling breathing, lack of pulse and pressure, an attack can be fatal.
Features of the attack
Sudden loss of consciousness can occur with epilepsy, a hysterical attack, thrombosis of cerebral vessels, pulmonary hypertension, acute or transient disruption of the blood supply to the brain due to blockage or spasm of blood vessels, narrowing of the aorta, or a drop in blood sugar.
Distinctive signs of MAS syndrome:
- Lack of pupillary response due to cyanosis.
- A slow pulse with no response to phases of the respiratory cycle, physical activity, or a rapid pulse that does not change when pressing on the eyeballs.
- Cannon tone at the moment of coincidence of contraction of the atria and ventricles, independent venous waves in the neck.
Diagnosis of an attack of MAS
The cause of the development of MAS syndrome can be determined using ECG diagnostics. Depending on the type of rhythm disturbance, there is a blockade of the conduction pathways or asynchronous contractions of the atria and ventricles.
With a routine study, it is most often impossible to detect this syndrome, so Holter monitoring is indicated.
To confirm ischemic or dystrophic changes in the myocardium, coronary angiography or cardiac muscle biopsy is prescribed.
A short spontaneously terminated Morgagni-Adams-Stokes attack due to ventricular asystole in a patient with 3rd degree AV block
Treatment of Morgagni-Adams-Stokes attack
An important stage of treatment is the correct provision of emergency care in case of a sudden attack, since the patient’s life depends on it. After restoration of consciousness, drug and surgical treatment with the installation of a pacemaker is indicated.
Emergency assistance before the ambulance arrives from relatives
Resuscitation measures can be carried out by non-specialists. The following rules must be taken into account:
- Check the pulse in the carotid artery.
- If it is absent, hit the lower third of the sternum with your fist (the blow should be noticeable, but not excessive, usually the distance to the sternum is no more than 20 cm).
- Press rhythmically on the sternum, after 30 presses, take 2 breaths into the patient’s mouth.
To learn how to properly perform basic cardiopulmonary resuscitation, watch this video:
Actions of emergency medical personnel
To restore cardiac activity, the following measures are used:
- electrocardiostimulation;
- Adrenaline into the heart or trachea;
- Atropine sulfate subcutaneously;
- Izadrin tablet under the tongue, if ineffective intravenous Alupent and Ephedrine.
Treatment in hospital
After hospitalization, therapy with alpha-agonists and antiarrhythmic drugs continues. All medications are used under constant ECG monitoring. If it is difficult to achieve a normal rhythm and there is a risk of cardiac arrest, then such patients are recommended to install pacemakers that generate impulses constantly (with complete blockage of the conduction pathways) or on demand.
Prognosis for the patient
The course of the disease depends on the degree of myocardial damage.
In young patients, with timely diagnosis and treatment with antiarrhythmic drugs or after installation of an artificial pacemaker, the prognosis is favorable.
Against the background of widespread cardiosclerosis and concomitant impairment of the patency of cerebral vessels, the chances of a complete recovery even after surgical treatment are much lower.
We recommend reading about ventricular extrasystole. You will learn about the classification of PVCs, causes of development, symptoms, diagnosis and treatment. And here is more information about the treatment of ventricular tachycardia.
First aid algorithm
The main thing to do is call the emergency team. Until the doctor or paramedic arrives. Next, it is necessary to stabilize the victim’s condition. If possible.
What needs to be done and in what order?
- If a person is outdoors in the cold season, move him indoors or, as a last resort, lay something warm under his body.
- Loosen your collar or remove your body jewelry. Pressure on the carotid sinus in the neck will cause a reflex drop in blood pressure and heart rate. This is certain death in this situation.
- Open a window or window (in the room) to ensure normal ventilation. Restoration of gas exchange is required in all cases, this is important.
- Measure blood pressure and heart rate. These indicators must be reported to arriving doctors.
- Drugs are not given to an unconscious person.
- Turn your head to the side and release your tongue in case of vomiting.
- Heart rate is constantly monitored. In the absence of cardiac activity, direct massage is indicated. The palms are folded and rhythmically pressed on the chest 100-120 times per minute.
A rib fracture is not a reason to stop resuscitation efforts. If you have no experience in artificial respiration, it is better not to do it. There will be no point.
Upon arrival of the brigade, all activities cease. Briefly provide information about the victim and his condition. If necessary, you can accompany the person to the department.
Urgent Care
If an attack of MAS develops, the patient must urgently call an emergency cardiac care team. On the spot, those around the patient can carry out measures that are also used in case of cardiac arrest:
- A punch to the lower third of the sternum.
- Indirect cardiac massage.
- Artificial respiration (if breathing stops).
Before transporting the patient to the intensive care unit, emergency care is provided, which includes measures aimed at eliminating the symptoms of the underlying disease that provoked the attack. In case of cardiac arrest, the patient is given emergency electrical stimulation, and if it is impossible to perform it, intracardiac or endotracheal administration of a 0.1% solution of Adrenaline in 10 ml of physiological solution.
Next, the patient is injected with a solution of Atropine sulfate (subcutaneously) and given 0.005-0.01 g of Izadrina under the tongue. When the patient's condition improves, they begin transporting him to the hospital, repeating Izadrina as the heart rate decreases.
If the effect is insufficient, the patient is given a drip injection of 5 ml of 0.05% Orciprenaline sulfate (in 250 ml of a 5% glucose solution) or 0.5-1 ml of Ephedrine (in 150-250 ml of a 5% glucose solution). The infusion begins at a rate of 10 drops/minute, then the rate of administration is gradually increased until the required amount of heart rate appears.
In the hospital, emergency care is provided under constant ECG monitoring in the same way. The patient is injected with solutions of Atropine sulfate and Ephedrine subcutaneously 3-4 times a day and given 1-2 Izadrina tablets under the tongue every 4-6 hours. If drug therapy is ineffective, the patient is given transesophageal or other electrical stimulation.
What definitely should not be done
- Leave the patient lying in the cold. Hypothermia will lead to spasm of the coronary arteries, a profound deterioration of the condition. The patient needs to be moved indoors. This will also protect against frostbite; blood flow is already minimal, and tissue damage is possible.
- Giving drugs, especially putting them in the mouth by force. Possible asphyxia if inhaled.
- Intravenous administration and injections are prohibited. It is not known what caused the condition. Even if you have a medical education, you won’t be able to establish this right away.
Where to start therapy?
In order for MARS syndrome to manifest itself minimally or not at all, you need to choose an optimal daily routine, an appropriate load for your age and condition, alternating activities and rest. Many parents believe that a child with MARS needs to sharply limit exercise, which is fundamentally wrong. After consulting with a doctor, for the most part, you can not limit the baby’s movement at all. The heart develops correctly when it is given adequate stress. There is no need for restrictions in activity or excessive effort. If the baby expresses a desire to engage in any kind of sport, first consult with a cardiologist to see if the level of stress that sports activities will provide is possible for him. But ordinary daily activities - walking outside, cycling, running - are quite enough for proper development.
For a child with MARS syndrome, it is important to follow a daily routine, get enough sleep, eat properly, and receive all the nutrients and vitamins required by age. It is important to initially prepare yourself for long-term breastfeeding; this will help the baby get sick less and reduce the risk of heart complications at an early age to a minimum. In addition, it is necessary to introduce complementary foods into the child’s diet correctly and in a timely manner, and subsequently monitor the intake of sufficient amounts of protein foods and foods rich in calcium and magnesium.
Children who have neurological problems and are emotionally unstable benefit from working with a psychologist and sedative therapy. Physiotherapy - various baths, spa therapy, massages - also have a calming and restorative effect.
Such babies are monitored jointly by a pediatrician and a pediatric cardiologist. The timing of inspections is selected individually, depending on the type of MARS and the presence or absence of associated violations. Usually, for most children, non-drug measures or infrequent courses of cardiotrophic (supporting the proper functioning of the heart) drugs are sufficient.
Only isolated cases of MARS may require surgical correction. In such cases, the baby will be referred to a cardiac surgeon to decide on the volume and timing of the operation. There is no need to be afraid of this - open heart surgery is very rarely performed for MARS. Usually these are so-called endoscopic operations - an instrument is inserted into the heart cavity through small punctures or through large vessels and the defect is corrected. Usually, babies stay in the clinic for a short time and after discharge they lead the lifestyle of ordinary children.
Possible consequences of an attack
They depend on the type of pathological process, as well as the moment of starting first aid, qualified treatment in a hospital and recovery from the condition.
Typical complications:
- Cardiac arrest as a result of complete non-conduction of the sinoatrial node, His bundle, or total dysfunction of the sinus node. Asystole is the cause of death in the majority of cases. Moreover, recurrent attacks are associated with a high risk of death.
- Heart attack. As a result of stenosis of the coronary arteries and necrosis of active tissues.
- Stroke. Also a likely consequence. It is considered almost a classic of the genre. Accompanied by acute malnutrition of cerebral structures. Hence the death of nerve bundles. Even with the restoration of normal functioning, neurological deficits of varying degrees of severity remain.
- Pulmonary edema. As a result of insufficient outflow of blood from the small circle, its stagnation. Restoration is carried out urgently.
The result is at least severe disability for the patient. Death is also a likely outcome.
Doctors do not always have to deal with only one complication. They develop right at the moment of the acute course of a Morgagni-Adams attack.
This presents particular difficulties when bringing a person out of a critical situation and significantly worsens the overall prognosis.
Features of symptoms
With MAS syndrome, attacks occur suddenly and may be preceded by stress, severe nervous tension, fear, or excessive physical activity. A sudden change in body position, when the patient quickly gets up, can also contribute to the manifestation of heart pathology.
Usually, in the midst of complete health, a characteristic symptom complex of MAS appears, including cardiac disorders and brain dysfunction with loss of consciousness, convulsions, involuntary bowel movements and urine output.
The main symptom of the disease is loss of consciousness, but before it the patient feels some changes, which he can then talk about. Approaching fainting is indicated by darkening of the eyes, severe weakness, dizziness and noise in the head. Cold sticky sweat appears on the forehead, a feeling of nausea or lightheadedness appears, and there may be a feeling of palpitations or constriction in the chest.
20-30 seconds after the paroxysm of arrhythmia, the patient loses consciousness, and the signs of the disease are recorded by others:
- Lack of consciousness;
- The skin turns pale, cyanosis is possible;
- Breathing is shallow and may stop completely;
- Blood pressure drops;
- The pulse is threadlike and often cannot be felt at all;
- Convulsive muscle twitching is possible;
- Involuntary emptying of the bladder and rectum.
The disease can occur without loss of consciousness. This is typical for young patients in whom the vascular walls of the cerebral and coronary arteries are not damaged, and the tissues are relatively resistant to hypoxia. The syndrome is manifested by severe weakness, nausea, dizziness with preservation of consciousness.
Elderly patients with atherosclerosis of the cerebral arteries have a worse prognosis, and their attacks are more severe, with a rapid increase in symptoms and a high risk of clinical death, when there is no heartbeat and breathing, pulse and pressure are not detected, the pupils are dilated and do not respond to light.
Diagnostics
It is carried out in a hospital. But after first aid. The condition is too serious to delay.
The minimum program includes a visual assessment of the skin, mucous membranes, measurement of blood pressure, frequency of contractions of a muscle organ, and auscultation (listening to heart sounds).
Next comes first aid. It is possible to use Atropine or Epinephrine to restore adequate myocardial contraction, electrocardioversion, defibrillation to normalize the conductivity of structures.
Upon completion, already in a hospital setting, a group of activities is prescribed:
- Oral interview, history taking. What complaints, how long ago did they arise, whether there were attacks before, how severe, previous and current diseases of any profile, lifestyle, family history, operations in the past, etc.
- Auscultation (listening for a heartbeat).
- Repeated blood pressure and heart rate measurements.
- Daily monitoring. To assess heart rate and blood pressure over time, after the patient’s usual activity (as far as possible).
- Electrocardiography. Normally it shows no deviations. Changes are present in pathologies that can lead to MES syndrome.
- Echocardiography. To assess the organic state of tissues and structures.
- MRI if necessary.
- General blood test, biochemical, hormones.
The neurological status is examined as part of the identification of deficiency disorders.
Prevention of attacks and relapses
The use of preventive measures is possible for attacks that are caused by paroxysms of tachyarrhythmia or tachycardia. In this case, patients are prescribed various antiarrhythmic drugs.
It is also necessary to exclude factors that lead to an attack - sudden movements, sudden changes in body position, anxiety, nervous overload, emotional stress, intoxication.
In case of complete atrioventricular block, the main preventive method is the installation of a pacemaker.
Treatment methods
It is carried out under the supervision of a cardiologist. In the long term, drug therapy is ineffective, but it is used at the initial stage to ensure the stability of the patient’s condition.
The following drugs are prescribed:
- Antihypertensive drugs of various types. From ACE inhibitors to calcium antagonists and centrally acting agents. Depends on the main diagnosis and the degree of deviation of blood pressure from the standard.
- Antiarrhythmic. Amiodarone. Other drinks are strictly prohibited. Provocation of the syndrome is possible.
- Cardioprotectors. Restore normal metabolism in the tissues of cardiac structures. Mildronate.
- Cerebrovascular drugs. For adequate blood flow in the brain. Piracetam or Actovegin as the main ones.
A similar scheme is followed until the health status is normalized, heart rate and blood pressure are consistently adequate, and neurological symptoms are relieved.
Next, surgery is scheduled. The main way to eliminate the syndrome is implantation of a pacemaker. Morgagni-Adams-Stokes attacks stop developing as conduction is artificially normalized. Exceptions are extremely rare (no more than 5% of situations).
Clinical picture
The main wedge, symptoms in MS—hyperostosis of the internal plate of the frontal bone, obesity (of the hypothalamic type with uniform fat deposition) and hirsutism (see)—make up the classic Morgagni triad; disorders may be observed at the same time: emotional and mental (emotional instability, memory loss, sleep disorders, increased fatigue), autonomic and neurological (bulimia, polydipsia, ptosis, ocular convergence disorders, headaches, dizziness, sweating, trophic changes in the skin and mucous membranes of the genitals organs, increased blood pressure, sometimes epileptiform seizures) and neuroendocrine (disorders of carbohydrate metabolism, ovarian-menstrual function such as opso- and amenorrhea, infertility). The exchange of calcium and phosphorus is not impaired. The central mechanism of ovarian dysfunction is confirmed by the presence of changes in the ratio of the level of excretion of gonadotropins - follicle-stimulating hormone (FSH) and luteinizing hormone (LH) of the pituitary gland. With opsomenorrhea (see Menstrual cycle), the level of excretion of FSH and LH is reduced, but cyclic fluctuations in this level are noted. With prolonged amenorrhea, the excretion of both FSH and LH is sharply reduced and there are no pronounced fluctuations in the quantitative excretion of gonadotropins.
To identify the functions and state of the brain in M. s. electroencephalography is used (see), while in some patients the EEG in leads from the frontal and precentral parts of the brain is dominated by clearly expressed theta activity with a frequency of 5-7 oscillations per second; the reaction of depression of the basic rhythm to continuous light is weakened. Other patients have pronounced phenomena of irritation with a predominance of frequent activity in all leads from the cerebral cortex. In many patients, deviations are detected only under the influence of functions and loads. A certain relationship has been established between the symptoms of the disease and EEG data. With bulimia (see), polydipsia (see), trophic changes in the skin and mucous membranes, emotional and mental disorders, headaches, disturbances in the diencephalic region are detected on the EEG. With brainstem disorders - moderate ptosis (see), ocular convergence disorder (see) - and headaches, changes in the reticular formation of the midbrain predominate on the EEG. When the above symptoms are combined with increased blood pressure and impaired carbohydrate metabolism, the EEG shows disturbances in the meso- and diencephalic structures.
Expressiveness wedge. The picture, as a rule, is not related to age and duration of the disease, but depends on the function and activity of the pituitary gland.
Forecast
Depends on the quality of first aid, the moment of the start of emergency measures of a qualified plan.
Many factors need to be taken into account: age, general health, gender, history of illness, chances of undergoing radical treatment and implantation of a pacemaker, bad habits, family history and other points.
The ability to undergo surgery is associated with maximum survival. Almost 95%. Only 5% of patients have a worse prognosis, and not in absolute terms. It just requires additional correction. Stroke, heart attack, and other complications significantly worsen the outcome.
Questions of this nature should be addressed to your primary physician. Outsiders do not know the patient well enough, so they are unlikely to say anything right away. It is also impossible to take into account all the nuances on your own.
What if you need pills?
Sometimes there are situations when the doctor will recommend a course of certain medications. The main therapeutic effects are magnesium preparations. This trace element is a component of connective tissue and therefore improves its structure and heart function. The choice of magnesium preparations depends on the age of the patient. There are liquid and tablet forms. Particularly popular are “Magnerot” - in addition it also contains orotic acid, which promotes the absorption and more complete absorption of magnesium, “Magne B6” in the form of syrup or tablets, and “Potassium Orotate”. Usually 1-2 courses per year are recommended.
The second direction of therapy is cardiotrophic - nourishing the heart muscle. These are drugs that improve blood supply and nutrition to the tissue of the heart and other organs, affect metabolism in the body and are active antioxidants. Usually prescribed are “Elkar”, “Ubiquinone” or “Coenzyme Q10”, “Kudesan”, “Cyto-mac”. In addition to these drugs, some vitamins have a similar effect - PP, B2, B1, citric and succinic acids (the drug "Limontar"), biotin. They are prescribed as a multivitamin complex or each separately in courses of 10-14 days twice a year.
In case of infections, the baby is recommended to take preventive courses of antibiotic therapy to prevent heart complications such as endocarditis.
Regular examinations by an ENT specialist and a dentist are indicated to sanitize foci of chronic infection - carious teeth, tonsils, adenoids.
In the presence of arrhythmias, antiarrhythmic therapy is indicated, but it is selected individually in the hospital under the supervision of a physician.
Courses of sedatives are conducted that normalize the functioning of the nervous system, relieve anxiety, increased nervous excitability and treat neuroses.
Diagnosis
The diagnosis is made on the basis of anamnesis, typical manifestations of seizures, registration of asystole and other rhythm disturbances.
Differential diagnosis
most often carried out with epilepsy (see), less often with hysteria (see). With epilepsy, in contrast to M.—A.—S. there is an aura and tongue biting, epileptogenic bioelectrical activity is noted on the EEG, there are no changes on the ECG. During an epileptic seizure, the pulse is tense and rapid, the face is purple and bluish; during a seizure with M.—A.—S. s. the pulse is not detected or is sharply reduced, the face is initially deathly pale, then sharply cyanotic.
Cardiologist → Consultations
Hello! Unfortunately, it is not within our authority to give any recommendations for treatment; this can only be done by the doctor who prescribed you to take this medication.
The ECG was not interpreted correctly; there is no such electrocardiographic diagnosis. You need an in-person consultation with a cardiologist, where you will have the opportunity to evaluate your complaints.
Hello! Unfortunately, it is not within our authority to give a transcript of the tests - this is the business of your attending physician who sent you for diagnostics.
These symptoms are not normal, especially since they are quite dangerous in your situation. Perhaps it did not suit you and caused side effects. It's better not to take risks.
MAS is an attack of loss of consciousness accompanied by respiratory failure and convulsions due to acute hypoxia (oxygen starvation) of the brain.
This attack is associated with the occurrence of a blockade in the heart and a subsequent sharp decrease in the contractility of the myocardium (heart muscle).
The syndrome is named after the doctors who studied it: Morgagni, Adams and Stokes.
What happens in the heart during an attack of MAS?
Normally, impulses that promote normal contraction of the heart pass from the atria to the ventricles of the heart. When heart block occurs (AV - atrioventricular block), this impulse is interrupted and normal contraction of the heart is impossible.
Atrioventricular (AV) - heart block can be complete or incomplete.
What does it mean?
This means that with complete AV blockade, the flow of impulses from the atrium to the ventricle of the heart is blocked. The ventricles lose their ability to contract and cannot push blood out of the heart into the aorta (the largest vessel leaving the heart) in order to “saturate” the brain and other organs with blood. In turn, the brain begins to experience oxygen starvation and “turns off” in the form of a seizure with loss of consciousness.
What causes MAS?
Atrioventricular block (AV block) of the heart.
Transition from incomplete heart block to complete block.
At heart rate = 30 beats per minute.
At heart rate = 200 beats per minute or more.
Rhythm disturbances with a sharp decrease in the contractility of the heart (ventricular fibrillation and asystole (complete cardiac arrest)).
What triggers an attack of MAS during heart block?
Quick transition from a horizontal position to a vertical body position. Sudden rise from bed.
Mental overexcitation (stress, fear, anxiety, anticipation, etc.).
How does an attack of MAS manifest?
Clinical manifestations (symptoms and signs)
MAS attack
Dizziness.
Convulsions (start 1 minute after loss of consciousness).
Severe pallor of the skin.
The pupils dilate.
After providing appropriate assistance, the pumping (contractile) function of the heart is restored, blood enters the brain and the patient regains consciousness.
More often, after an attack, patients do not remember what happened to them and what events preceded the attack (amnesia).
In young people with good contractility of the heart and blood vessels “free” from atherosclerosis, seizures may be easier, starting with dizziness, increased heart rate up to 200 beats per minute and limited to temporary retardation.
In older people suffering from atherosclerosis of the vessels of the heart and brain, attacks develop quickly and are more severe.
Diagnosis of Morgagni–Adams–Stokes syndrome (MAS)
Diagnosing MAS has certain difficulties, because the clinical picture of MAS is identical to the picture of clinical death (it is not always possible to immediately determine that this condition is caused by AV heart block.
Sudden onset (in the midst of full health).
Dizziness.
Darkening of the eyes, tinnitus and loss of consciousness.
Convulsions (starting 1 minute after loss of consciousness).
Facial cyanosis (bluish tint of lips, nose, ears, fingers).
The pulse is sluggish or not palpable at all.
Blood pressure cannot be measured.
The pupils dilate.
Considering these manifestations and the rapid restoration of the contractile function of the heart during emergency care, and often the absence of atherosclerotic vascular damage, it may suggest that this patient has Morgagni–Adams–Stokes syndrome.
ECG (electrocardiogram)
During and immediately after an attack of MAS, giant negative T waves are recorded on the cardiogram; they indicate a recent attack with loss of consciousness and are a very characteristic sign of MAS.
Daily monitoring (Holter)
This is a method of recording an ECG during the day, which increases the chance of “catching” an incoming heart block, against the background of which an attack of loss of consciousness occurs.
Holter makes it possible to record data and determine the correctness of the diagnosis. Daily heart monitoring makes it possible to exclude brain diseases, which can also manifest as attacks of loss of consciousness up to several times a day (epilepsy) and to develop further treatment tactics.
Treatment of Morgagni–Adams–Stokes syndrome (MAS)
Treatment of MAS syndrome involves providing assistance during an attack and conducting therapy aimed at preventing the occurrence of new attacks.
A patient after an attack of MAS should be hospitalized in a specialized cardiology department to clarify the causes of these attacks and a more thorough examination of the heart in order to make the correct diagnosis and determine further treatment tactics.
Help with an attack of MAS
At the time of a seizure, the patient receives standard resuscitation measures (as in clinical death).
1. Mechanical defibrillation is performed - a “precordial” blow, this is a sharp blow with a fist to the lower third of the sternum (but in no case to the heart area!), in order to cause a reflex response of the heart and force it to contract.
2. If there is no effect, electrical defibrillation is performed (applying electrodes to the chest and delivering a “shot” with an electric current discharge) in order to “start” the heart and force it to work in the correct rhythm.
3. In case of respiratory arrest, mechanical ventilation (artificial pulmonary ventilation) is carried out, by blowing air “mouth to mouth” or using a special breathing apparatus.
4. If cardiac arrest occurs, a solution of adrenaline and atropine is administered intravenously.
5. Resuscitation measures continue until consciousness is fully restored or signs of biological death appear.
Drug therapy for MAS syndrome
Constant use of various antiarrhythmic drugs is prescribed to prevent relapses (repeated attacks) of MAS. But the diagnosis of Morgagni–Adams–Stokes syndrome itself implies only surgical treatment.
Surgical treatment of MAS
The presence of MAS syndrome in patients serves as a direct indication for implantation (installation) of an electrical pacemaker (PAC).
In case of complete heart block (AV block), constantly working pacemakers are implanted, which turn on “on demand”. Namely, at the moment when heart contractions begin to slow down, the pacemaker turns on and stimulates heart contractions.
Surgical destruction of additional pathways for conducting impulses (laser, chemicals) or mechanical destruction is the “destruction” of additional pathways for conducting electrical impulses in the heart.
Prognosis for MAS syndrome
With prolonged oxygen starvation, lasting more than 5 minutes, the nervous system and intellect suffer. The more frequent the attacks of MAS, the worse the prognosis. One of the attacks of MAS can result in the death of the patient. Timely diagnosis and surgical treatment of MAS significantly improves the quality of life of patients and the prognosis for survival.
All information on the site is provided for informational purposes only and cannot be taken as a guide to self-medication.
Treatment of diseases of the cardiovascular system requires consultation with a cardiologist, a thorough examination, prescription of appropriate treatment and subsequent monitoring of the therapy.
Course of the disease
Morgagni-Morel-Stewart syndrome can affect the body in different ways. This often depends on the degree of obesity. Pronounced has a great influence on life expectancy:
- heart activity is difficult;
- due to the accumulation of fat, the myocardium and pericardium arise;
- high aperture position;
- blood circulation is impaired, and in combination with atherosclerosis and hypertension, heart failure develops, which is the cause of disability;
- If a patient with the syndrome also has diabetes mellitus, then metabolic disorders begin, which leads not only to a decrease in performance, but also reduces life expectancy.
Features of the attack
Sudden loss of consciousness can occur with epilepsy, a hysterical attack, thrombosis of cerebral vessels, pulmonary hypertension, acute or transient disruption of the blood supply to the brain due to blockage or spasm of blood vessels, narrowing of the aorta, or a drop in blood sugar.
Distinctive signs of MAS syndrome:
- Lack of pupillary response due to cyanosis.
- A slow pulse with no response to phases of the respiratory cycle, physical activity, or a rapid pulse that does not change when pressing on the eyeballs.
- Cannon tone at the moment of coincidence of contraction of the atria and ventricles, independent venous waves in the neck.
Mechanism of action
During normal heart function, impulses travel from the atria to the ventricles. Arterial blockade is an interruption of this impulse. Due to this process, myocardial contraction does not occur.
The blockade is divided into several types:
- complete - in this case, the passage of impulses towards the ventricles completely stops. Oxygen does not enter the tissues and organs of the body, the brain. Gradually their work stops. This is why the patient loses consciousness. Help must be immediate.
- partial, when the impulse is interrupted irregularly.